Mid-to-late pregnancy is a critical period for fetal growth and the maturation of various organs. The primary focus during this stage includes evaluating fetal development, assessing intrauterine conditions, and identifying fetal anomalies in a timely manner.
Medical History and Symptoms
A history of early pregnancy is typically present. Individuals may notice progressive abdominal enlargement and perceive fetal movements.
Signs and Examinations
Uterine Enlargement
An enlarged uterus can be observed during abdominal examinations. The height of the uterine fundus or the length of the uterus above the symphysis pubis (measured manually or with a ruler) provides an estimate of fetal size and gestational age. Uterine fundal height varies depending on the distance between the umbilicus and symphysis, fetal growth, amniotic fluid volume, and whether it is a singleton or multiple pregnancy. The rate of uterine growth differs across gestational weeks. Between 20 and 24 weeks, the fundus grows rapidly, with an average increase of 1.6 cm per week. From 36 to 40 weeks, growth slows to an average of 0.25 cm per week. Normally, the uterine height reaches its peak at 36 weeks and slightly decreases at term due to fetal descent into the pelvis.
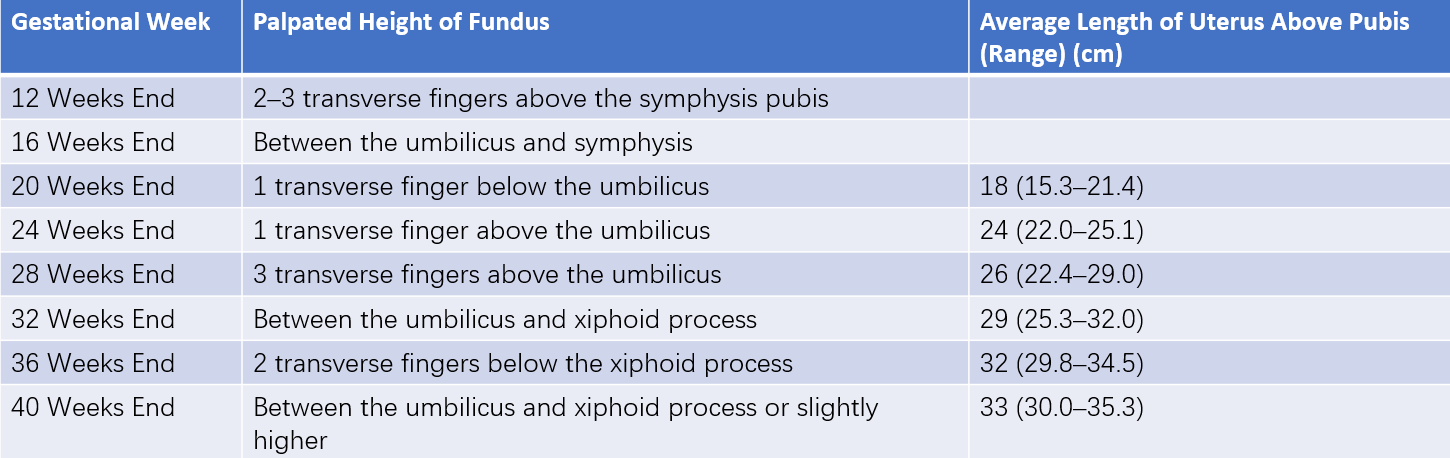
Table 1 Uterine height and length at different gestational ages
Fetal Movement (FM)
Fetal movement refers to the physical activities of the fetus. Individuals often begin perceiving fetal movements between 16 and 20 weeks of gestation. Movements become progressively stronger as pregnancy advances, peaking at 32–34 weeks. After 38 weeks, they gradually decrease. After 28 weeks, normal fetal movement generally occurs at least three times per hour or ten times over two hours. Fetal movements may also be observed or palpated during abdominal examinations.
Fetal Body Parts
After 20 weeks of gestation, fetal body parts can be palpated through the abdominal wall. From 24 weeks onward, fetal structures such as the head, back, buttocks, and limbs become distinguishable during palpation. The fetal head is round and firm, with a ballottable sensation; the back is broad and flat; the buttocks are wide and soft with irregular shapes; and limbs are small with irregular movements. As pregnancy progresses, Leopold’s maneuvers can be used to determine the fetal position within the uterus.
Fetal Heart Sounds
The detection of fetal heart sounds confirms pregnancy and indicates fetal viability. Fetal heart sounds can be detected using a Doppler fetal monitor as early as 12 weeks of gestation and with a standard stethoscope through the abdominal wall from 18 to 20 weeks. Fetal heart tones are characterized by a dual-sound rhythm resembling a "tick-tock," with a relatively fast rate. The normal fetal heart rate ranges between 110 and 160 beats per minute. Fetal heart sounds need to be differentiated from uterine bruits, abdominal aortic sounds, and umbilical cord murmurs.
Auxiliary Examinations
Ultrasound Examination
Ultrasound provides insights into fetal characteristics, including the number of fetuses, fetal presentation, fetal lie, detection of fetal heart activity, placental location (and its relation to the internal cervical os), and amniotic fluid volume. Measurements of fetal biometric parameters, such as biparietal diameter, head circumference, abdominal circumference, and femur length, can estimate fetal weight and monitor fetal growth and development. Between 20 and 24 weeks, ultrasound can be used for a detailed fetal anatomical survey to screen for structural abnormalities.
Color Doppler Ultrasound
Color Doppler ultrasound assesses blood flow velocity waveforms in the uterine arteries, umbilical arteries, and fetal vessels. In late pregnancy, the pulsation index (PI) and resistance index (RI) of the umbilical artery can evaluate placental vascular resistance and fetal blood supply. The peak systolic velocity (PSV) of the middle cerebral artery (MCA) is a parameter for assessing the severity of fetal anemia.