After the 28th week of pregnancy, when the placenta is positioned lower than the presenting part of the fetus and attaches to the lower segment of the uterus, with its margins close to or covering the internal cervical os, it is referred to as placenta previa. Placenta previa is the most common cause of vaginal bleeding in late pregnancy and is a serious pregnancy complication. Its incidence is approximately 0.3% to 0.5%.
Etiology
The exact cause of placenta previa remains unclear but is believed to be associated with the following factors:
Abnormalities of the Placenta
Abnormalities in the shape or size of the placenta may contribute. When the placenta is positioned normally but accessory lobes extend into the lower uterine segment near the internal cervical os, or when the placenta is unusually large and thin (e.g., membranous placenta), it may extend into the lower uterine segment. Twin pregnancies have a higher incidence of placenta previa compared to singleton pregnancies, with the risk being approximately doubled.
Endometrial Pathology or Damage
Conditions such as a history of cesarean section, uterine surgery, multiple miscarriages with dilation and curettage, puerperal infections, and pelvic inflammatory disease may lead to endometritis or atrophic changes of the endometrium. Implantation of the fertilized egg into damaged endometrium may result in poor vascular development of the uterine decidua, inadequate placental blood supply, and compensatory extension of the placenta into the lower uterine segment to obtain adequate nutrition. Uterine scarring from previous cesarean deliveries may impede the upward migration of the placenta during the later stages of pregnancy, as the uterine isthmus expands. Poor development of the decidua in the lower uterine segment can also result in abnormal placental invasion into the myometrium, leading to placenta accreta spectrum (PAS) disorders. Placenta previa is a common high-risk factor for PAS disorders.
Delayed Development of the Trophoblast
When the trophoblast has not yet developed sufficiently to allow proper implantation, the fertilized egg may continue to descend into the uterine cavity and implant in the lower uterine segment, leading to the development of placenta previa.
Other High-Risk Factors
Factors such as the use of ovulation induction medications during assisted reproductive technologies (ART) may alter sex hormone levels, and the process of external fertilized egg cultivation and artificial implantation may disrupt the synchronization between endometrial and embryonic development. Artificial embryo transfer can also induce uterine contractions, leading to implantation in lower segments of the uterus. Additional risk factors include uterine anomalies, smoking, and a history of placenta previa in previous pregnancies.
Classification
Placenta previa is categorized into four types based on the relationship between the lower edge of the placenta and the internal cervical os:
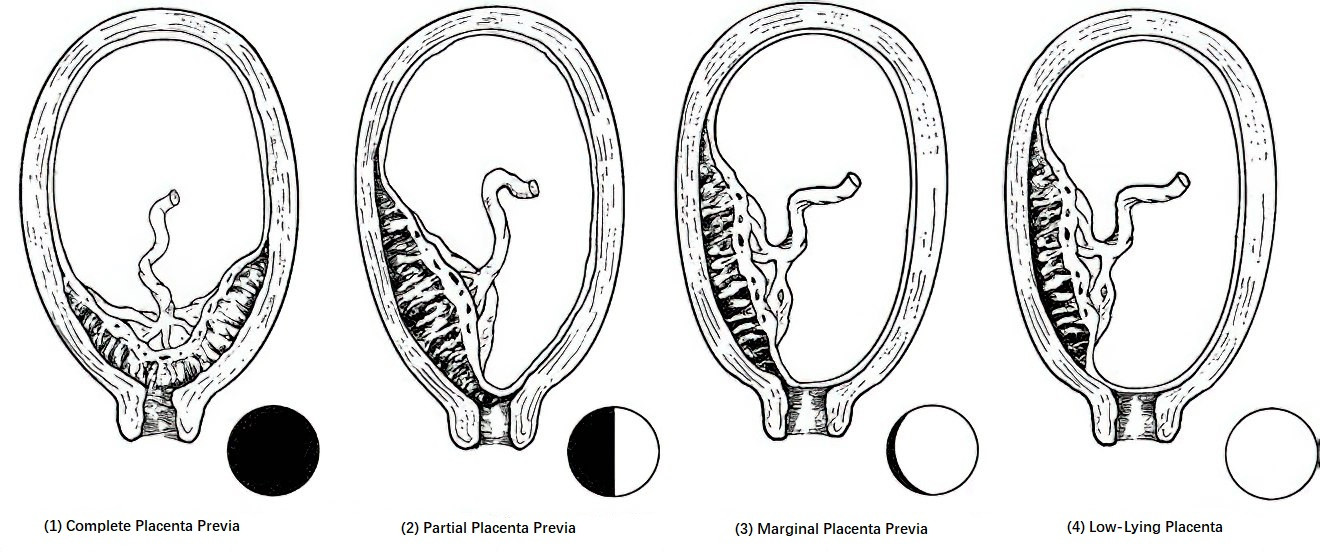
Figure 1 Types of placenta previa
Complete Placenta Previa (Central Placenta Previa)
The placenta completely covers the internal cervical os.
Partial Placenta Previa
The placenta partially covers the internal cervical os.
Marginal Placenta Previa
The placenta is attached to the lower uterine segment, with its edge reaching the internal cervical os but not extending beyond it.
Low-Lying Placenta
The placenta is attached to the lower uterine segment, with its edge located less than 2 cm from the internal cervical os.
Due to factors such as the formation of the lower uterine segment, cervical canal effacement, and dilation of the cervix, the relationship between the placenta's margin and the internal cervical os may change with advancing gestation. Clinical classification is determined based on the most recent examination results prior to management.
Clinical Manifestations
Symptoms
The classic symptom is painless, recurrent vaginal bleeding that occurs in late pregnancy or during the onset of labor without any apparent trigger. In late pregnancy, the elongation of the lower uterine segment results in cervical traction and gradual shortening of the cervical canal. During labor, regular uterine contractions cause the cervical canal to efface and become part of the soft birth canal. When the lower uterine segment forms and the cervix dilates, the placenta's attachment to this area becomes misaligned due to its limited stretchability, leading to separation from the uterine wall and rupture of placental blood sinuses, resulting in bleeding. Bleeding often occurs without any obvious precipitating factors, and the initial bleeding episodes are usually mild and tend to stop spontaneously due to clot formation. However, severe bleeding can occur during the first episode, potentially leading to life-threatening hemorrhage and shock. The frequency and volume of bleeding typically increase as the lower uterine segment continues to stretch. The timing, quantity, and recurrence of bleeding are closely associated with the type of placenta previa.
Signs
The severity of symptoms is directly related to the volume and rate of bleeding. Massive hemorrhage may result in pale skin, weak pulse, cold extremities, and a drop in blood pressure indicative of shock. Recurrent bleeding can result in anemia. Abdominal examination usually reveals a soft uterus, no tenderness, clear uterine contours, and uterine size consistent with gestational age. The placenta's location in the lower uterine segment may prevent engagement of the presenting part, resulting in a high and floating fetal presentation. Approximately one-third of cases are associated with abnormal fetal positions. Severe bleeding, whether recurrent or massive, may cause fetal hypoxia, abnormal or absent fetal heart tones, or intrauterine fetal demise. If the placenta is attached to the anterior uterine wall, placental blood flow sounds may be audible above the symphysis pubis.
Diagnosis
High-Risk Factors
A history of multiple miscarriages, uterine surgeries, puerperal infections, advanced maternal age, cesarean deliveries, and multiparity may be associated with placenta previa.
Clinical Features
Symptoms
The typical symptom is painless, recurrent vaginal bleeding during late pregnancy or labor, without any apparent trigger. The clinical condition of the patient is often proportional to the amount of blood loss. Severe bleeding can cause symptoms such as pallor, a rapid and weak pulse, and a drop in blood pressure, indicative of shock.
Signs
The uterus is soft, well-defined, non-tender, and its size corresponds to the gestational age. The fetal position is usually identifiable. The presenting part of the fetus is often high and floating, and abnormal fetal positions may coexist. For confirmed placenta previa, vaginal examinations are generally avoided. If vaginal examination is absolutely necessary to confirm the diagnosis or determine the mode of delivery, it should be performed under conditions where intravenous fluids, blood transfusion, and emergency cesarean section are immediately available.
Imaging Studies
Ultrasound Examination
Ultrasound is able to clearly visualize the uterine wall, placenta, presenting part of the fetus, and the cervix, and is useful for determining the type of placenta previa. Transvaginal ultrasound provides greater accuracy in assessing the relationship between the placental edge and the internal cervical os compared to abdominal ultrasound. For suspected cases of abnormal placental positioning, transvaginal ultrasound is typically recommended.
Placenta previa diagnosis via ultrasound requires consideration of gestational age. During mid-pregnancy, the portion of the placenta covering the uterine cavity is approximately half its area, whereas by late pregnancy, this has reduced to about one-third or one-quarter. Formation of the lower uterine segment increases the distance between the internal cervical os and the placental edge. Placentae that were initially attached to the lower uterine segment may migrate upward toward the uterine fundus as pregnancy progresses, resulting in a normal placental location. Placental previa identified during mid-pregnancy should not be definitively diagnosed as placenta previa but referred to as a "low-lying placenta."
Magnetic Resonance Imaging (MRI)
For suspected cases of placenta accreta spectrum disorders, MRI may be employed in facilities where it is available to evaluate the depth of placental invasion into the uterine myometrium and assess potential involvement of the bladder, rectum, or adjacent uterine tissues.
Differential Diagnosis
Placenta previa should be differentiated from other causes of antepartum bleeding, such as placental abruption, rupture of placental marginal blood sinuses, velamentous cord insertion, ruptured vasa previa, and cervical lesions. Differentiation is usually straightforward when integrating the patient’s medical history, clinical presentation, and results from auxiliary diagnostic tests.
Impact on Mother and Fetus
Intrapartum and Postpartum Hemorrhage
During cesarean deliveries for placenta previa, excessive bleeding may occur if the uterine incision cannot avoid the placenta attached to the anterior uterine wall. After fetal delivery, thinning and poor contractility of the myometrium in the lower uterine segment can complicate complete placental separation. When the placenta does separate, the open venous sinuses in the poorly contractile lower uterine segment may fail to close, leading to significant postpartum hemorrhage that is difficult to control. If placenta previa is accompanied by placenta accreta spectrum disorders, the risk of postpartum hemorrhage is further elevated.
Anemia and Infection
Recurrent episodes of vaginal bleeding during pregnancy may result in maternal anemia. Additionally, bacteria ascending through the vagina to the placental separation site near the external cervical os may increase the risk of infection.
Adverse Perinatal Outcomes
Rates of therapeutic preterm delivery are higher in placenta previa, leading to increased incidences of low birth weight and neonatal mortality. Severe maternal bleeding may result in fetal distress, intrauterine fetal demise, or neonatal death.
Management
The treatment principles include suppression of uterine contractions, correction of anemia, and timely termination of pregnancy. Management depends on factors such as the type of placenta previa, severity of bleeding, the overall condition of the pregnant woman, gestational age, fetal status, and whether labor has begun. Patients with placenta previa complicated by placenta accreta spectrum disorders should receive care in hospitals equipped with appropriate emergency response capabilities.
Expectant Management
The goal is to prolong pregnancy as much as possible to improve fetal survival while ensuring the safety of both the mother and fetus. Expectant management is appropriate for pregnancies under 36 weeks gestation, with a viable fetus, when the general condition of the patient is stable, vaginal bleeding is minimal, and there is no immediate need for delivery. This approach is recommended in medical facilities equipped to handle maternal and fetal emergencies. Hospitalization is emphasized once vaginal bleeding occurs, with close monitoring and treatment of maternal and fetal conditions.
General Measures
Potential triggers of uterine contractions, such as fatigue, stress, constipation, and diarrhea, should be avoided. Activities should be restricted during periods of vaginal bleeding, with emphasis on rest. Rectal examinations and unnecessary vaginal examinations should be prohibited. Vaginal bleeding should be closely monitored, fetal status should be evaluated, and normal blood volume should be maintained. Blood transfusions may be given when necessary. Blood supplies should be routinely prepared in case emergency surgery is required.
Suppression of Uterine Contractions
Uterine contraction inhibitors may be administered to patients at risk of preterm labor to prevent further bleeding caused by contractions.
Correction of Anemia
Hemoglobin levels should be raised to ≥110 g/L, and hematocrit levels to ≥0.30, to improve maternal reserves.
Corticosteroids
When there is a risk of preterm labor before 34 weeks of gestation, corticosteroids may be used to promote fetal lung maturity.
Termination of Pregnancy
Indications
Significant bleeding, potentially leading to hemorrhagic shock, requires immediate termination of pregnancy to save the mother’s life, without consideration of fetal status.
Emergency surgical delivery is recommended if there are obstetric indications such as fetal distress and the fetus is viable.
Placenta previa diagnosed during labor, with substantial bleeding and no likelihood of delivery in the short term, also necessitates termination of pregnancy.
Asymptomatic placenta previa should have its timing for delivery determined based on its type.
Complete placenta previa can be managed with scheduled delivery at 37 weeks of gestation or later.
Partial placenta previa should be evaluated for the degree of cervical os coverage to determine the timing of delivery.
Marginal placenta previa can be managed with scheduled delivery at 38 weeks of gestation or later.
Patients with a history of recurrent vaginal bleeding, complications such as placenta accreta spectrum disorders, or other high-risk factors may require termination of pregnancy between 34 and 37 weeks of gestation.
Surgical Management
Cesarean section is the primary method of delivery for placenta previa. The procedure should be performed by skilled surgeons with a clear plan for stepwise management. Preoperative measures include correcting anemia, preventing infection, ensuring sufficient blood supply, and preparing for postpartum hemorrhage and neonatal care. The placenta should be localized through preoperative ultrasound or intraoperative evaluation, and the uterine incision should avoid the placenta as much as possible. After fetal delivery, uterine contraction should be enhanced. Various methods, including local sutures, uterine compression sutures, uterine cavity packing with gauze, uterine artery or internal iliac artery ligation, and uterine artery embolization, may be used to control bleeding. If bleeding cannot be controlled, a hysterectomy may be performed after thorough communication with the patient and family.
If a localized area of significantly distended blood vessels is observed in the lower uterine segment during cesarean section, and placenta previa is found at the site of a previous cesarean scar, placenta accreta spectrum disorders should be highly suspected. Comprehensive measures should be in place for the management of maternal and neonatal complications and emergencies.
Vaginal Delivery
Vaginal delivery is an option only in cases of marginal placenta previa or low-lying placenta, with a cephalic presentation, minimal vaginal bleeding, and a high likelihood of a rapid delivery. It should be conducted in a well-equipped facility with adequate blood supplies and close monitoring.
Prevention
Effective contraception should be practiced to reduce the incidence of multiple induced abortions and uterine procedures, thereby minimizing the risk of infection. Strict adherence to indications for cesarean section is necessary to reduce cesarean delivery rates. Routine prenatal care should be standardized to facilitate early diagnosis and proper management of placenta previa.