Associated Factors
The condition is associated with the following factors:
- HPV Infection: Approximately 40%–60% of vulvar carcinomas are linked to HPV infection, with more than 50% being associated with HPV 16.
- Non-HPV-Related Factors: These include race, advanced age, smoking, vulvar lichen-related diseases or vulvar inflammation, and human immunodeficiency virus (HIV) infection.
Pathology
Macroscopic Features
Lesions typically appear as superficial ulcers or firm nodules and may be accompanied by infection, necrosis, or bleeding. The surrounding skin may show thickening or pigmentation changes.
Microscopic Features
Most squamous cell carcinomas display well-differentiated cells, with keratin pearls and intercellular bridges observed. Lesions in the vestibule and clitoral region tend to exhibit poor differentiation and often show invasion into lymphatic vessels and perineural tissue.
Patterns of Metastasis
The main routes of metastasis include direct extension and lymphatic spread, with hematogenous spread occurring in advanced stages.
Direct Extension
Lesions gradually enlarge, infiltrating adjacent skin, mucosa, or organs such as the urethra, vagina, and anus. Advanced stages may involve the bladder and rectum.
Lymphatic Spread
Cancer cells typically spread along lymphatic vessels to the superficial inguinal lymph nodes, then to the deep inguinal lymph nodes, and subsequently to the external iliac, obturator, and internal iliac nodes. Ultimately, they may reach the para-aortic and supraclavicular lymph nodes. Tumors located ≥2 cm from the vulvar midline generally metastasize to ipsilateral lymph nodes, while midline lesions frequently involve bilateral inguinal lymph nodes. Lesions involving the clitoris or posterior vulvar region, or those extending to the urethra, vagina, bladder, or rectum, may directly metastasize to pelvic lymph nodes.
Hematogenous Spread
In advanced stages, hematogenous metastasis primarily involves the lungs and bones.
Clinical Manifestations
Symptoms
Early stages may be asymptomatic. The most common symptoms include vulvar pruritus, localized masses, or ulcers. Pain, fluid discharge, and bleeding may develop with secondary infection or advanced disease.
Physical Signs
The most commonly affected site is the labia majora, followed by the labia minora, clitoris, perineum, urethral meatus, and perianal region. In cases where metastasis involves the inguinal lymph nodes, enlarged, firm, mobile, or fixed lymph nodes may be palpable.
Diagnosis
Thorough Evaluation
A detailed medical history, symptoms, and gynecological examination should be performed. The evaluation includes assessing the lesion's location, size, consistency, mobility, pigmentation changes, and relationships to adjacent organs (e.g., involvement of the urethra, vagina, anus, or rectum), as well as checking for enlarged inguinal lymph nodes on both sides. Examination of the vagina and cervix is also performed to rule out tumors in other sites.
Histopathological Examination
Histopathology is the only definitive method of diagnosis for vulvar carcinoma. Vulvar excrescences, ulcers, and suspicious lesions require early biopsy. Specimens must be of adequate depth and include adjacent normal skin and subcutaneous tissue. Colposcopy-guided biopsy can be used for sampling suspicious lesions.
Other Diagnostic Tools
Techniques such as cytology, imaging (ultrasound, MRI, CT, or whole-body PET/CT), cystoscopy, proctoscopy, HPV testing, and HIV testing provide additional diagnostic support or help in differential diagnosis.
Advanced, Metastatic, and Recurrent Disease Assessment
Techniques such as mismatch repair (MMR) testing, microsatellite instability (MSI) analysis, programmed death-ligand 1 (PD-L1), tumor mutation burden (TMB), and NTRK gene fusion testing may be employed in these cases.
Differential Diagnosis
Vulvar squamous cell carcinoma needs to be differentiated from benign or other conditions, including vulvar papilloma, vulvar tuberculosis, and lichen-related vulvar diseases.
Staging
The 2021 International Federation of Gynecology and Obstetrics (FIGO) surgical-pathological staging system is employed for vulvar malignancies, excluding malignant melanoma.
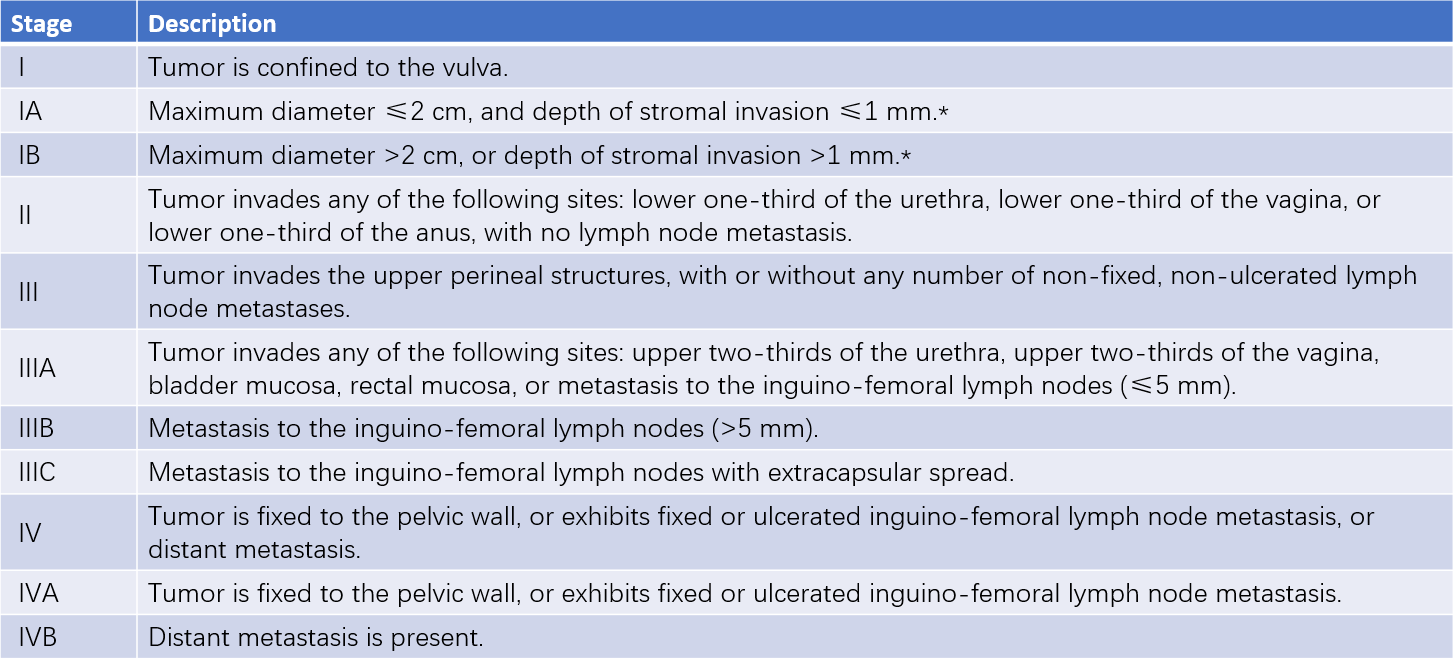
Table 1 Staging of vulvar cancer (FIGO, 2021)
Note: * The depth of invasion refers to the distance from the basement membrane of the epithelium of the most adjacent dermal papilla to the deepest point of invasion.
Treatment
Early-stage tumors are primarily managed with surgery, while locally advanced tumors are treated with a combination of surgery and radiotherapy or chemotherapy. Advanced or metastatic tumors are addressed with palliative radiotherapy and chemotherapy alongside symptomatic and supportive care. In early cases, surgical range tends to be minimized to preserve the normal anatomy of the vulva without compromising prognosis, aiming to improve the patient’s quality of life.
Surgical Management
Early Tumors (Stage I and lesions ≤4 cm in Stage II)
Initial biopsy of the lesion is performed, followed by staging based on the lesion's size and depth of invasion, with surgical approaches tailored accordingly. Surgical margins should be at least 1 cm from the tumor edge, and the depth should extend to the level of the deep perineal fascia, which corresponds to the fascia plane at the level of the pubic symphysis.
Stage IA involves simple partial vulvectomy, followed by regular postoperative follow-up.
Stage IB requires surgical decisions based on lesion location:
- Unilateral lesions (≥2 cm from the vulvar midline) involve radical partial vulvectomy with evaluation of ipsilateral inguinal lymph nodes, either through sentinel lymph node biopsy or unilateral inguinal-femoral lymphadenectomy.
- Midline lesions (anterior or posterior) involve radical partial vulvectomy with bilateral inguinal lymph node evaluation, either through sentinel lymph node biopsy or bilateral inguinal-femoral lymphadenectomy.
Subsequent decisions regarding adjuvant therapy are made depending on the pathological findings of both the primary lesion and lymph nodes.
Locally Advanced Tumors (lesions >4 cm in Stage II and Stage III)
Management of inguinal lymph nodes and vulvar lesions is done in stages. Imaging studies and lymph node pathology evaluations are performed first, followed by individualized surgical treatment or a combination of surgery and radiotherapy/chemotherapy based on the results.
Tumors with Metastases Beyond the Pelvis
Local control measures or palliative external beam radiotherapy and/or systemic therapy may be considered, as well as optimal supportive care approaches.
Radiotherapy
Despite the sensitivity of squamous cell carcinoma to radiotherapy, vulvar skin demonstrates poor tolerance to radiation, often resulting in skin edema, ulceration, and severe pain. Achieving curative radiation doses is challenging. Radiotherapy is commonly used as adjuvant therapy after initial surgery, as primary treatment for locally advanced disease, or as second-line/palliative therapy for recurrent or metastatic disease.
Chemotherapy or Targeted Therapy
Chemotherapy and targeted therapy are commonly administered as part of concurrent radiochemotherapy or as treatments for advanced or recurrent cancer. Frequently used drugs include cisplatin, carboplatin, paclitaxel, fluorouracil, and gemcitabine, either as monotherapy or in combination regimens, with bevacizumab often added. Biomarker-directed second-line systemic treatments may involve:
- Pembrolizumab for tumors exhibiting high tumor mutation burden (TMB-H), PD-L1 positivity, or microsatellite instability hypermutated (MSI-H)/mismatch repair-deficient (dMMR) characteristics.
- Nivolumab for HPV-associated advanced/metastatic recurrent vulvar cancer.
- Larotrectinib or entrectinib for tumors with NTRK gene fusion positivity.
Prognosis
The overall prognosis for vulvar squamous cell carcinoma is relatively favorable, with a five-year survival rate of approximately 70%. Prognostic factors include tumor stage, histological grade, patient age, tumor size, and lymphovascular space invasion. Among these, tumor stage and the number and condition of inguinal lymph node metastases are the most critical factors influencing prognosis.
Follow-Up
Patients treated for vulvar carcinoma are followed closely, with evaluations conducted every 3–6 months during the first two years post-treatment, every 6–12 months during years three to five, and annually thereafter. Cervical/vaginal cytology and HPV testing are recommended to identify epithelial lesions of the lower genital tract at an early stage. Radiotherapy may affect the accuracy of cytological results. Imaging and laboratory tests are performed in cases where recurrence is suspected.