Aerobic vaginitis (AV) refers to vaginitis caused by the reduction or depletion of normal hydrogen peroxide-producing lactobacilli and an overgrowth of aerobic bacteria.
Etiology
In AV, hydrogen peroxide-producing lactobacilli decrease, while aerobic bacteria proliferate and vaginal microbial diversity increases, leading to dysbiosis of the vaginal microecology. The main pathogens include aerobic and facultative anaerobic bacteria such as Group B Streptococcus, Escherichia coli, Staphylococcus aureus, Enterococcus faecalis, Streptococcus anginosus, and Klebsiella pneumoniae. Factors that promote the changes in the vaginal microbiota in AV remain unclear, but it may be related to the vaginal colonization of intestinal bacteria, local immune dysregulation, or local estrogen deficiency.
Clinical Manifestations
Between 10% and 20% of AV patients exhibit no symptoms. Symptomatic cases are characterized by increased vaginal discharge, vulvovaginal itching or burning, and dyspareunia. The vaginal discharge is typically thin and purulent, yellow to yellow-green in color, and has an unpleasant odor that is not fishy. Gynecological examination may reveal vaginal mucosal redness and swelling, ulcerations, or signs of vaginal mucosal atrophy to varying degrees.
Diagnosis
AV represents vaginal dysbiosis, so bacterial culture is not necessary. Diagnosis can involve the use of saline wet mount diagnostic criteria combined with clinical symptoms and signs, with a score of ≥3 used to diagnose AV. Scores of 3–4 indicate mild AV, 5–6 indicate moderate AV, and 7–10 indicate severe AV.
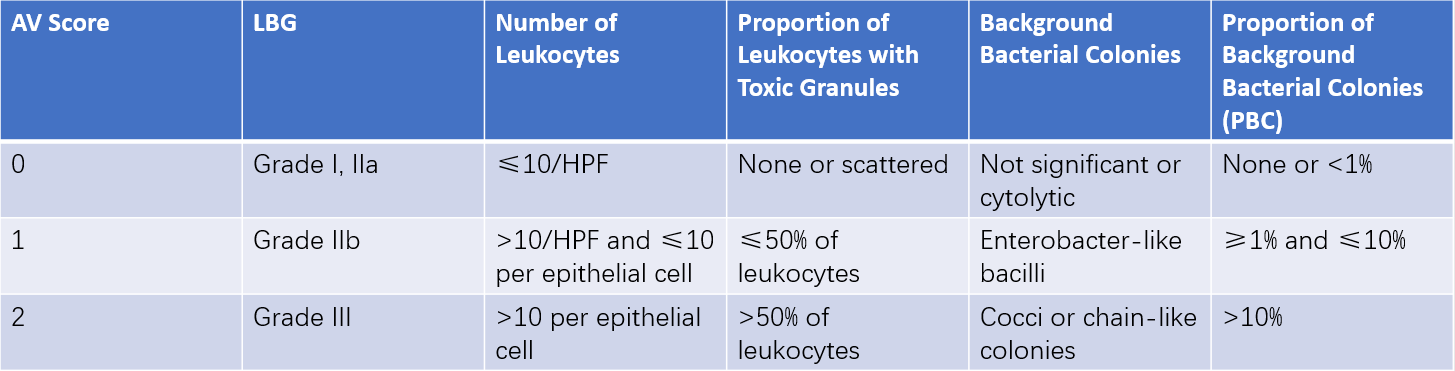
Table 1 Diagnostic criteria for aerobic vaginitis using saline wet mounts
Note:
Based on saline wet mount microscopy (400× magnification, phase-contrast microscope).
LBG: Lactobacillary grade.
Grade I: Dominance of polymorphic lactobacilli, absence of other bacteria.
Grade IIa: Mixed flora dominated by lactobacilli.
Grade IIb: Mixed flora with significantly reduced proportions of lactobacilli compared to other bacteria.
Grade III: Severe reduction or absence of lactobacilli, with excessive growth of other bacteria.
HPF: High power field (400× magnification).
PBC: Parabasal epithelial cells.
Despite its diagnostic utility, the saline wet mount technique has limitations, such as poor specimen preservation, inability to re-examine slides, and high requirements for laboratory personnel and equipment (including the need for phase-contrast microscopy, which makes bacterial observation more challenging). These factors make it less practical.
Gram-stained smears, on the other hand, can be preserved and re-examined and are observed using a standard optical microscope. This method has lower technical and equipment demands, enabling the observation of epithelial cells at 400x magnification and bacterial morphologies at 1,000x magnification for clearer bacterial visualization. As a result, researchers have proposed a combined diagnostic standard for AV that incorporates clinical features and Gram-stained smear observations. Using a Gram-stained vaginal smear viewed under a standard microscope, a total score of ≥4 indicates AV. Scores of 4–5 suggest mild AV, 6–7 suggest moderate AV, and 8–10 indicate severe AV.
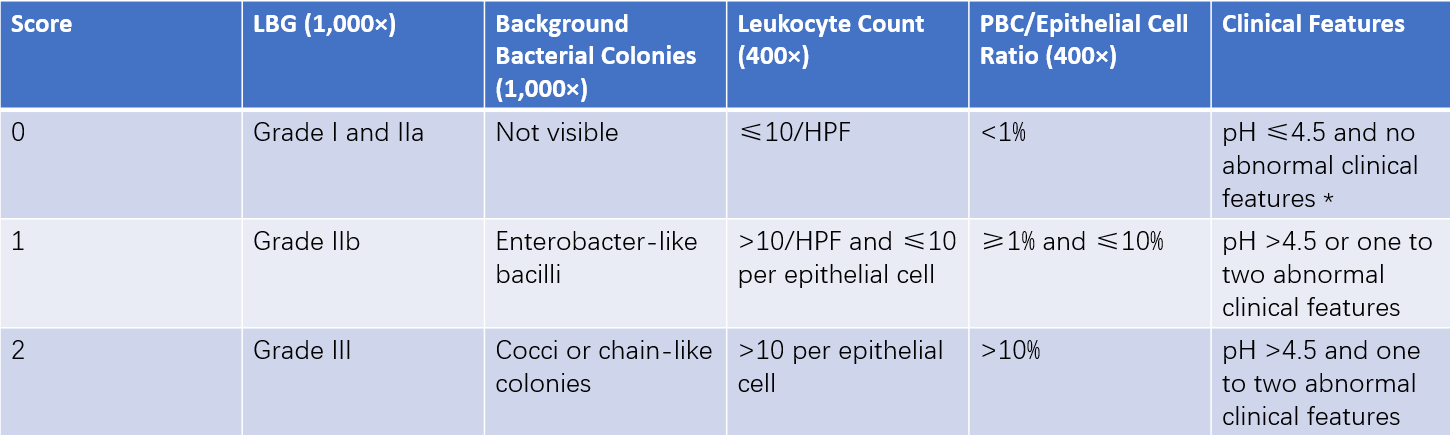
Table 2 Combined diagnostic criteria for aerobic vaginitis using gram-stained smears and clinical features
Note:
*Abnormal clinical features include vaginal mucosal hyperemia and yellow vaginal discharge.
LBG: Lactobacillary grade from 1,000× magnified Gram-stained smears.
HPF: High power field (400× magnification).
PBC: Parabasal epithelial cells.
Treatment
Symptomatic cases require treatment, while there is debate about whether asymptomatic cases require intervention.
Treatment for AV primarily involves the use of antibiotics targeting aerobic bacteria:
- For infections caused by Gram-positive cocci, treatment options include 2% clindamycin cream (5g, applied vaginally once daily for 7–21 days).
- For infections caused by Gram-negative bacilli, oral cefuroxime axetil (0.25g, twice daily for 7 days) may be recommended.
- For mixed infections involving both types of bacteria, oral levofloxacin (0.2g, twice daily for 7 days) or moxifloxacin (0.4g, once daily for 6 days) can be used.
Treatment for Vaginal Mucosal Atrophy may involve vaginal administration of chlorquinaldol-progesterone vaginal tablets (1 tablet daily before bedtime for 12 days).
Treatment for Local Inflammatory Responses of Vulvovaginal Mucosa includes the topical application of glucocorticoids.
Other Treatments may include the use of vaginal probiotics such as lactobacill or other interventions to regulate the vaginal microecology.
Management of Sexual Partners does not require routine screening or treatment of male sexual partners of AV patients.
Follow-Up is recommended in cases where symptoms persist or recur.