Vaginal trichomoniasis, also known as trichomonal vaginitis (TV), is a common vaginitis caused by Trichomonas vaginalis and is also a common sexually transmitted infection.
Pathogen
Trichomonas vaginalis demonstrates strong viability and thrives in moist environments with temperatures of 25-40°C and a pH of 5.2-6.6. Its growth is inhibited in environments with a pH below 5.0. The organism can survive for up to 23 hours on moist towels and clothing. Changes in vaginal pH occur before and after menstruation; after menstruation, the pH becomes near neutral, allowing the trichomonads hidden in the glands and vaginal folds to multiply. As a result, vaginal trichomoniasis often recurs around the menstrual period. Trichomonads consume or engulf glycogen within vaginal epithelial cells, which inhibits lactic acid production and raises the vaginal pH. They also consume oxygen, creating an anaerobic vaginal environment conducive to anaerobic bacterial overgrowth. Approximately 60% of patients with trichomoniasis concurrently develop bacterial vaginosis. In addition, Trichomonas vaginalis can engulf sperm, reducing sperm viability in the vagina and contributing to infertility. Beyond colonizing the vagina, the organism frequently invades the urethra, periurethral glands, bladder, or even the renal pelvis, leading to a variety of clinical symptoms.
Modes of Transmission
The primary mode of transmission of Trichomonas vaginalis is direct sexual contact. Trichomonads can inhabit the folds of the penile foreskin, the urethra, or the prostate gland in men. Men infected with trichomoniasis are often asymptomatic, acting as reservoirs of infection. The organism can also be transmitted indirectly through contaminated items such as bathtubs, towels, toilet seats, and clothing.
Clinical Presentation
The incubation period ranges from 4 to 28 days. Approximately 70-85% of individuals are asymptomatic or experience mild symptoms. Without treatment, infections can persist for months to years. The primary symptoms include increased vaginal discharge and vulvar itching, occasionally accompanied by burning, pain, or dyspareunia. The characteristic vaginal discharge is thin, purulent, foamy, and foul-smelling. The discharge may appear gray-yellow or yellow-white and purulent due to a high leukocyte count; it may turn greenish-yellow when co-infections occur. The foamy texture and odor result from the anaerobic fermentation of carbohydrates by trichomonads, producing malodorous gases. Itching is localized primarily to the vaginal introitus and vulva. When urethral involvement occurs, symptoms may include frequency, dysuria, or, in some cases, hematuria. Gynecological examination often reveals congested vaginal mucosa, and in severe cases, scattered petechiae or bleeding spots may appear on the cervix, giving it a "strawberry-like" appearance. Some asymptomatic patients may have no noticeable changes in vaginal mucosa.
Diagnosis
Diagnosis is straightforward based on typical clinical manifestations, with confirmation achieved by detecting trichomonads in vaginal secretions. The simplest diagnostic method involves a saline wet mount of vaginal discharge, under which motile Trichomonas vaginalis exhibiting wavy movements and increased leukocytes can be observed via microscopy. The sensitivity of this method is 40-70%. Sexual intercourse, vaginal douching, or local medications should be avoided for 24-48 hours prior to specimen collection. During the sample collection, vaginal speculums should not be lubricated, and specimens should be sent for examination promptly while kept warm to preserve trichomonad motility and facilitate identification. Gram-stained smears of secretions can eliminate trichomonad motility, reducing detection rates. Laboratories with suitable conditions may use nucleic acid amplification testing (NAAT), which offers diagnostic sensitivity and specificity exceeding 95% and is not affected by lubricants, timing of sexual intercourse, or other limitations. Differential diagnosis from other common forms of vaginitis is necessary in clinical practice.
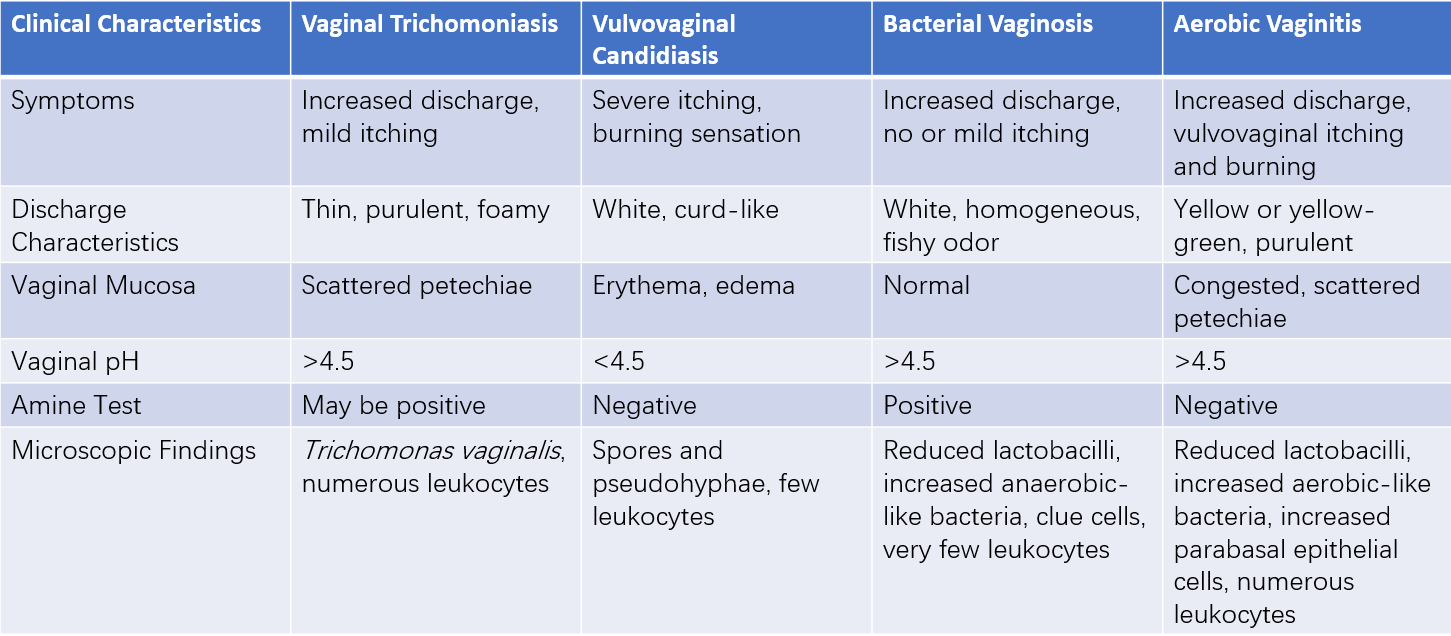
Table 1 Differential diagnosis of four common types of vaginitis
Treatment
Patients with vaginal trichomoniasis may have infections in multiple locations, including the urethra, periurethral glands, and Bartholin's glands; systemic treatment is required to achieve a cure. The primary treatment involves nitroimidazole drugs.
Systemic Treatment
This includes:
- Preferred regimen: Metronidazole 0.4g, twice daily, for 7 days.
- Alternative regimen: Tinidazole 2g as a single dose.
During metronidazole treatment and for 24 hours after its discontinuation, as well as during tinidazole treatment and for 72 hours afterward, alcohol consumption is contraindicated. Breastfeeding is not recommended during treatment.
Treatment of Sexual Partners
Since vaginal trichomoniasis is primarily sexually transmitted, sexual partners should receive concurrent treatment. Patients and their partners should be informed to avoid unprotected sexual activity until the infection is cured.
Follow-Up and Management of Treatment Failure
Given the high reinfection rates, re-testing within three months of initial treatment is recommended for all sexually active women diagnosed with vaginal trichomoniasis. For cases of initial treatment failure without evidence of reinfection, an increased dosage or extended treatment duration may be required, with susceptibility testing performed if possible. The specific regimen involves oral metronidazole or tinidazole 2g once daily for 7 consecutive days. For further treatment failure, tinidazole 2g orally once daily, combined with 0.5g of tinidazole administered intravaginally twice daily for 14 days, may be used. To prevent reinfection, closely used items such as underwear and towels may be disinfected by boiling for 5-10 minutes to eliminate the pathogen.