Spontaneous abortion refers to the loss of an embryo or fetus before it has developed the capacity for survival, and is defined as the termination of pregnancy before 28 weeks gestation or when the fetal weight is less than 1,000 grams. Pregnancies terminating before 12 weeks are classified as early spontaneous abortion, while those occurring at or after 12 weeks are termed late spontaneous abortion. Spontaneous abortion accounts for approximately 15–25% of all pregnancies, with 80% classified as early abortions. Among early abortions, roughly two-thirds occur before the expected menstrual period, a phenomenon referred to as biochemical pregnancy.
Etiology
The causes of spontaneous abortion include factors related to the embryo, the mother, the father, and the environment.
Embryonic Factors
Chromosomal abnormalities in the embryo represent the most common reason for early pregnancy loss, accounting for 50–60%. In comparison, chromosomal abnormalities are responsible for about one-third of mid-pregnancy losses and only 5% of late-pregnancy losses. These abnormalities can involve numerical or structural anomalies. Among numerical anomalies, trisomy is the most frequent, with common examples including trisomy 13, 16, 18, 21, and 22, followed by X monosomy. Triploidy and tetraploidy are rare. Structural abnormalities, while less common, may also result in spontaneous abortion.
Maternal Factors
Systemic Diseases
Conditions such as severe infection, high fever, severe anemia, heart failure, thrombotic disorders, chronic wasting diseases, chronic liver or kidney disorders, and hypertension can all contribute to spontaneous abortion. Though TORCH infections might not significantly impact the mother, they can infect the fetus and lead to pregnancy loss.
Genital Abnormalities
Abnormalities of the uterus—such as uterine hypoplasia, bicornuate uterus, unicornuate uterus, septate uterus, and double uterus—or conditions like submucosal fibroids, certain intramural fibroids, adenomyosis, and intrauterine adhesions can impair embryo implantation and development, leading to spontaneous abortion.
Cervical insufficiency, caused by congenital cervical developmental abnormalities or acquired cervical trauma, results in an inability to sustain pregnancy, often culminating in late-term pregnancy loss. It is seen as a common cause of late spontaneous abortion.
Endocrine Disorders
Conditions like luteal phase deficiency, hyperprolactinemia, polycystic ovary syndrome, thyroid dysfunction (hypothyroidism or hyperthyroidism), poorly controlled diabetes mellitus, and others can lead to spontaneous abortion.
Severe Stress and Harmful Habits
Physical stressors during pregnancy, including surgical procedures, direct trauma to the abdomen, or excessive sexual activity, along with psychological stressors such as severe anxiety, tension, fear, or grief, can contribute to pregnancy loss. Smoking, caffeine, alcohol, and drug consumption may also increase the risk of miscarriage in a dose-dependent manner.
Immune Dysfunction
Immune-related causes include both autoimmune dysfunction and alloimmune imbalances. Autoimmune disorders such as antiphospholipid syndrome (APS), systemic lupus erythematosus (SLE), undifferentiated connective tissue disease, and Sjögren's syndrome may induce localized or systemic inflammatory damage, potentially leading to pregnancy loss. Alloimmune responses are based on the theory that pregnancy functions as an allogeneic transplant. Immune tolerance at the maternal-fetal interface is essential for fetal survival, and disruptions in this balance may contribute to recurrent unexplained pregnancy losses.
Prethrombotic State (PTS)
PTS is characterized by pathological physiological changes in the blood's cellular and non-cellular components, resulting in a hypercoagulable state and a predisposition to thrombus formation, also known as thrombophilia. During pregnancy, PTS can lead to microthrombi formation in spiral arteries or chorionic villous vessels, causing multifocal placental infarcts. This disrupts uteroplacental circulation, increasing the risk of miscarriage or intrauterine fetal demise.
Paternal Factors
Research has established that chromosomal abnormalities in sperm can contribute to spontaneous abortion. However, there is insufficient evidence to confirm whether a significantly increased rate of sperm deformities directly correlates with pregnancy loss.
Environmental Factors
Exposure to excessive radiation or harmful substances such as arsenic, lead, formaldehyde, benzene, chloroprene, and ethylene oxide may result in spontaneous abortion.
Pathology
In early spontaneous abortion, the embryo is often no longer viable before being expelled. This process is typically accompanied by bleeding within the decidua basalis, necrosis of surrounding tissues, and separation of embryonic villi. Once separated, the embryonic tissue acts as a foreign body, triggering uterine contractions that usually result in the complete expulsion of pregnancy-related materials. However, in some cases, incomplete or failed expulsion occurs, leading to significant bleeding.
In late spontaneous abortion, the majority of fetuses still have a detectable heartbeat prior to expulsion. This process often begins with abdominal pain, followed by the expulsion of the fetus and placenta. In certain cases, the cervix may dilate and the fetus may be expelled without noticeable labor symptoms. A smaller proportion of fetuses lose their heartbeat before expulsion, after which the fetus is expelled naturally.
Clinical Manifestations
Key clinical features include vaginal bleeding and abdominal pain following amenorrhea.
Early Spontaneous Abortion
Prior to the expulsion of pregnancy-related materials, the embryo is typically already dead. Bleeding and separation of the chorionic villi from the decidua occur first, opening blood sinuses and causing vaginal bleeding. The detached embryo and accumulated blood stimulate uterine contractions, resulting in the expulsion of the embryo and other pregnancy-related materials, accompanied by paroxysmal lower abdominal pain. After complete expulsion, uterine contraction closes the blood sinuses, and bleeding stops.
Late Spontaneous Abortion
In most cases, the fetus remains viable prior to expulsion, often due to uterine anatomical abnormalities. The clinical course resembles preterm labor, with the fetus being delivered first, followed by the placenta, with minimal bleeding. In other cases, the fetus may have already died before expulsion. Non-anatomical factors, such as severe fetal developmental abnormalities, autoimmune disorders, prethrombotic states, intrauterine infections, or abnormalities in pregnancy-related tissues, are common causes in such cases.
Clinical Types
Spontaneous abortion is classified into different clinical types based on its developmental stages.
Threatened Abortion
Threatened abortion refers to the onset of vaginal bleeding before 28 weeks of gestation, often presenting as a small amount of dark red blood or blood-stained discharge. No pregnancy-related materials are expelled, and paroxysmal lower abdominal or lumbar pain occurs subsequently. Gynecological examination reveals an intact cervix, unruptured membranes, and uterine size consistent with gestational age. Symptoms may resolve with rest and treatment, allowing the pregnancy to continue. However, increased vaginal bleeding or intensified abdominal pain may progress to inevitable abortion.
Inevitable Abortion
Inevitable abortion refers to cases where miscarriage cannot be prevented. On the basis of threatened abortion, vaginal bleeding volume increases, paroxysmal lower abdominal pain intensifies, or amniotic fluid may be observed draining from the vagina due to ruptured membranes. Gynecological examination shows cervical dilation, and embryonic tissues or amniotic sacs may sometimes obstruct the cervix. Uterine size is generally consistent with or slightly smaller than gestational age.
Incomplete Abortion
Incomplete abortion arises as the progress of inevitable abortion, where portions of pregnancy-related materials are expelled from the uterine cavity while others remain inside or are trapped within the cervix. Retention of placental tissue in the uterine cavity or cervix after fetal expulsion can hinder uterine contractions, resulting in persistent bleeding and, in severe cases, shock. Gynecological examination reveals a dilated cervix with retained pregnancy tissues blocking the cervical canal and continuous bleeding. The uterus is smaller than the gestational age.
Complete Abortion
Complete abortion refers to cases where all pregnancy-related materials have been expelled, with vaginal bleeding ceasing gradually and abdominal pain alleviating. Gynecological examination shows a closed cervix with the uterus returning to near-normal size.
Special Situations
Missed Abortion
Also known as a delayed abortion, this occurs when the embryo or fetus has died but remains in the uterine cavity without being expelled promptly. Symptoms include the cessation of early pregnancy-related signs, the presence or absence of symptoms associated with threatened abortion, and the cessation of uterine enlargement. In mid-pregnancy, failure of continued abdominal growth and absent fetal movements are observed. Gynecological examination reveals a closed cervix with a uterus smaller and firmer than expected for the timeframe of amenorrhea, along with the absence of fetal heartbeat.
Recurrent Spontaneous Abortion (RSA)
RSA is defined as two or more consecutive spontaneous abortions (including biochemical pregnancies) with the same sexual partner. It occurs predominantly in the early stages of pregnancy but can also appear in the late stages. The causes of RSA are similar to those of sporadic abortion, but the relative contribution of each factor differs. For instance, the frequency of embryonic chromosomal abnormalities decreases with successive abortion events. Common causes of early RSA include chromosomal abnormalities, immune dysfunction, luteal phase deficiency, and hypothyroidism. Common causes of late RSA include uterine anatomical abnormalities, autoimmune dysfunction, and prethrombotic states. In many cases, the etiology and mechanisms of RSA remain unexplained. Cases where all known causes are excluded are termed unexplained recurrent spontaneous abortion (URSA).
Abortion with Infection
Infection may complicate abortion when prolonged vaginal bleeding occurs, pregnancy-related tissues remain in the uterine cavity, or unsafe abortion methods are employed. Uterine cavity infections frequently involve mixed anaerobic and aerobic bacterial pathogens. Severe infections can spread to the pelvic cavity, abdominal cavity, or systemically, leading to complications such as pelvic inflammatory disease, peritonitis, sepsis, or infectious shock.
Diagnosis
Diagnosing spontaneous abortion is generally straightforward and can often be confirmed based on the patient’s medical history and clinical manifestations. Only a minority of cases require auxiliary examinations. After confirming a diagnosis of spontaneous abortion, determining the clinical type is necessary to guide the appropriate treatment plan.
Medical History
A comprehensive inquiry should cover whether the patient has a history of amenorrhea or recurrent pregnancy loss, early pregnancy symptoms, vaginal bleeding (amount and duration), the expulsion of pregnancy-related materials, abdominal pain (location, nature, and severity), fever, the characteristics of vaginal secretions, and whether an odor is present.
Physical Examination
Examination involves measuring temperature, pulse, respiratory rate, and blood pressure, as well as observing for signs of anemia or infection. After sterile preparation of the external genital area, gynecological examination may provide information on cervical dilation, bulging of the amniotic sac, obstruction of the cervical os by pregnancy-related materials, uterine size relative to gestational length, uterine tenderness, and any tenderness or masses in the adnexa. Careful and gentle techniques are emphasized during these procedures.
Auxiliary Examinations
Ultrasound
Ultrasound imaging helps assess the location, shape, and viability of the gestational sac, enabling confirmation of its position and the viability of the embryo, which informs treatment strategies. An abnormal shape or lower position of the gestational sac typically indicates poor prognosis. Ultrasonography can assist in diagnosing incomplete and missed abortions. Before 8 weeks of gestation, transvaginal ultrasound provides greater accuracy.
Urine and Blood hCG Testing
Urine tests using hCG test strips offer rapid confirmation of pregnancy. Blood hCG levels, measured dynamically with higher sensitivity, are helpful for evaluating the progression of pregnancy.
Progesterone Testing
Due to the pulsatile secretion of progesterone within the body, serum progesterone levels exhibit significant fluctuations, limiting their clinical value as a reliable indicator.
Differential Diagnosis
Differentiation of the type of abortion is prioritized. Early spontaneous abortion must be distinguished from ectopic pregnancy, molar pregnancy, and uterine fibroids.
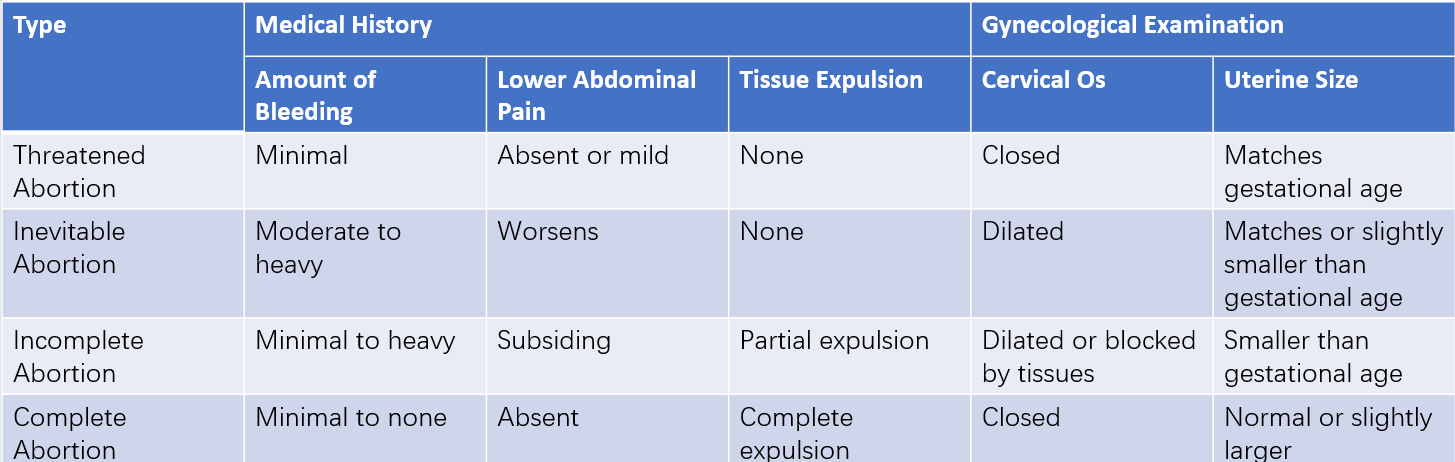
Table 1 Clinical features of different types of spontaneous abortion
Management
Management approaches are determined based on the clinical type of spontaneous abortion.
Threatened Abortion
Adequate rest and abstention from sexual intercourse are recommended. For cases involving luteal phase deficiency, intramuscular or oral administration of progestational agents may be used, while hypothyroidism should be managed with thyroid hormone supplementation. If symptoms resolve and ultrasound indicates embryonic viability, pregnancy may continue. However, symptom aggravation, poor embryonic development on ultrasound, or a stagnant or declining hCG level indicates inevitable abortion, requiring termination of pregnancy.
Inevitable Abortion
Following confirmation, complete expulsion of embryonic or fetal tissues and placental material should be achieved promptly. In early pregnancy, uterine evacuation procedures, such as curettage, are often necessary. Pregnancy-related materials should be thoroughly examined and sent for pathological or genetic testing if conditions allow, aiding in identifying the cause of miscarriage. In late pregnancy, the larger uterine size and greater blood loss may necessitate uterotonic medications to enhance uterine contractions. After fetal and placental expulsion, completeness should be checked, and curettage may be performed to remove residual pregnancy tissues. Prophylactic antibiotic administration is recommended post-procedure to prevent infection.
Incomplete Abortion
Once confirmed, curettage or evacuation utilizing surgical instruments should be undertaken promptly to clear retained materials from the uterine cavity. Patients experiencing significant vaginal bleeding accompanied by shock should receive simultaneous blood transfusion, infusion therapy, and prophylactic antibiotics to prevent infection.
Complete Abortion
With resolved clinical symptoms and ultrasound findings confirming no residual pregnancy materials in the uterine cavity, further treatment is generally unnecessary unless signs of infection are present.
Missed Abortion
Management of missed abortion can present challenges. Placental tissue often becomes organized and adheres firmly to the uterine wall, complicating evacuation procedures. Prolonged retention of late pregnancy tissue increases the risk of coagulation dysfunction and disseminated intravascular coagulation (DIC), potentially leading to severe hemorrhage. Pre-treatment evaluations of blood counts, platelet levels, and coagulation function should be conducted, alongside preparation for blood transfusion. If coagulation function is normal, missed abortions at ≤12 weeks gestation may be managed via surgical, pharmacological, or expectant approaches.
- Surgical Treatment: Includes vacuum aspiration (for pregnancies ≤10 weeks) and curettage (for pregnancies of 10–12 weeks).
- Pharmacological Treatment: May involve prostaglandin analogs alone or in combination with mifepristone.
- Expectant Management: Requires thorough patient counseling, informed consent, close ultrasound monitoring, and an observation period of 7–14 days.
Missed abortions >12 weeks gestation may require either pharmacological or surgical treatment, with curettage being the preferred surgical method, preceded by cervical ripening procedures as needed. Significant coagulation dysfunction calls for the timely transfusion of fresh blood, plasma, and fibrinogen, alongside symptomatic improvement of coagulation function prior to evacuation procedures.
Recurrent Spontaneous Abortion
Identifying underlying causes and implementing targeted treatments is necessary.
- In couples with chromosomal abnormalities, genetic counseling before pregnancy is essential to determine feasibility and the appropriate type of conception (natural or assisted reproductive technology).
- Submucosal fibroids may be removed via hysteroscopic surgery, while intramural fibroids affecting pregnancy may be considered for surgical resection.
- Uterine septa and intrauterine adhesions can be addressed with hysteroscopic septum resection or adhesion lysis.
- Cervical insufficiency may be managed with cervical cerclage.
- Patients with autoimmune diseases or prethrombotic conditions require collaborative management with rheumatologists or immunologists.
- Progesterone supplementation is appropriate for luteal phase insufficiency.
- Thyroid hormone supplementation is needed in cases of hypothyroidism, both before and throughout pregnancy.
Abortion with Infection
Treatment principles prioritize infection control while promptly removing retained intrauterine materials.
If vaginal bleeding is not excessive, broad-spectrum antibiotic therapy is initiated for 2–3 days, followed by curettage once the infection is under control.
If bleeding is significant, broad-spectrum antibiotics are administered intravenously alongside blood transfusion. Retained tissue fragments in the uterine cavity are removed using ovum forceps to reduce bleeding. Comprehensive curettage should be avoided initially to prevent spreading infection.
Postoperative broad-spectrum antibiotics are continued, and thorough curettage can be performed once infection is controlled.
For patients with septic shock, anti-shock treatment is provided, with curettage performed after stabilization.
In cases of severe infection or pelvic abscess formation, surgical drainage may be required, and hysterectomy is considered if necessary.