Importance of Nutrition During Pregnancy
The food consumed daily by pregnant women not only meets the nutritional needs required to maintain their own metabolic functions but also provides the nutrients necessary for the growth and development of the fetus. Research has shown that nutrition, as a critical environmental factor, significantly impacts both the short-term and long-term health of mothers and their offspring. Poor nutrition during pregnancy is associated with complications such as miscarriage, preterm birth, difficult labor, stillbirth, fetal abnormalities, low birth weight, macrosomia, pregnancy-related anemia, preeclampsia, gestational diabetes, and postpartum hemorrhage. Moreover, it may have adverse effects on the postnatal growth and metabolic health of offspring. Therefore, guiding pregnant women to consume adequate amounts of protein, fats, carbohydrates, vitamins, and minerals through a balanced diet composed of diverse foods is essential for improving maternal and fetal outcomes.
Nutritional Requirements for Pregnant Women
Energy
The total energy requirement increases during pregnancy to support fetal growth, placental development, maternal tissue expansion, protein and fat storage, and increased metabolic demands. Additional energy intake is generally unnecessary in early pregnancy. From the fourth month of pregnancy until delivery, an additional 200 kcal per day is required. Staple foods are the main source of energy for most people, and pregnant women are advised to consume 200–450 grams of staple foods per day.
Protein
The demand for protein increases during pregnancy, particularly during the second and third trimesters when fetal growth accelerates. Early in pregnancy, extra protein is not required. Starting from the second trimester, protein intake should increase by 15 grams per day. Primary sources of protein include animal-derived foods such as fish, poultry, eggs, lean meats, and dairy products.
Carbohydrates
Carbohydrates serve as the main source of energy, contributing 50%–60% of the total caloric intake. During the second and third trimesters, an additional 35 grams of grain-based staple foods per day is recommended.
Fats
Fats should account for 25%–30% of total energy intake. Excessive fat consumption may lead to overweight and increase the risk of pregnancy complications. However, long-chain polyunsaturated fatty acids have been shown to support fetal brain and retinal development. Including fish and other seafood, particularly deep-sea fish, as well as walnuts, in the diet may provide benefits.
Vitamins
Vitamins are essential for regulating metabolism and maintaining physiological functions, as well as for fetal growth and development. During early embryonic development, inadequate or excessive vitamin intake may increase the risk of fetal abnormalities. The demand for vitamins rises during the second and third trimesters as the fetus grows rapidly, so vitamin intake needs to be increased throughout pregnancy.
Minerals
Minerals such as calcium, magnesium, iron, zinc, and iodine are crucial for fetal growth and development. Deficiencies can lead to fetal growth restriction, and early deficiencies may result in congenital abnormalities. Due to increased blood volume during pregnancy, physiological anemia is more likely to occur, necessitating increased intake of trace elements throughout pregnancy.
Dietary Fiber
Dietary fiber is not absorbed by the body but plays a role in reducing the absorption of sugars and fats, slowing blood sugar elevation, and preventing or alleviating constipation and improving intestinal function. Foods rich in dietary fiber, such as vegetables, low-sugar fruits, and whole grains, are recommended during pregnancy.
Dietary Guidelines for Pregnant Women
Pregnant women should follow general dietary guidelines while incorporating the following five additional recommendations:
- Folic acid supplementation, regular consumption of iron-rich foods, and the use of iodized salt.
- For those experiencing severe nausea and vomiting during pregnancy, small, frequent meals should be consumed, ensuring adequate intake of foods containing necessary amounts of carbohydrates.
- Moderate increases in the intake of milk, fish, poultry, eggs, and lean meat during the second and third trimesters.
- Moderate physical activity to maintain appropriate weight gain during pregnancy.
- Smoking and alcohol should be avoided, and preparation for breastfeeding should be prioritized.
Early Pregnancy
Meals that are light, palatable, and easy to digest help reduce pregnancy-related symptoms. These include fresh vegetables and fruits, soy products, fish, poultry, eggs, and various cereal products.
The frequency, quantity, variety, and timing of meals should be adjusted based on the appetite and severity of symptoms experienced. Meals consumed in smaller portions but more frequently can help ensure adequate intake.
A minimum of 130 grams of carbohydrates per day is recommended during early pregnancy. Easily digestible cereal-based staples, such as approximately 200 grams of whole wheat flour or 180 grams of rice, should be prioritized. Pregnant women who experience severe nausea and are unable to consume sufficient carbohydrates should seek medical assistance to avoid adverse effects on early fetal brain development. A perfectly balanced diet may not always be necessary during this time.
A lack of folic acid during early pregnancy increases the risk of neural tube defects and preterm birth. Women should consume folate-rich foods such as animal liver, dark green leafy vegetables, and legumes starting at the planning stage of pregnancy. It is also recommended to supplement with 400–800 μg of folic acid daily.
Nicotine in tobacco and cyanide and carbon monoxide in smoke can lead to fetal hypoxia, malnutrition, and developmental delays. Alcohol can cross the placenta and cause poor fetal growth, central nervous system abnormalities, and other complications.
Mid to Late Pregnancy
In the second trimester, total daily protein intake should increase by 50 grams. In the third trimester, an additional 75 grams of protein per day is required. Fish, especially deep-sea varieties high in docosahexaenoic acid (DHA), are beneficial for fetal brain and retinal development. Consuming deep-sea fish 2–3 times per week is encouraged.
Dairy products are rich in protein and are an excellent source of calcium. Starting in the second trimester, a daily intake of 250–500 grams of dairy products is recommended, along with supplementation of 600 mg calcium.
The recommended iodine intake during pregnancy is 230 μg per day. In addition to using iodized salt, pregnant women should consume iodine-rich foods like seaweed and kelp 1–2 times per week.
Pregnant women are prone to iron-deficiency anemia. To meet the increased need for fetal iron storage, iron intake should be increased starting in the second trimester. This includes an additional 20–50 grams of red meat daily and the consumption of organ meats or animal blood 1–2 times per week. Iron supplements can be taken if medically indicated.
At least 30 minutes of moderate-intensity physical activity daily, such as walking, aerobics, swimming, or yoga, can support appropriate weight gain and facilitate natural labor.
Tobacco and alcohol have well-documented toxic effects on fetal development at all stages. Stimulants, such as caffeine, should also be limited or avoided.
Weight Management
Weight Gain During Pregnancy
Maternal weight gain can impact the short- and long-term health of both the mother and child. In recent years, the increase in overweight and obese pregnant women has been linked to excessive weight gain during pregnancy, which raises the risk of complications such as delivering large-for-gestational-age infants, difficult births, birth injuries, and gestational diabetes. Conversely, insufficient weight gain is associated with restricted fetal growth, preterm birth, and low birth weight. Proper attention must be given to pregnancy weight management. Pre-pregnancy Body Mass Index (BMI) should be determined during the first prenatal visit to provide individualized guidance on weight gain, diet, and exercise.
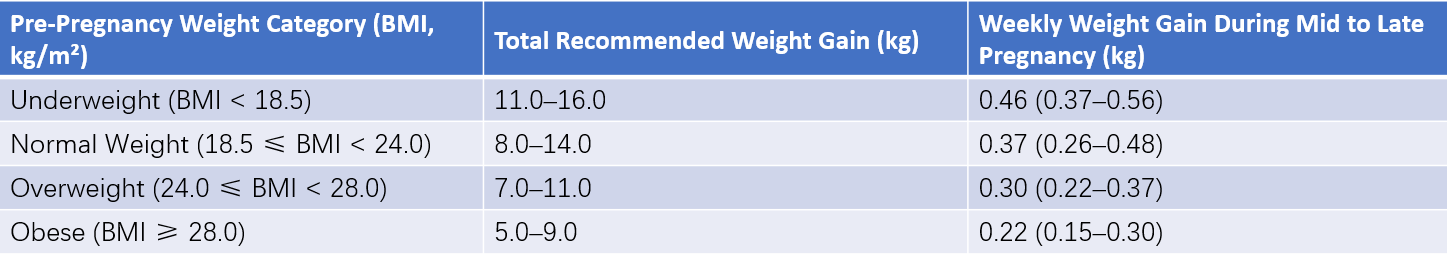
Table 1 Recommended weight gain standards during pregnancy
Exercise Guidance
Exercise is a key component of weight management during pregnancy. Physical activity helps improve muscle strength, enhance metabolism, promote blood circulation, improve gastrointestinal motility to reduce constipation, strengthen abdominal and pelvic muscles, and enhance cardiovascular function. Stress relief and improved sleep quality are additional benefits. Activities may include household tasks, walking, light dancing, prenatal exercises, swimming, cycling, yoga, or Kegel exercises, based on personal preferences. However, activities such as jumping, high-impact sports, ball games, high-altitude activities (above 2,500 meters), long-distance travel, prolonged standing, diving, skiing, and horseback riding are not considered safe due to their associated risks.