A physical examination is typically conducted after obtaining the patient's medical history. The scope of the examination includes a general physical assessment, abdominal examination, and gynecological examination. Except for emergency situations, this process is performed in the following sequence. Both significant positive findings and negative findings with diagnostic value are documented. After completing the physical examination, the findings are communicated to the patient or their family members.
General Examination
Standard measurements include body temperature, pulse, respiration, and blood pressure, with weight and height recorded if necessary. Additional features of the examination involve evaluating the patient's consciousness, mental state, facial appearance, body posture, general physical development, hair distribution, skin condition, and superficial lymph nodes—especially the left supraclavicular and inguinal lymph nodes. Examination also includes the head, neck (with attention to thyroid enlargement), breasts (noting development, presence of skin depressions, masses, or milk/other discharge), heart, lungs, spine, and extremities.
Abdominal Examination
The abdominal examination forms an essential component of a gynecological physical assessment and is performed prior to the gynecological examination. Visual inspection assesses the abdomen for abnormalities such as prominence, frog-belly shape, scars, varicose veins, stretch marks, abdominal hernias, or rectus abdominis diastasis. Palpation evaluates abdominal wall thickness and checks for enlargement or tenderness in the liver, spleen, and kidneys. The presence of abdominal tenderness, rebound tenderness, muscle rigidity, or masses is assessed. If a mass is palpable, its location, size (in centimeters), shape, texture, mobility, surface smoothness or irregularity, and tenderness are described. Percussion identifies tympanic and dull sounds and delineates their distribution while noting the presence of shifting dullness. Auscultation is performed, if necessary, to evaluate bowel sounds. In patients who are pregnant, the size of the abdomen, uterine fundal height, fetal position, fetal heart rate, and fetal size are examined.
Gynecological Examination
The gynecological examination, referred to as a pelvic examination, includes an assessment of the external genitalia, vagina, cervix, uterus, and bilateral adnexa.
General Guidelines
Physicians are expected to demonstrate care and consideration for the patient by maintaining a polite attitude, using gentle language, and performing meticulous and gentle examination techniques. Patients are informed that discomfort may occur during the examination and are encouraged to relax their abdominal muscles.
Except for patients with urinary incontinence, the bladder should be emptied prior to the examination; catheterization may be performed if necessary. Patients with full bowels should undergo examination after defecation or an enema.
To avoid cross-contamination, disposable drapes or paper sheets placed under the patient are replaced after each use.
The lithotomy position is typically used, with the patient’s hips positioned at the end of the table, their head slightly elevated, and arms relaxed at their sides to promote abdominal muscle relaxation. The examiner stands between the patient’s legs. For critically ill patients who cannot be repositioned, examinations are performed in bed.
Gynecological examinations are avoided during menstruation unless there is abnormal vaginal bleeding requiring evaluation. Antiseptic cleansing of the vulva is performed prior to the examination, and sterile gloves and instruments are utilized to prevent infection.
Speculum and bimanual examinations are contraindicated in patients without a history of sexual activity. For these patients, recto-abdominal diagnoses are performed instead. Speculum or bimanual examinations may only be carried out when absolutely necessary, and only after obtaining consent from the patient and their family members.
For uncooperative patients with thick abdominal walls or high muscle tension, or for suspected pelvic pathologies, ultrasound is performed if a satisfactory bimanual examination is not possible. Anesthesia-assisted examination may be considered, if necessary.
Examination Methods and Procedures
External Genital Examination
This involves inspecting the development of the external genitalia, distribution of pubic hair (female or male pattern), and noting any abnormalities such as deformities, dermatitis, ulcers, masses, or growths. Changes in skin and mucosal color, pigmentation, or texture are assessed, along with signs of thickening, thinning, or atrophy. The labia minora are separated to expose the vaginal vestibule for evaluation of the urethral opening and vaginal introitus. The appearance and surroundings of the urethral opening—such as mucosal coloration and presence of growths—are observed. In women without sexual experience, the hymen is typically intact but may barely allow the insertion of a single finger. In sexually active women, the vaginal introitus can accommodate two fingers, while in multiparous women, remnants of the hymen or scars from an episiotomy may be observed. The patient is asked to bear down during the examination to check for prolapse of the vaginal anterior or posterior wall, uterine prolapse, or urinary incontinence.
Speculum Examination
When visualizing the vagina and cervix with a speculum, the structural details of the instrument must be considered:
Insertion and Removal
Duckbill speculums are commonly used for clinical purposes, enabling vaginal treatment procedures. Speculums come in different sizes and are selected according to vaginal width. During insertion, the blades are initially closed, lubricated, and inserted at an oblique angle along the posterior vaginal wall to avoid damage. However, if cervical cytology or vaginal secretion smears are planned, sterile saline is used instead of lubricant to prevent interference with sample quality. The labia minora are parted with one hand while the speculum is gently and gradually inserted with the other hand, avoiding the sensitive area around the urethra. After insertion, the blades are opened to expose the cervix, vaginal walls, and fornices. The speculum is rotated as needed to ensure complete visualization before withdrawal. When removing the speculum, the blades are closed and withdrawn slowly along the posterior vaginal wall.
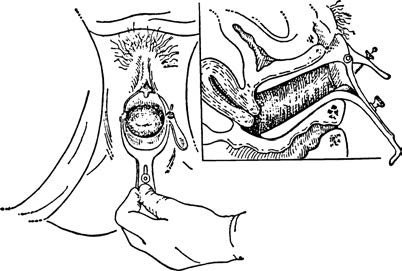
Figure 1 Vaginal speculum examination
Frontal and lateral views as seen after the speculum is in place, exposing the cervix and lateral vaginal walls.
Visual Inspection
Vaginal Examination
The anterior, posterior, and lateral walls of the vagina, as well as the mucosal folds of the fornices, are inspected for color, presence of folds, and congenital anomalies such as vaginal septa or double vagina. Abnormalities such as ulcers, masses, or cysts are assessed, and the amount, consistency, color, and odor of vaginal discharge are evaluated. If discharge appears abnormal, additional tests for Trichomonas, Candida, Neisseria gonorrhoeae, and clue cells are conducted. It is important to differentiate normal from abnormal discharge, as all healthy women produce some degree of vaginal secretions.
Cervical Examination
Upon exposing the cervix, its size, color, and external os shape are evaluated for signs of bleeding, enlargement, erosion-like changes, lacerations, eversion, nabothian cysts, polyps, or masses. Discharge or bleeding from the cervical canal is noted. Samples from the squamo-columnar junction at the cervical os may be collected for cytology and HPV testing.
Bimanual Examination
Bimanual examination is a critical component of gynecological assessment. In this procedure, two fingers or one finger of one hand are placed in the vagina while the other hand palpates the abdomen. This approach examines the vagina, cervix, uterus, fallopian tubes, ovaries, parametrium, and pelvic cavity walls to identify any abnormalities.
Examination Technique
The examiner wears sterile gloves, lubricates the index and middle fingers, and gently inserts them along the posterior vaginal wall. This process evaluates vaginal patency, depth, elasticity, deformities, scars, masses, and the condition of the vaginal fornices. The cervix is then palpated for its size, shape, consistency, condition of the external os, and whether there is any contact bleeding.
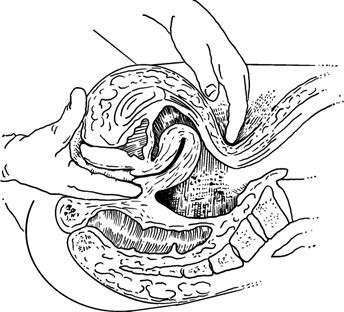
Figure 2 Bimanual examination (Examining the uterus)
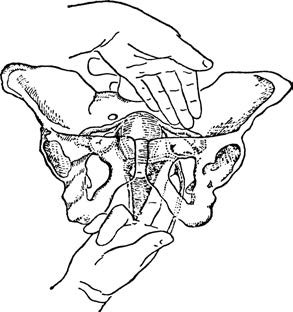
Figure 3 Bimanual examination (Examining the adnexa)
The uterus is next examined by positioning the vaginal fingers behind the cervix and placing the other hand palm-down flat on the abdomen at the umbilicus. While the vaginal fingers lift the cervix upward and forward, the abdominal hand presses downward and backward toward the pubic symphysis. This coordinated upward lifting and downward pressing maneuver evaluates the uterus's position, size, shape, consistency, mobility, and tenderness. A normal uterus is typically anteverted and slightly anteflexed.
Version refers to the relationship between the uterine axis and the body axis. When the uterus is tilted anteriorly toward the pubic bone, it is described as anteverted; when it is tilted posteriorly toward the sacrum, it is retroverted.
Flexion refers to the relationship between the uterine body and the cervix. An anteriorly angled relationship is termed anteflexion, while a posterior angle is referred to as retroflexion.
After evaluating the uterus, the vaginal fingers are moved from behind the cervix to one of the lateral fornices, attempting to palpate deeper into the pelvic region. Simultaneously, the abdominal hand palpates downward from the iliac crest on the same side. This coordination assesses the adnexal region for masses, thickening, or tenderness. If a mass is detected, its location, size, shape, consistency, mobility, relationship to the uterus, and tenderness are recorded. Normal ovaries may occasionally be palpable and produce mild soreness upon examination, while normal fallopian tubes are typically non-palpable.
Vagino-Recto-Abdominal Examination
The vagino-recto-abdominal examination combines vaginal, rectal, and abdominal evaluations. After completing the bimanual exam, the examiner inserts the index finger into the vagina and the middle finger into the rectum, following the same general steps as the bimanual process. This serves as a supplement to the bimanual examination by addressing areas that may not have been thoroughly assessed.
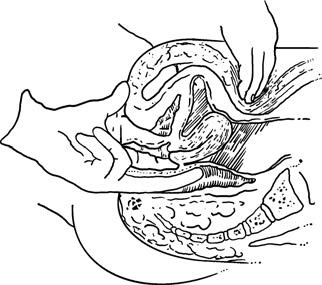
Figure 4 Vagino-recto-abdominal examination
This technique can clarify the size of a retroverted or retroflexed uterus, detect abnormalities in the uterine posterior wall, parametrium, rectouterine pouch, uterosacral ligaments, and the posterior pelvic region. It also helps to evaluate the extent of pelvic pathology and its relationship to the uterus or rectum, particularly in cases involving tumors and their connection to the pelvic wall. Additionally, it identifies abnormalities in the rectovaginal septum, the anterior sacrum, or within the rectum. This examination is particularly significant in evaluating genital cancers, tuberculosis, endometriosis, and pelvic inflammatory conditions.
Recto-Abdominal Examination
The recto-abdominal examination involves inserting the index finger of one hand into the rectum while using the other hand to palpate the abdomen. This technique is suitable for patients without a history of sexual activity, those with vaginal atresia, or when bimanual examination is otherwise inappropriate.
Key Considerations for Bimanual, Vagino-Recto-Abdominal, or Recto-Abdominal Examinations
Adhering to the following principles can facilitate the examination process:
- If the patient experiences pain or discomfort while two fingers are inserted into the vagina, the examination can be performed with a single finger.
- During the vagino-recto-abdominal examination, instructing the patient to bear down as if defecating when inserting the middle finger into the rectum can help relax the anal sphincter and reduce discomfort.
- For patients with tense abdominal muscles, conversing with them during the examination and encouraging open-mouth breathing may help relax the abdominal muscles.
- If the examiner is unable to clarify pelvic anatomical relationships, persistent palpation is generally not recommended, as it may cause undue discomfort without yielding additional diagnostic value. Under such circumstances, the examination may be discontinued, and satisfactory findings are often achieved in subsequent evaluations.
Documentation of Findings
After completing the gynecological examination, findings are organized and recorded in sequential anatomical order.
External Genitalia
Notes include the developmental condition and marital/reproductive history classification (such as unmarried, married but nulliparous, or multiparous). Abnormal findings are described in detail.
Vagina
Assessment includes vaginal patency, condition of the mucosa, quantity, color, and consistency of secretions, and whether there is any abnormal odor.
Cervix
Documentation includes size, consistency, presence of erosion-like changes, lacerations, polyps, nabothian cysts, as well as contact bleeding, tenderness upon lifting, or pain with movement.
Uterine Body
Notes include position, size, consistency, mobility, surface smoothness or irregularity, and tenderness.
Adnexa (Ovaries and Fallopian Tubes)
Findings include the presence of masses, thickening, or tenderness. If a mass is detected, its position, size, consistency, surface smoothness, mobility, tenderness, and its relationship to the uterus and pelvic walls are documented. The findings for the left and right sides are recorded separately.
Laboratory and Special Tests
Existing laboratory and special test results are summarized. Results from external facilities should include the name of the institution and the date of the examination.