Disorders of sexual development (DSD) refer to a group of conditions characterized by one or more congenital abnormalities or inconsistencies involving sex chromosomes, gonads, external genitalia, or secondary sexual characteristics.
Classification
The classification of DSD is relatively complex, but it is currently preferred to categorize the conditions into three main groups based on karyotype:
- Sex chromosome DSD
- 46,XX DSD
- 46,XY DSD
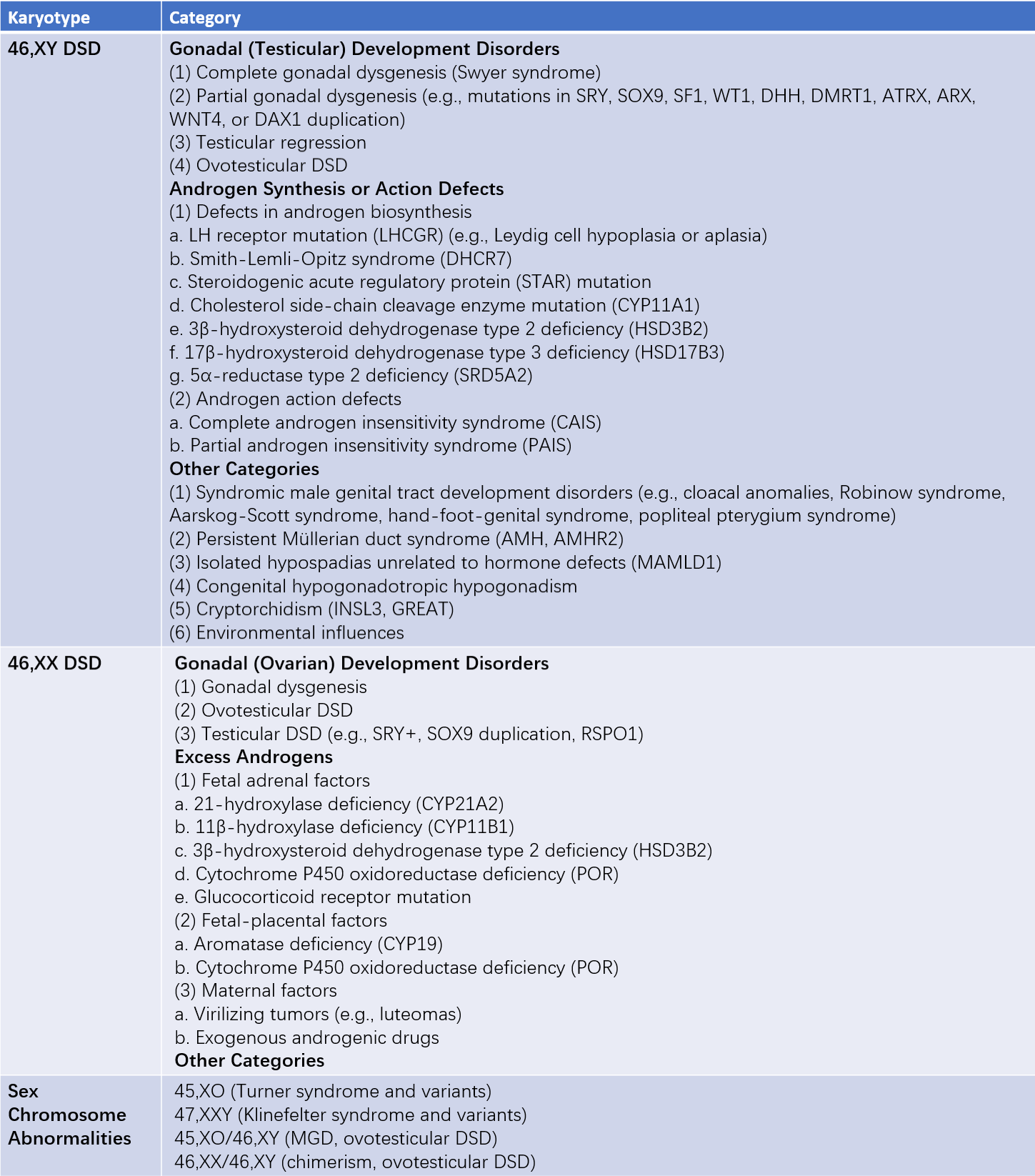
Table 1 Classification of disorders of sexual development
Note: MGD (mixed gonadal dysgenesis)
Common Clinical Manifestations
Based on the consistency between secondary sexual characteristics, sex chromosomes, gonads, and genital structures, this section briefly introduces common disorders of sexual differentiation, with a focus on the features of secondary sexual characteristics.
Sexual Development Disorders with Normal Secondary Sexual Characteristics
This group is characterized by an XX karyotype. Secondary sexual characteristics and ovarian development are typically normal, but abnormalities are present in the development of internal genitalia.
Sexual Development Disorders with Underdeveloped Secondary Sexual Characteristics
This group is mostly associated with chromosomal abnormalities. Karyotypes may include 45,XO, mosaics of 45,XO (e.g., 45,XO/46,XX), or 47,XXX.
Turner Syndrome
Turner syndrome is the most common sexual development disorder, with chromosomal abnormalities such as 45,XO, mosaic forms (e.g., 45,XO/46,XX), or structural abnormalities of the X chromosome. The main pathological feature is ovarian dysgenesis, accompanied by abnormal somatic growth. Clinical manifestations include wide-set eyes, short stature (below 150 cm), webbed neck, shield chest, and cubitus valgus. Secondary sexual characteristics fail to develop, and hypoplasia of the uterus with primary amenorrhea is observed. Treatment focuses on promoting height, stimulating the development of breasts and genitalia, and preventing osteoporosis.
46,XY Pure Gonadal Dysgenesis
Also referred to as Swyer syndrome, this can be divided into complete and partial types. The karyotype is 46,XY. The primitive gonads fail to differentiate into testes, thus neither Müllerian-inhibiting factor (MIF) nor androgens are produced. As a result, the Müllerian ducts persist, leading to the formation of a uterus and vagina, and external genitalia appear female. Patients typically present with underdeveloped secondary sexual characteristics and primary amenorrhea. The external genitalia and vagina are childlike, and the uterus is small. Hormone replacement therapy can promote uterine development and menstruation. The gonads, which appear as streak gonads or dysplastic testes, are prone to tumor development and should be surgically removed upon diagnosis. Partial cases of 46,XY pure gonadal dysgenesis may exhibit masculinized external genitalia, which can be addressed with reconstructive surgery.
Masculinization in Female Sexual Development Disorders
This group of patients has a 46,XX karyotype, ovaries as gonads, and internal genitalia including a uterus, fallopian tubes, and vagina. However, exposure to excessive androgens during embryonic or fetal development leads to varying degrees of masculinization of the external genitalia. The degree of masculinization depends on the timing and amount of androgen exposure. Mild cases may show posterior fusion of the labia, while severe cases may exhibit fused labia and clitoromegaly. The causes of excess androgen production primarily include congenital adrenal hyperplasia (CAH) and androgen exposure from other sources.
Congenital Adrenal Hyperplasia (CAH)
CAH is an autosomal recessive disorder caused by genetic defects in adrenal enzymes required for cortisol synthesis. The most common type, accounting for 90–95% of CAH cases, is 21-hydroxylase deficiency. A deficiency in this enzyme prevents the conversion of 17α-hydroxyprogesterone to cortisol, resulting in reduced cortisol production. This removes the negative feedback on the hypothalamic-pituitary axis, leading to increased secretion of adrenocorticotropic hormone (ACTH), adrenal hyperplasia, and overproduction of androgens. In female fetuses, this results in varying degrees of external genital masculinization. Early treatment of the simple virilizing form of 21-hydroxylase deficiency is critical. Excessive adrenal androgen production can accelerate epiphyseal fusion, so delayed treatment can lead to shorter adult height. Early treatment also helps prevent further masculinization. Abnormal external genitalia may be corrected surgically.
Androgens from Other Sources
Maternal intake of androgenic medications during early pregnancy can lead to mild masculinization of the external genitalia in female fetuses. However, this does not worsen after birth or during puberty, and reproductive endocrine hormone levels typically remain within the normal range.