Umbilical Cord Presentation and Prolapse
When the umbilical cord is positioned anteriorly or to the side of the presenting fetal part without rupture of the membranes, it is referred to as umbilical cord presentation (or occult prolapse of the umbilical cord). When the umbilical cord descends through the cervical os and into the vagina or extends beyond the external genitalia after membrane rupture, it is referred to as umbilical cord prolapse.
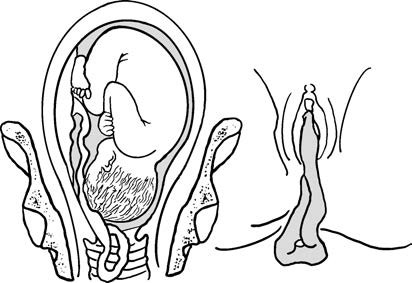
Figure 1 Umbilical cord prolapse
Etiology
Common causes include:
- Lack of engagement of the fetal head, such as cephalopelvic disproportion or difficulty in descent into the pelvis.
- Abnormal fetal presentations, including breech presentation, shoulder presentation, or occipitoposterior position.
- Small fetal size or excessive amniotic fluid volume.
- Long umbilical cord.
- Abnormal attachment of the umbilical cord, such as marginal insertion, and low-lying placenta.
Effects on the Mother and Fetus
Effects on the Mother
Rates of cesarean delivery and assisted births through operative interventions increase.
Effects on the Fetus
If umbilical cord presentation occurs before engagement of the presenting fetal part while membranes remain intact, intermittent compression of the umbilical cord may occur during uterine contractions as the presenting part descends, resulting in transient fetal heart rate abnormalities. If engagement has occurred and membranes are ruptured, the umbilical cord may become compressed between the presenting part and the pelvic bones, leading to fetal hypoxia or complete cessation of the fetal heart rate. Cases involving vertex presentations are generally more severe, while shoulder presentations are less severe. If blood flow through the umbilical cord is blocked for more than 7–8 minutes, intrauterine fetal death may occur.
Diagnosis
Umbilical cord prolapse should be suspected in cases with associated risk factors. Umbilical cord presentation may be indicated when fetal heart rate decelerations occur suddenly after fetal movements or uterine contractions and improve rapidly with changes in maternal position or displacement of the presenting part combined with elevation of the maternal pelvis. Continuous fetal heart rate monitoring is recommended during labor for cases at risk. In the presence of ruptured membranes and fetal heart rate abnormalities, vaginal examination is necessary to assess for cord prolapse and detect vascular pulsations within the umbilical cord. Diagnosis is confirmed if the cord is palpated next to or anterior to the presenting fetal part or if it is detected within the vagina or externally beyond the genitalia. Ultrasound imaging, particularly with color Doppler ultrasound, facilitates diagnostic confirmation.
Management
Umbilical Cord Presentation
For multiparous women with intact membranes and effective uterine contractions, adoption of a head-down and pelvis-elevated position may assist in fetal head engagement. With progressive cervical dilation and consistently normal fetal heart rates, vaginal delivery may proceed. Primiparous women and cases involving footling or shoulder presentations are generally managed by cesarean delivery.
Umbilical Cord Prolapse
For cases of umbilical cord prolapse where fetal heart rates remain normal and the fetus is alive, expedited delivery is essential.
- When the cervix is fully dilated: Instrumental delivery using forceps is performed for head presentations already engaged in the pelvis, while breech extraction is used for breech presentations.
- When the cervix is not fully dilated: Immediate repositioning of the pregnant woman to a head-down and pelvis-elevated position, upward displacement of the presenting fetal part, and administration of medications to suppress uterine contractions are utilized to relieve or reduce cord compression. Continuous fetal heart rate monitoring is employed while preparations for cesarean delivery are made as quickly as possible.
Prevention
Late pregnancy and intrapartum ultrasound examinations may assist in early detection of umbilical cord presentation. For fetuses with unengaged presenting parts during labor, unnecessary or frequent rectal and vaginal examinations should be avoided.
Umbilical Cord Entanglement
Umbilical cord entanglement refers to the wrapping of the cord around the fetal neck, limbs, or torso. Approximately 90% of such cases involve nuchal cord entanglement, with a single loop around the neck being the most common, accounting for roughly 20% of deliveries. Causes are associated with excessive cord length, small fetal size, excessive amniotic fluid volume, and frequent fetal movements. The effects of nuchal cord entanglement depend on the tightness of the wrapping, the number of encircling loops, and the cord's length.
Clinical Features
Obstruction of Fetal Descent
Umbilical cord entanglement may shorten the effective cord length, hindering engagement of the presenting fetal part and causing prolonged or arrested labor.
Fetal Distress
When the cord is tightly wrapped or subjected to traction during contractions, fetal blood flow may be impaired, leading to fetal hypoxia.
Fetal Heart Rate Variability
Frequent variable decelerations may occur if intrauterine hypoxia develops.
Ultrasound Findings
Color Doppler imaging may reveal blood flow signals around the fetal neck.
Physical Signs on Ultrasound
Skin impressions at the site of cord entanglement are visible on ultrasound. A single loop may appear as a U-shaped mark containing a small circular hypoechoic area and short echogenic stripes. Two loops typically create a W-shaped impression, while three or more loops form a serrated pattern with a linear hypoechoic band. Special attention is required when frequent decelerations on cardiotocography cannot be resolved with changes in maternal position or oxygen supplementation. In such cases, pregnancy termination may be necessary. Prenatal ultrasound confirmation of cord entanglement calls for enhanced fetal monitoring during labor. Signs of fetal distress should prompt timely intervention.
Abnormal Umbilical Cord Length
The normal umbilical cord length ranges from 30 to 100 cm, with an average length of 55 cm. An umbilical cord shorter than 30 cm is referred to as an excessively short cord, while a cord longer than 100 cm is considered excessively long.
Excessively Short Cord
During pregnancy, an excessively short cord usually does not exhibit clinical manifestations. However, during labor, excessive traction may occur as the presenting fetal part descends, potentially disrupting fetal circulation. This may result in fetal heart rate abnormalities, fetal hypoxia, or, in severe cases, placental abruption. Obstructed descent of the presenting part is common, leading primarily to prolonged second-stage labor. Lack of improvement in fetal heart rate despite oxygen supplementation may necessitate cesarean delivery.
Excessively Long Cord
An excessively long cord increases the risk of complications such as nuchal cord entanglement, wrapping around the body, cord knotting, prolapse, or cord compression.
Umbilical Cord Knotting
Umbilical cord knots may be classified as false or true knots:
False Knots
These typically result from the umbilical vessels being longer than the cord and looping or twisting to resemble knots. A false knot may also occur due to tortuosity of the umbilical vein (which is longer than the arteries). False knots usually pose little harm to the fetus.
True Knots
True knots are rare and typically form when the cord wraps around the fetal body and subsequently creates a knot as the fetus moves through a loop. Untightened true knots typically do not cause any symptoms; however, if a knot tightens, restricted fetal blood flow may lead to intrauterine fetal death. True knots are most commonly diagnosed post-delivery.
Umbilical Cord Torsion
Umbilical cord torsion occurs when fetal movements twist the cord along its axis to form a spiral pattern, which is physiologically normal and may involve 6–11 twists. Excessive torsion near the fetal umbilical insertion site may thin the cord, cause necrosis with vascular obstruction, and result in fatal loss of blood supply to the fetus.
Abnormal Attachment of the Umbilical Cord
The umbilical cord normally attaches to the fetal navel and the placental fetal surface near its center.
###Fetal Site Abnormalities
Abnormal umbilical cord attachment to the fetus may result in omphalocele or gastroschisis, which can be clarified via ultrasound imaging. Management of the pregnancy depends on the presence of structural abnormalities and their prognosis.
Placental Site Abnormalities
When the cord attaches near the placental margin, the condition is referred to as battledore placenta. This typically does not affect the mother or fetus during labor and is identified post-delivery during placental examination.
When the cord attaches to the fetal membranes rather than the placental disc, the vessels traverse between the amnion and chorion to reach the placenta, a condition called velamentous cord insertion.
Complications of Velamentous Cord Insertion
If the cord vessels pass over the internal cervical os and lie anterior to the presenting part, the condition is termed vasa previa. The absence of Wharton's jelly protection renders these vessels susceptible to compression during contractions or rupture during membrane rupture. This can lead to impaired fetal circulation and fetal hemorrhage, increasing the risk of fetal distress or sudden fetal death.
Velamentous cord insertion poses a severe risk to the fetus, emphasizing the importance of ultrasound localization of the cord's attachment to the placenta, particularly in cases of low-lying placental position during late gestation. Pregnant individuals with risk factors for vasa previa, such as cord insertion abnormalities, bilobed or accessory placentas, or vaginal bleeding, may benefit from transvaginal color Doppler ultrasound evaluation. Pregnant individuals diagnosed with velamentous cord insertion and vasa previa require close monitoring during pregnancy. Pulmonary maturation should be promoted before 35 weeks of gestation, and cesarean delivery should be scheduled electively before labor onset or membrane rupture.
Umbilical Vessel Abnormalities
A normal umbilical cord contains three vessels: one vein and two arteries. In cases where only a single artery is present, the condition is referred to as single umbilical artery.
Diagnostic Considerations
Most cases can be identified via prenatal ultrasound. If single umbilical artery is detected without additional structural abnormalities, neonatal prognosis is typically favorable. However, when structural abnormalities coexist, the risks of chromosomal aneuploidy and other malformations increase, including renal dysplasia, imperforate anus, and vertebral defects. Prenatal diagnostic evaluations are recommended in such cases.