Bacterial vaginosis (BV) refers to an endogenous vaginal infection caused by the reduction or depletion of normal hydrogen peroxide-producing lactobacilli and an overgrowth of anaerobic bacteria.
Etiology
Under normal conditions, hydrogen peroxide-producing lactobacilli dominate the vaginal microbiota. In BV, the number of lactobacilli decreases, causing anaerobic microorganisms to proliferate, which disrupts the vaginal microecology. The primary pathogen is Gardnerella vaginalis, as well as other anaerobes such as Mobiluncus, Prevotella, Porphyromonas, Bacteroides, Atopobium vaginae, and Peptostreptococcus. Mixed infections involving Mycoplasma hominis are also common. The exact reasons for changes in the vaginal microbiota remain unclear, but factors such as frequent sexual activity and recurrent vaginal douching have been associated with BV.
Clinical Manifestations
Between 10% and 40% of individuals with BV are asymptomatic. In symptomatic cases, the primary feature is increased vaginal discharge that is thin with a characteristic fishy odor. Mild vulvar pruritus or a burning sensation may occur, and symptoms often worsen after sexual intercourse. The fishy odor is caused by amines (such as putrescine, cadaverine, and trimethylamine) produced by anaerobic bacteria. Gynecological examinations reveal no significant signs of inflammation such as vaginal mucosal congestion. The discharge is thin, homogenous, gray-white in color, and often adheres to the vaginal walls but can be easily removed.
Diagnosis
The diagnosis of BV is made primarily using Amsel's clinical criteria or Nugent's Gram-stain scoring system in the laboratory.
Amsel's Clinical Criteria
A diagnosis is confirmed if three of the following four criteria are present:
- Thin, homogeneous, gray-white vaginal discharge.
- Vaginal discharge with a pH > 4.5.
- Positive whiff test: When a small amount of vaginal discharge is placed on a glass slide and 1–2 drops of 10% potassium hydroxide are added, a fishy odor (resembling spoiled fish) is produced due to amine release.
- Presence of clue cells: Clue cells are exfoliated vaginal squamous epithelial cells with numerous Gardnerella vaginalis and other anaerobic bacteria adhering to their surface and surroundings. In severe BV, clue cells may constitute more than 20% of squamous epithelial cells observed microscopically.
Nugent's Scoring System
This laboratory standard involves Gram-staining a vaginal smear and examining bacterial morphotypes under a 1,000x oil-immersion microscope. A quantification scoring system (0–10) is used:
- 0–3: Normal.
- 4–6: Intermediate BV.
- ≥7: BV confirmed.
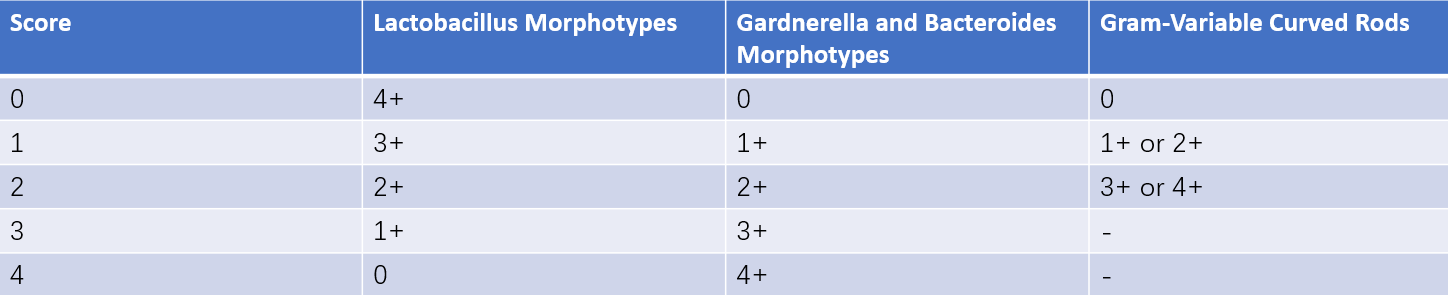
Table 1 Nugent scoring criteria
Note: Each score is based on the average number of bacterial morphotypes observed per 10 oil-immersion fields:
0: No bacteria observed.
1+: Fewer than 1 bacterium.
2+: 1–4 bacteria.
3+: 5–30 bacteria.
4+: More than 30 bacteria.
-: Not applicable.
Additional diagnostic methods include molecular techniques and enzymatic assays. However, as BV involves dysbiosis of the vaginal microbiota, bacterial cultures are of limited diagnostic value.
Treatment
Patients with symptoms require treatment using antibiotics targeting anaerobic bacteria. Common options include metronidazole, tinidazole, and clindamycin. Metronidazole, which inhibits anaerobic bacterial growth without affecting lactobacilli, is considered the preferred treatment.
Systemic Therapy
This includes:
- First-Line: Metronidazole 0.4g, orally, twice daily for 7 days.
- Alternative Regimens: Tinidazole 2g, orally, once daily for 2 days; or tinidazole 1g, orally, once daily for 5 days; or clindamycin 0.3g, orally, twice daily for 7 days. Single-dose administration of 2g metronidazole is no longer recommended.
Topical Therapy
This includes:
- First-Line: Metronidazole 0.75% gel, 5g intravaginally, once daily for 5 days; or metronidazole vaginal effervescent tablets, 0.2g intravaginally, nightly for 7 days; or clindamycin 2% cream, 5g intravaginally, nightly for 7 days.
- Alternative Regimens: Clindamycin suppository, 0.1g intravaginally, nightly for 3 days.
Considerations
BV has been associated with endometritis, pelvic inflammatory disease (PID), and vaginal cuff infections following hysterectomy. Patients scheduled for uterine procedures or hysterectomy should receive treatment even if they are asymptomatic.
BV is linked to adverse pregnancy outcomes such as chorioamnionitis, premature rupture of membranes, preterm delivery, and postpartum endometritis. Pregnant patients with symptoms should be treated.
For recurrent BV, alternative anaerobic-targeting antibiotics or vaginal lactobacillus preparations may aid in restoring and maintaining vaginal microbiota balance.