Assessing fetal health includes identifying high-risk fetuses and monitoring the intrauterine condition of the fetus.
Identifying High-Risk Fetuses
High-risk fetuses include:
- Gestational age <37 weeks or ≥42 weeks
- Birth weight <2,500 g
- Small-for-gestational-age (SGA) or large-for-gestational-age (LGA) fetuses
- Apgar score of 0–3 within 1 minute after birth
- Intrapartum infections
- Neonates born to mothers with high-risk pregnancies
- Neonates delivered via surgical procedures
- Neonates with siblings who have a history of severe neonatal illness or neonatal death.
Monitoring the Intrauterine Condition of the Fetus
Early Pregnancy
Assessment of uterine size through gynecological examination to determine whether it corresponds to gestational age. Ultrasound can detect the gestational sac and primitive cardiac tube pulsation as early as the 6th week of gestation. If available, ultrasound at 11–13+6 weeks can measure nuchal translucency (NT) and evaluate fetal development.
Mid-Pregnancy
Fundal height measurements during every prenatal visit aid in assessing fetal size and whether it aligns with gestational age. Ultrasound is used to assess fetal growth and screen for structural anomalies. Fetal heart rate (FHR) is auscultated during each check-up.
Late Pregnancy
Fundal height measurements and auscultation of fetal heart rate during every prenatal visit. Ultrasound not only assesses fetal growth but also determines fetal position, placental location, amniotic fluid volume, and placental maturity.
Fetal Movement Monitoring
Monitoring fetal movements is a simple, economical, and effective method for pregnant women to self-evaluate the intrauterine condition of the fetus. Fetal movements are typically felt between 16–20 weeks of gestation and are more active during the afternoon and evening. Fetal movements may cease during the fetal sleep cycle, which lasts 20–40 minutes. After 28 weeks, fewer than 6 movements within two hours may indicate possible fetal hypoxia.
Electronic Fetal Monitoring (EFM)
EFM has become an important method for assessing fetal health. It continuously observes and records dynamic changes in FHR, as well as uterine contractions and fetal movements, reflecting the relationships among them. Evaluation criteria for EFM include baseline variability, which is considered the most important parameter.
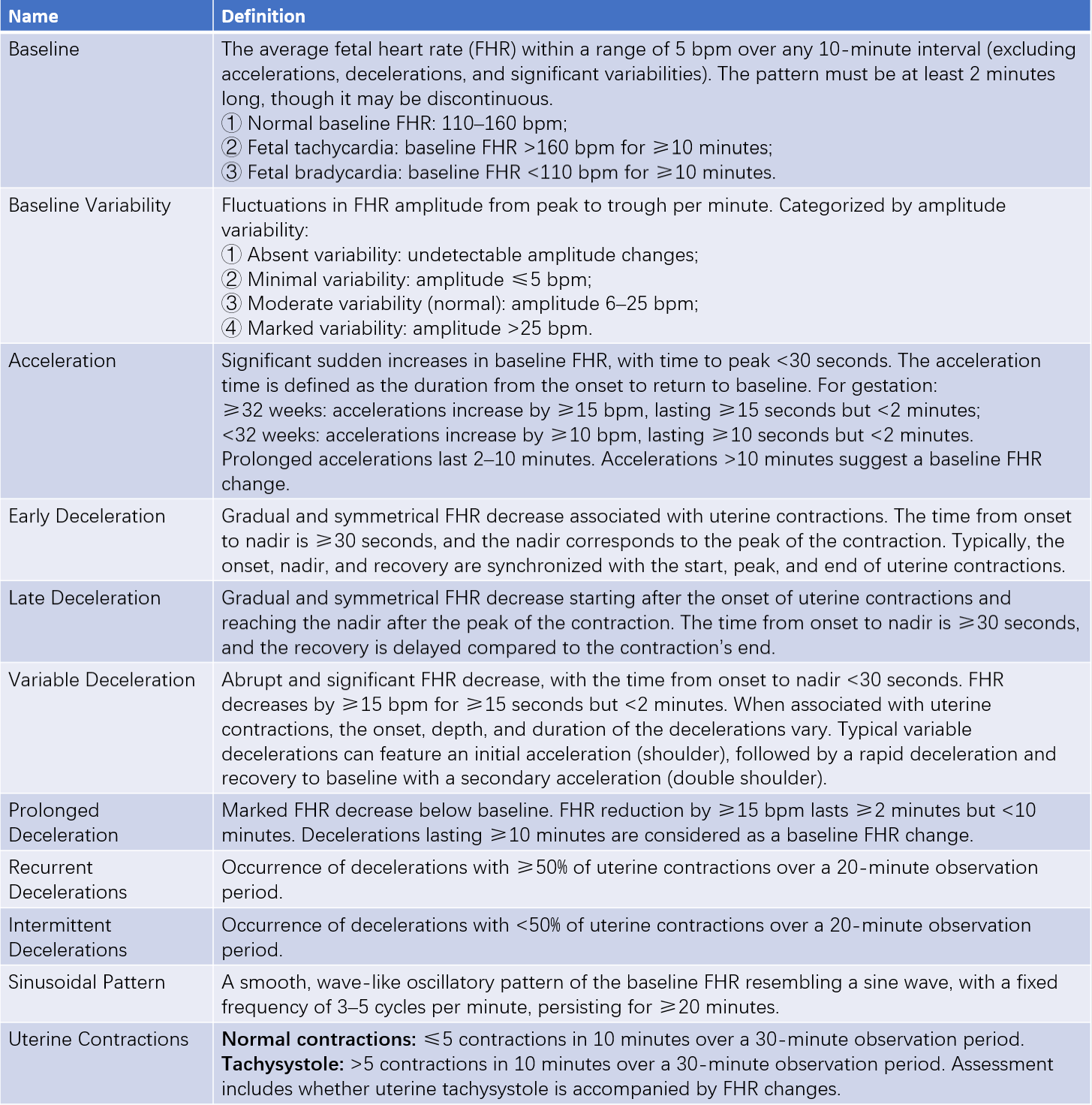
Table 1 Evaluation criteria for electronic fetal monitoring (EFM)
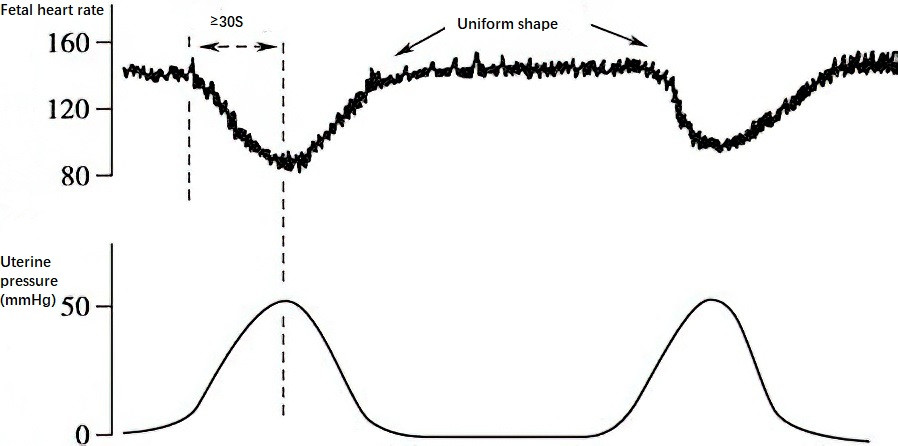
Figure 1 Early deceleration
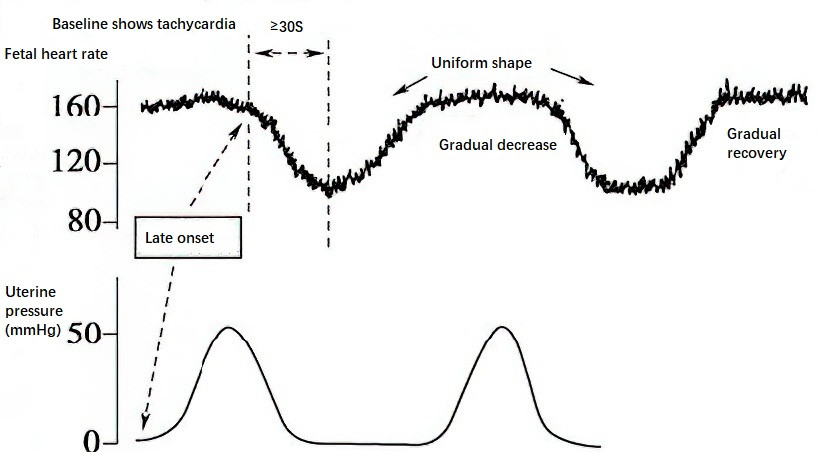
Figure 2 Late deceleration
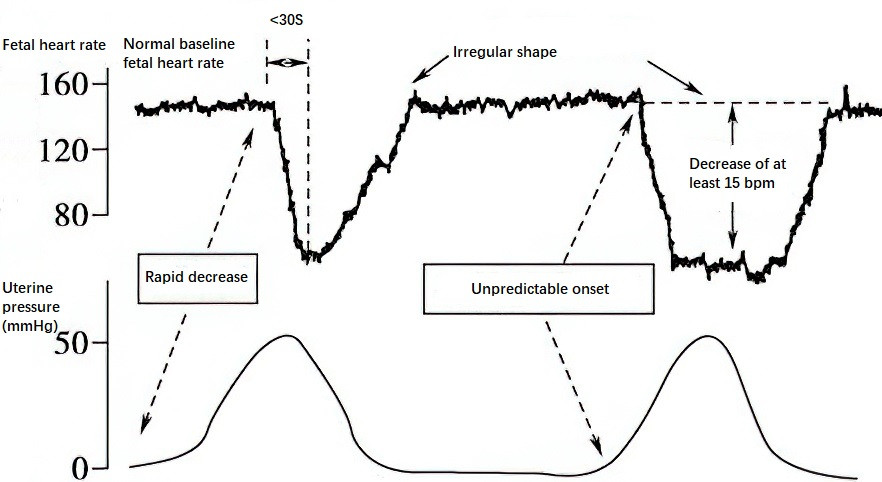
Figure 3 Variable deceleration
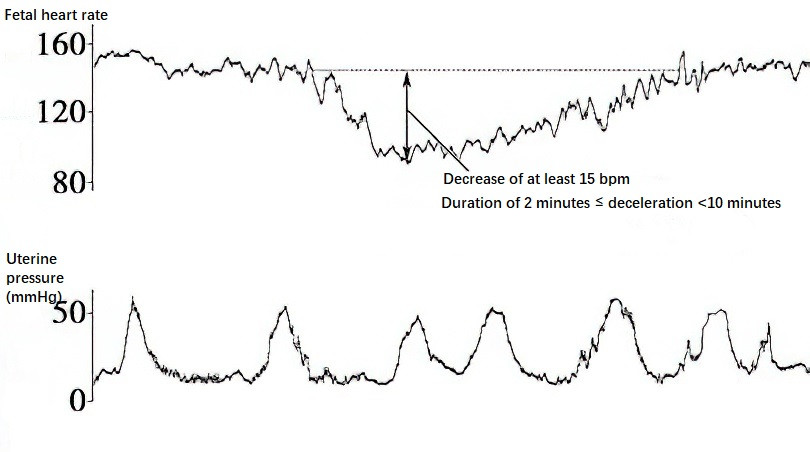
Figure 4 Prolonged deceleration
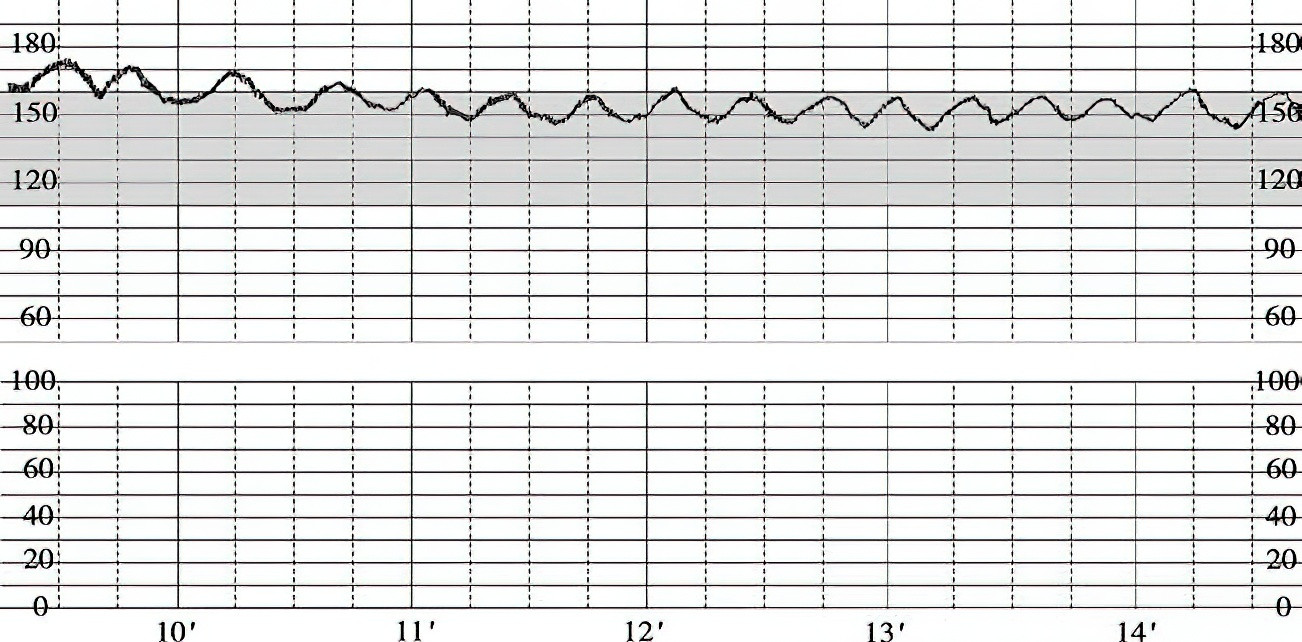
Figure 5 Sinusoidal pattern
Assessing Fetal Intrauterine Reserve Capacity
Non-Stress Test (NST) is used for prenatal monitoring.
Oxytocin Challenge Test (OCT) involves inducing uterine contractions with oxytocin and recording FHR changes using electronic fetal monitoring. OCT can aid in evaluating placental function both during prenatal monitoring and labor induction.
Interpretation of NST
Guidelines from the 2007 Society of Obstetricians and Gynaecologists of Canada (SOGC) are considered, noting the high rate of false positives. Abnormal NST results require retesting with extended monitoring time, and further evaluation using biophysical profiling when necessary.
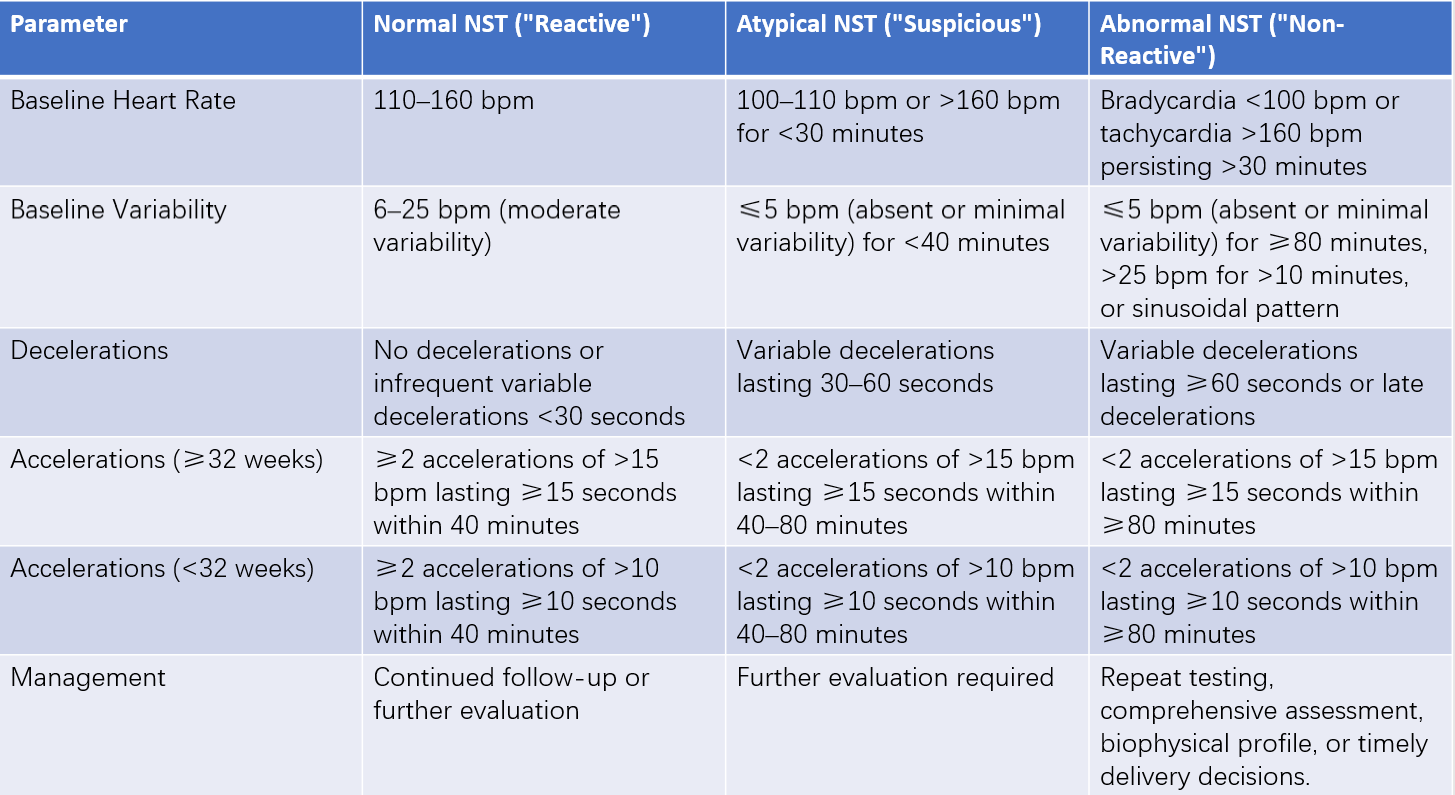
Table 2 NST interpretation and management
Interpretation of OCT
OCT results are primarily based on the presence of late decelerations or variable decelerations:
- Negative: No late decelerations or severe variable decelerations.
- Suspicious (any of the following): Intermittent late or severe variable decelerations, uterine hyperstimulation (>5 contractions in 10 minutes), decelerations lasting >90 seconds during contractions, or unexplained patterns.
- Positive: Late decelerations occur with ≥50% of contractions.
Interpretation of Intrapartum Fetal Monitoring Patterns
To avoid unnecessary intrapartum cesarean sections, the three-tier classification system for fetal monitoring patterns, recommended by the 2009 guidelines of the American College of Obstetricians and Gynecologists (ACOG), is generally used.
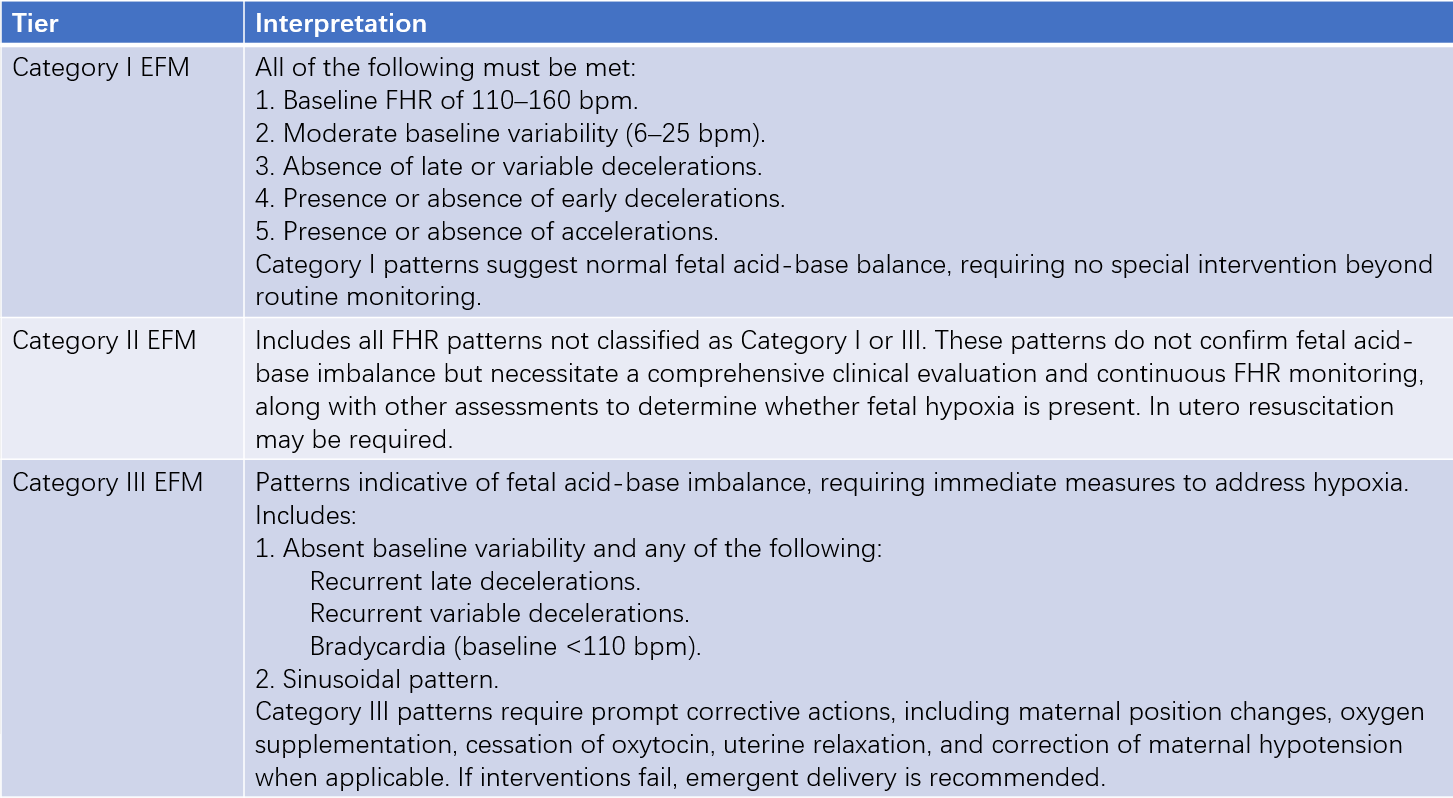
Table 3 Three-tier system for EFM interpretation
Fetal Biophysical Profile (BPP)
BPP integrates electronic fetal monitoring and ultrasound-assessed physiological activities to determine acute or chronic fetal hypoxia. Manning’s scoring method is commonly used, though its clinical application has declined due to its time intensity and susceptibility to subjective factors.
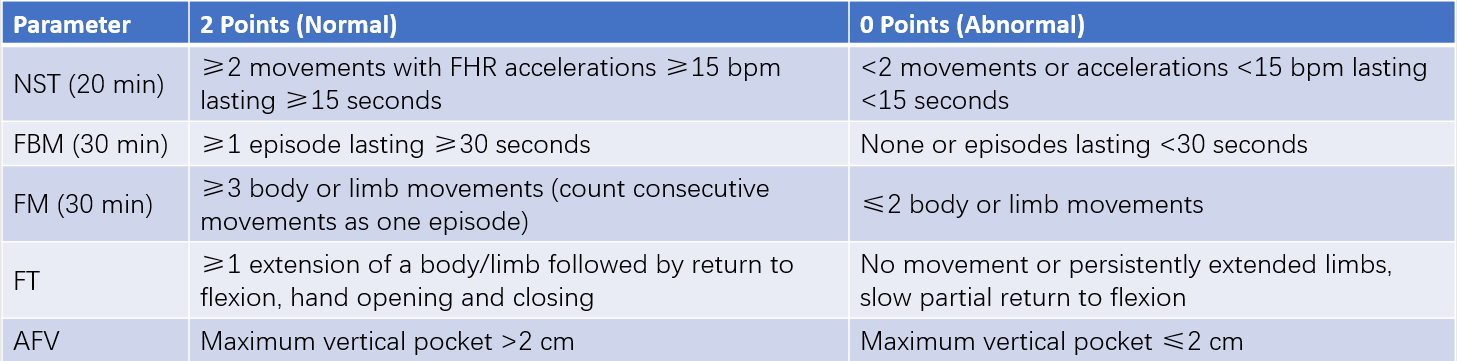
Table 4 Manning scoring method
Color Doppler Ultrasound for Fetal Blood Flow Monitoring
This technique evaluates fetal hemodynamics, offering an objective assessment of fetuses with high-risk factors. It assists in determining the optimal timing for pregnancy termination. Common indices include the S/D ratio (systolic/diastolic velocity ratio), resistance index (RI), pulsatility index (PI), and waveform analysis of the umbilical vein and ductus venosus. S/D is calculated as peak systolic flow velocity (S) divided by end-diastolic flow velocity (D), while RI is defined as (S-D)/S, and PI as (S-D)/mean velocity. Varying S/D, PI, and RI values correspond to different gestational weeks. Well-acknowledged criteria for detecting abnormal fetal blood flow include:
- Pulsatility index of the umbilical artery exceeding the 95th percentile for gestational age or more than two standard deviations above the mean, indicating potential fetal hypoxia.
- Absent or reversed end-diastolic flow in the umbilical artery, indicating severe fetal hypoxia.
- Decreased PI or S/D ratio of the fetal middle cerebral artery, suggesting fetal hypoxia.
- The presence of pulsation in the umbilical vein or ductus venosus a-wave reversal, indicating a critical condition in the fetus.