Standardized prenatal check-ups can help identify and manage pregnancy complications or comorbidities early, promptly detect fetal abnormalities, determine the timing and mode of delivery, and ensure maternal and fetal safety.
Timing, Frequency, and Gestational Weeks for Prenatal Check-Ups
Reasonable timing and frequency of prenatal check-ups not only enhance the quality of prenatal care but also optimize the use of healthcare resources. According to the World Health Organization (2016), for pregnant women without complications in developing countries, at least eight prenatal visits are recommended. These visits are scheduled for the following gestational weeks: less than 12 weeks, 20 weeks, 26 weeks, 30 weeks, 34 weeks, 36 weeks, 38 weeks, and 40 weeks. Currently, recommended prenatal check-up intervals are at gestational weeks 6–13, 14–19, 20–24, 25–28, 29–32, 33–36, and 37–41, with weekly visits from week 37 onwards. Additional visits may be needed for pregnancies with high-risk factors.
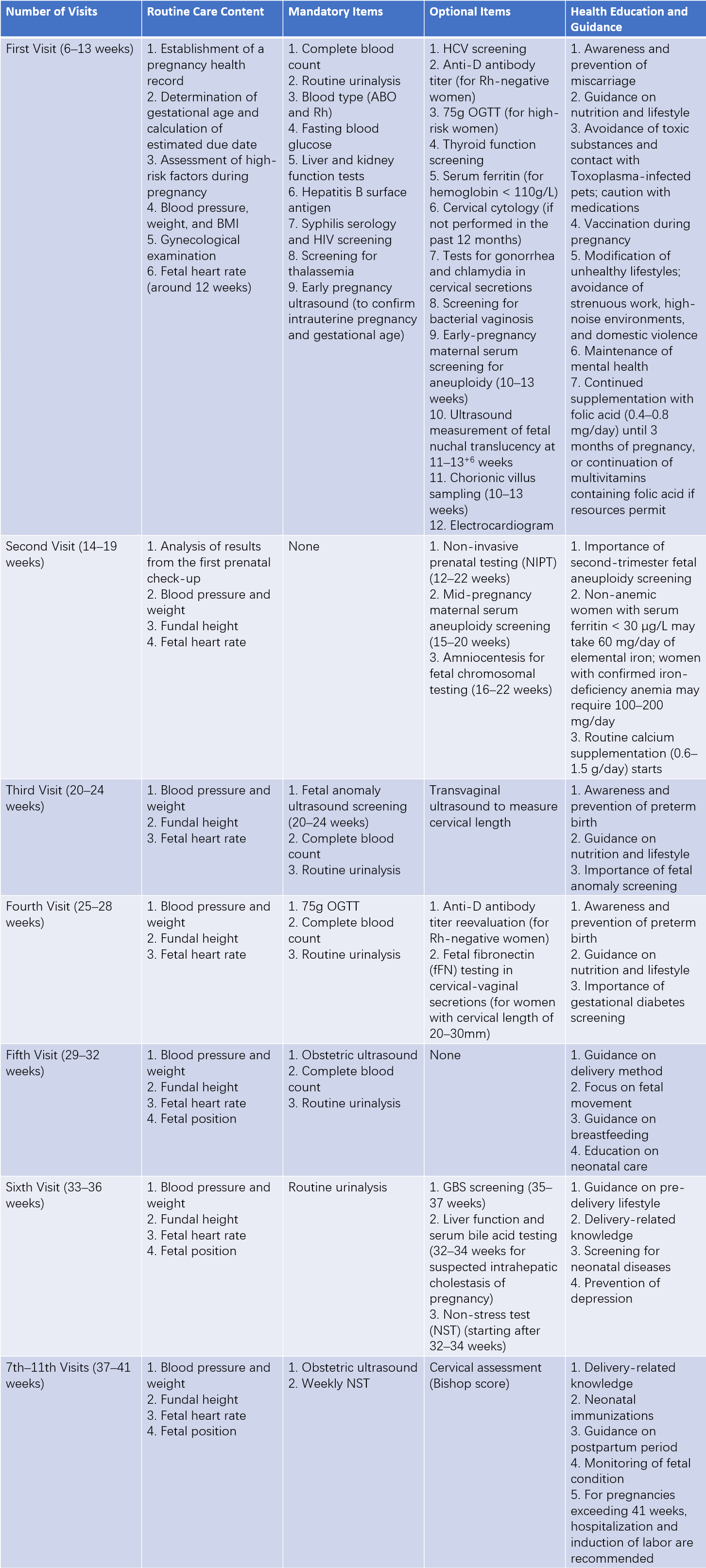
Table 1 Prenatal check-up schedule and content
Content of Prenatal Check-Ups
The check-up includes a detailed medical history, a comprehensive physical examination, specialized obstetric assessments, necessary complementary tests, and guidance on health education.
Medical History
Age
Pregnancies under 18 years or at 35 years and older are considered high-risk. Women aged 35 years and older are classified as advanced maternal age, and pregnancies at 40 years and older carry a significantly increased risk of maternal and fetal complications.
Occupation
Women engaged in occupations involving exposure to toxic substances or radiation face increased risks of adverse maternal and fetal outcomes. It is advised that such women consider changing jobs either before conception or upon becoming pregnant.
Course of Current Pregnancy
Information is gathered on whether early pregnancy symptoms, viral infections, or medication use occurred during the early stages of pregnancy. The onset and patterns of fetal movement, diet, sleep, and exercise habits, as well as symptoms such as vaginal bleeding, headaches, visual disturbances, palpitations, shortness of breath, or lower limb edema, are carefully documented.
Calculation and Confirmation of Expected Date of Confinement (EDC)
The EDC is calculated based on the first day of the last menstrual period (LMP). The formula involves adding 9 months or subtracting 3 months from the month of the LMP and then adding 7 days. For pregnancies achieved through assisted reproduction technology (ART), the LMP date can be back-calculated based on the date of embryo transfer, adjusted according to the stage of embryonic development, to determine the due date. Early pregnancy ultrasound results are used to confirm the EDC, particularly for women who are unsure of their LMP or conceive during breastfeeding amenorrhea. Before 14 weeks of gestation, crown-rump length (CRL) measurements are used to estimate gestational age. At 14 weeks and beyond, a composite assessment of biparietal diameter, head circumference, abdominal circumference, and femur length is conducted. Pregnancies where ultrasound confirmation of gestational age has not been performed by 22 weeks, and the gestational age is based solely on the LMP, are classified as suboptimally dated pregnancies. If the gestational age calculated from the LMP differs from early ultrasound findings by more than 5 days, the EDC is adjusted based on the ultrasound results.
Theoretically, earlier ultrasounds provide more accurate gestational age estimates. If multiple ultrasound results exist, the earliest measurement is used for determining the due date. However, considering potential measurement errors, current evidence suggests that fetal CRL measured during early pregnancy is the most accurate indicator for estimating gestational age.
Menstrual and Obstetric History
Questions focus on the age at menarche, menstrual cycle regularity, the number of pregnancies (gravidity) and deliveries (parity), as well as any history of miscarriages or uterine surgeries. Labor history, fetal outcomes (e.g., stillbirth), delivery methods, and neonatal health are also reviewed. Any complications or outcomes in previous pregnancies are documented.
Past and Surgical History
Information is collected on previous diagnoses and treatments for conditions such as hypertension, heart disease, tuberculosis, diabetes, hematologic disorders, liver or kidney diseases, and autoimmune diseases, as well as any previous surgeries.
Family History
Questions focus on family history of tuberculosis, hypertension, diabetes, twin pregnancies, or other hereditary conditions.
Husband’s Health Status
The husband’s age, general health, and presence of hereditary disorders are also assessed.
Physical Examination
Observations include the woman's physical development, nutritional status, and mental state. Particular attention is paid to gait and height, as women shorter than 145 cm are more likely to have a narrow pelvis. Examinations cover potential heart conditions, spinal or lower limb deformities, breast condition, and signs of edema. Blood pressure, weight, and height are measured, and the body mass index (BMI) is calculated. The BMI is determined using the formula: BMI = weight (kg) / height (m2). The presence or absence of edema is also noted.
Obstetric Examination
Obstetric examination includes abdominal examination, pelvic measurement, and vaginal examination.
Abdominal Examination
This examination is performed with the pregnant woman lying on her back after emptying her bladder. The head is slightly elevated, the abdomen is exposed, and the legs are slightly bent and apart to allow abdominal muscles to relax. The examiner stands on the right side of the patient during the examination.
Inspection
Observations include the shape and size of the abdomen, the presence of striae gravidarum (stretch marks), surgical scars, or edema. If the abdomen is hanging downward (pendulous abdomen), there is a need to consider the possibility of a narrow pelvis.
Palpation
During mid to late pregnancy, Leopold's maneuvers (four maneuvers) are used to assess uterine size, fetal lie, fetal presentation, fetal position, and whether the presenting part has engaged. For the first three maneuvers, the examiner faces the mother's head, while the fourth maneuver is performed with the examiner facing the mother's feet. A soft tape measure may be used to measure uterine height (distance from the upper edge of the pubic symphysis to the fundus). Abnormal uterine height warrants further investigation, such as re-verification of the expected date of confinement (EDC) or ultrasound assessment.
- First Maneuver: Both hands are placed on the fundus of the uterus to evaluate its shape and height. The estimated fetal size is checked against gestational age. The examiner uses the fingertips to lightly press on the fundus to identify the part of the fetus located there: the fetal head is firm, rounded, and mobile, while the fetal buttocks are soft, wide, and irregular in shape.
- Second Maneuver: Each hand is placed on one side of the mother's abdomen. One hand remains stationary while the other palpates deeply. A smooth and firm surface indicates the fetal back, whereas uneven, movable parts indicate the fetal limbs, which may sometimes feel like active fetal movements.
- Third Maneuver: The examiner separates their right thumb from the other four fingers and places them above the pubic symphysis to grasp the presenting part. This determines whether the presenting part is the fetal head or breech, and whether it has engaged by gently attempting to move it side to side. If the presenting part remains mobile, it has not engaged. If it is immobile, engagement is confirmed.
- Fourth Maneuver: With hands placed on either side of the presenting part, the examiner pushes downward toward the pelvic inlet to confirm the accuracy of the presenting part as previously assessed and to determine the degree of engagement.
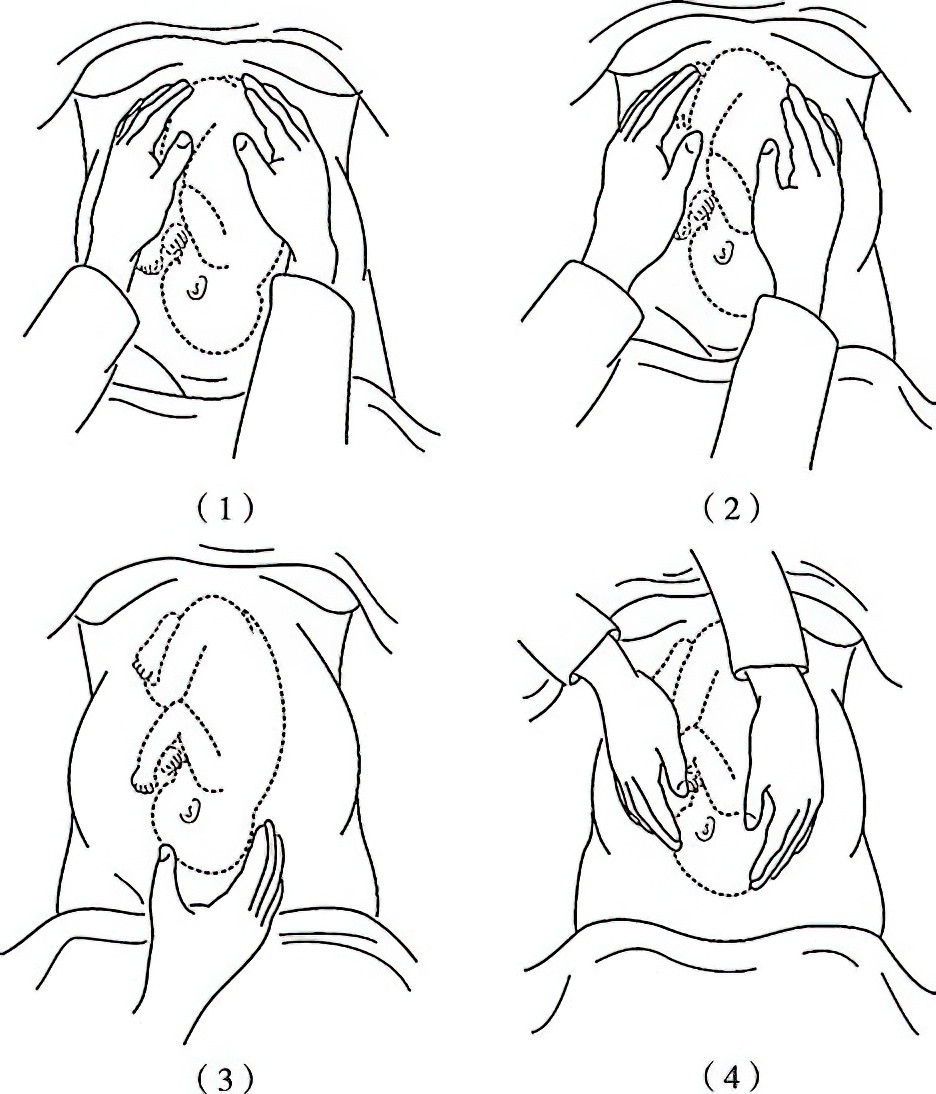
Figure 1 Four-step palpation method for fetal position examination
Auscultation
Fetal heart sounds are most distinctly heard on the mother's abdominal wall closest to the fetal back. In vertex presentations, the fetal heart is heard below the umbilicus on the right or left; in breech presentations, it is heard above the umbilicus on the right or left. For shoulder presentations, the fetal heart sound is clearest near the lower part of the umbilicus.
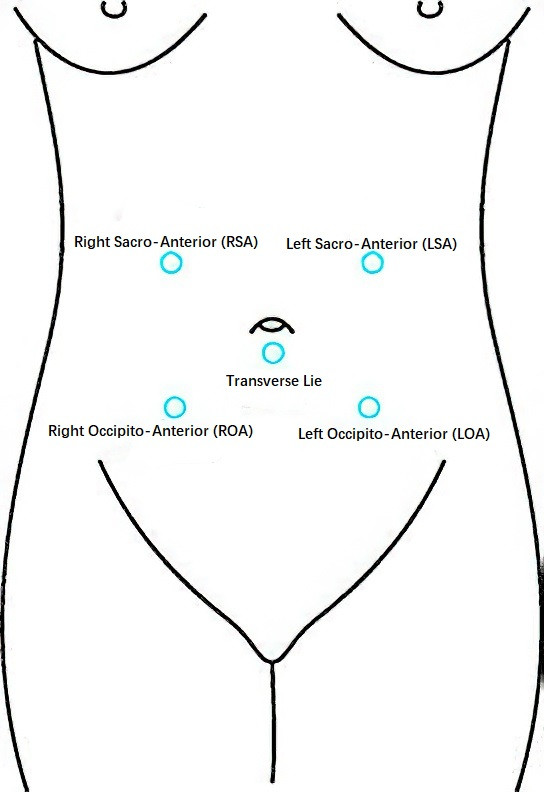
Figure 2 Locations for auscultation of fetal heart sounds in different fetal positions
Pelvic Measurement
Internal Pelvimetry
To assess the maternal bony pelvis and determine its condition for vaginal delivery, internal pelvic measurement may be performed either antenatally or during labor.
Diagonal Conjugate (DC)
This is the distance from the lower edge of the pubic symphysis to the midpoint of the sacral promontory. The normal value is 12.5–13.0 cm, and subtracting 1.5–2.0 cm from this gives the true conjugate (conjugate vera), which represents the anteroposterior diameter of the pelvic inlet. The examiner inserts the index and middle fingers of one hand into the vagina, with the middle fingertip touching the midpoint of the sacral promontory and the upper edge of the index finger against the lower edge of the pubic symphysis. The other hand marks this contact point externally. After removing the fingers from the vagina, the distance between the tip of the middle finger and the marked point is measured to determine the diagonal conjugate.
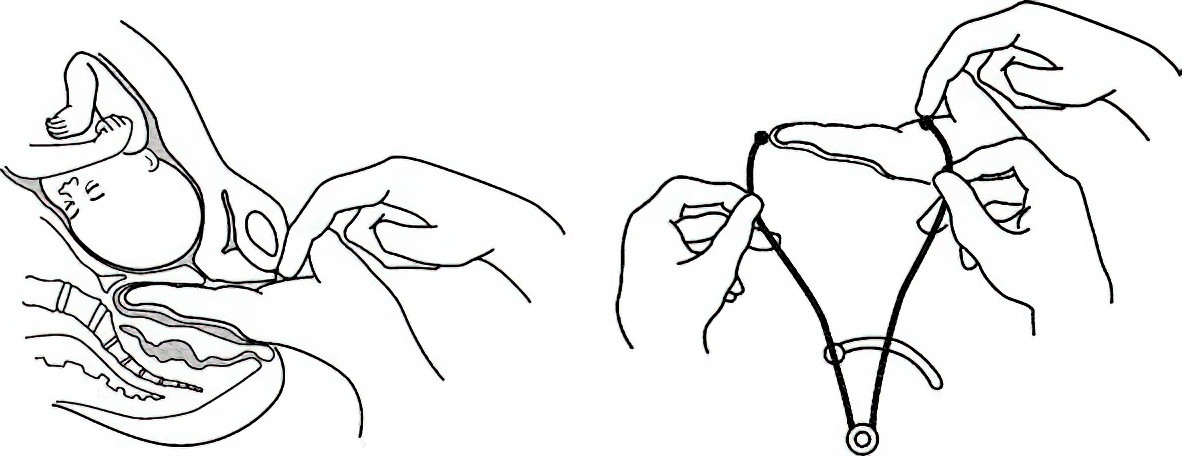
Figure 3 Measurement of the diagonal conjugate
Interspinous Diameter
This is the distance between the ischial spines, which is normally about 10 cm. The examiner places the index and middle fingers into the vagina and palpates the ischial spines on both sides to estimate the distance.
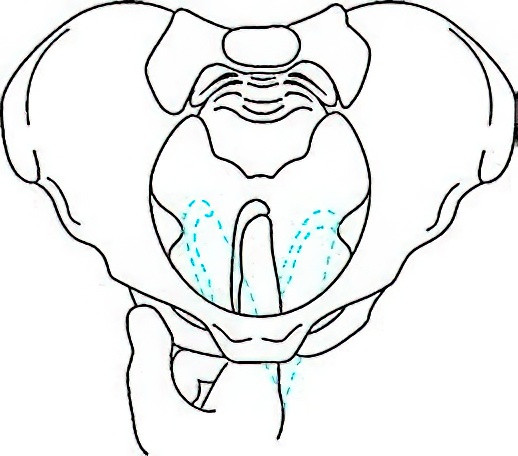
Figure 4 Measurement of the interspinous diameter
Ischial Notch Width
Representing the posterior sagittal diameter of the midpelvis, this is the width between the ischial spines and the lower part of the sacrum, corresponding to the width of the sacrospinous ligament. If three transverse fingers (5.5–6.0 cm) can be accommodated on the ligament during vaginal palpation, it is considered normal. Otherwise, midpelvic constriction is indicated.
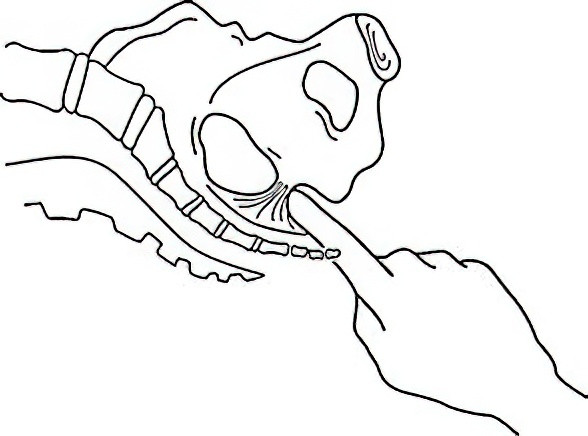
Figure 5 Measurement of the width of the ischial notch
Posterior Sagittal Diameter of Outlet
This is the distance from the midpoint of the intertuberous diameter to the sacral tip. The examiner inserts the gloved index finger of the right hand into the anus pointing toward the sacrum, while the thumb is placed externally over the sacrococcygeal region. Together, both fingers identify the sacral tip. Next, the pelvic outlet measuring device is used, with one end placed at the midpoint of the intertuberous diameter and the other at the sacral tip. The marking on the measuring device indicates the posterior sagittal diameter of the outlet, with a normal value being 8–9 cm.
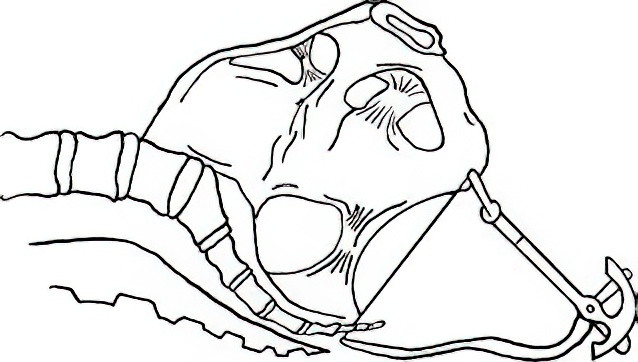
Figure 6 Measurement of the posterior sagittal diameter of the pelvic outlet
External Pelvic Measurement
External pelvic measurements include assessments of the interspinous diameter (normal range: 23–26 cm), the intercristal diameter (normal range: 25–28 cm), the external conjugate diameter (normal range: 18–20 cm), and the intertuberous diameter, also known as the transverse outlet diameter (TO). There is sufficient evidence indicating that measurements of the interspinous diameter, intercristal diameter, and external conjugate diameter do not effectively predict cephalopelvic disproportion during labor, and performing these measurements is therefore unnecessary. When pelvic outlet narrowing is suspected, measurements of the intertuberous diameter and the angle of the pubic arch may be performed.
Measurement Method for the Intertuberous Diameter
The pregnant woman is positioned supine with knees bent, and both hands clasping the knees. The distance between the inner edges of the ischial tuberosities is measured, with normal values ranging from 8.5 to 9.5 cm. When the sum of the posterior sagittal diameter of the outlet and the intertuberous diameter exceeds 15 cm, significant narrowing of the pelvic outlet is unlikely.
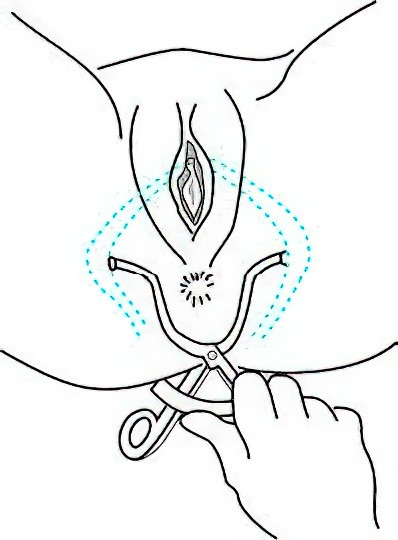
Figure 7 Measurement of the intertuberous diameter
Measurement Method for the Angle of the Pubic Arch
The examiner aligns the tips of both thumbs diagonally and places them below the lower edge of the pubic symphysis, with the thumbs resting flat on the descending rami of the pubic bones. The angle formed between the thumbs determines the angle of the pubic arch. A normal angle is approximately 90°, while values below 80° are considered abnormal. This angle reflects the width of the transverse diameter of the pelvic outlet.
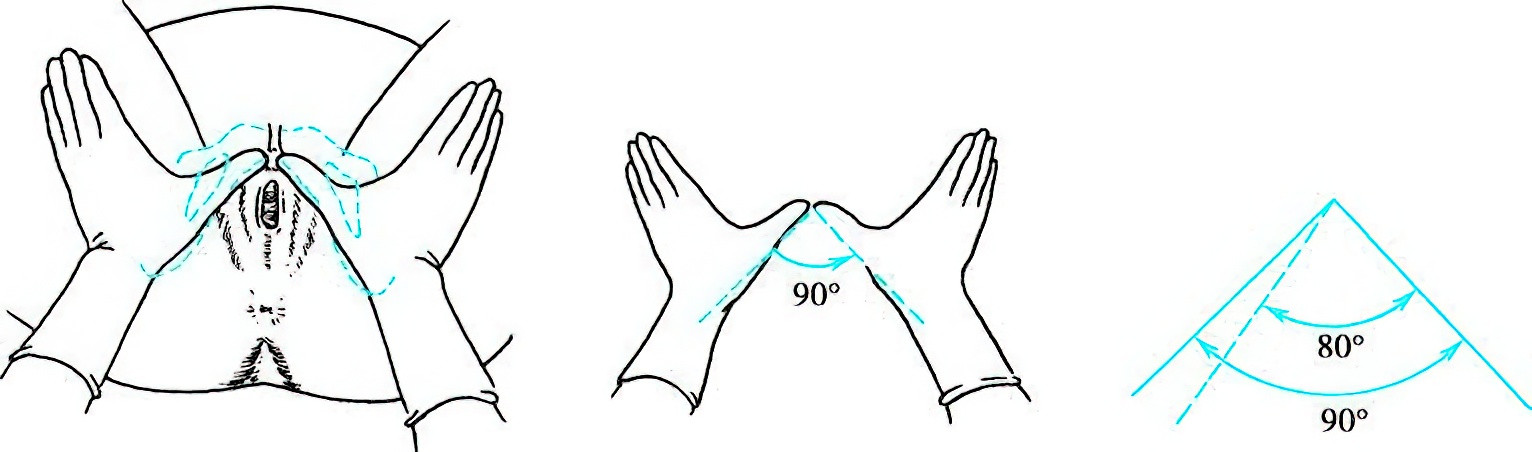
Figure 8 Measurement of the angle of the pubic arch
Vaginal Examination
Vaginal examination may be performed during pregnancy, particularly in cases of abnormal vaginal bleeding or unusual vaginal discharge. Vaginal examinations before labor can help determine pelvic dimensions, cervical effacement, and the degree of cervical dilation, as well as allow for a Bishop score assessment of the cervix.
Auxiliary Examinations and Health Education
Each prenatal check-up includes corresponding auxiliary tests and recommendations for pregnancy care based on the gestational week. Prenatal check-ups involve routine care, auxiliary examinations (divided into mandatory and optional items), and health education and guidance. The routine care components, health education, and mandatory testing apply to all pregnant women. Optional items may be conducted in hospitals with the necessary resources, or when specific indications are present.
Prenatal Care for Advanced Maternal Age
Pregnancy risks increase with advanced maternal age, including higher incidences of miscarriage, fetal chromosomal and structural abnormalities, gestational hypertensive disorders, gestational diabetes, fetal growth restriction (FGR), preterm birth, and stillbirth. Detailed counseling and assessment are conducted based on specific age factors and high-risk conditions.
Folic acid or multivitamins containing folic acid are supplemented in a standardized manner. Calcium and iron supplementation is provided promptly and appropriately, with possible increases in dosage based on individual needs. For those with indications, low-dose aspirin may be prescribed to prevent preeclampsia. Women of advanced maternal age are prioritized for prenatal screening and diagnosis.
For women aged between 35 and 39 years where age is the sole risk factor, non-invasive prenatal screening (NIPS) for fetal aneuploidy may be offered after informed consent is obtained. For women aged 40 and above at the expected date of confinement, invasive prenatal diagnostic procedures are recommended to rule out fetal aneuploidy.
Fetal structural abnormalities and FGR, as well as gestational diabetes and gestational hypertensive disorders, are areas of focus for screening. For women aged 40 and above, enhanced fetal monitoring is recommended, and pregnancy termination before 40 weeks of gestation is advised as appropriate.