The female reproductive organs are anatomically adjacent to the urethra, bladder, ureters, rectum, and appendix. Pathological changes in the female reproductive organs often affect neighboring structures, complicating diagnosis and treatment. Since the female reproductive system and the urinary system share a common embryological origin, abnormalities in the development of the female reproductive organs may coincide with anomalies in the urinary system.
Urethra
The urethra is a muscular tube that begins at the tip of the trigone of the bladder, passes through the urogenital diaphragm, and opens externally at the external urethral orifice in the vaginal vestibule. It measures 4–5 cm in length and approximately 0.6 cm in diameter and is composed of two layers: an inner mucosal layer and an outer muscular layer. The mucosa lines the lumen and is continuous with the bladder mucosa. The muscular layer is further divided into two parts: the inner layer consists of longitudinal smooth muscle, which shortens and widens the urethral lumen during urination, while the outer layer consists of striated muscle, forming the urethral sphincter. This sphincter, composed of "slow-twitch" muscle fibers, sustains prolonged contractions to maintain urethral closure. Rapid urethral closure is aided by contractions of the surrounding levator ani muscle. The levator ani muscle and pelvic fascia provide support to the urethra, offering resistance to maintain closure during increased intra-abdominal pressure. Damage to these structures can result in stress urinary incontinence. Because the female urethra is short, straight, and in close proximity to the vagina, it is more susceptible to urinary tract infections.
Urinary Bladder
The bladder is a sac-like muscular organ. When empty, it lies between the pubic symphysis and the uterus, while a distended bladder can extend upward into the pelvic or even abdominal cavity. The average adult bladder capacity is 350–500 ml. The bladder is divided into four parts: apex, base, body, and neck. The apex of the bladder is covered by the peritoneum, which transitions posteriorly to cover the anterior wall of the uterus, forming the vesicouterine pouch. The inner surface of the bladder base contains a triangular area known as the trigone. The trigone's apex points downward to the internal urethral orifice, while the base is bounded by the openings of the ureters on either side, forming an equilateral triangle with a side length of approximately 2.5 cm when the bladder contracts. The base of the bladder lies adjacent to the cervix and the anterior vaginal wall, with loose intervening connective tissue. When the pelvic floor muscles and fascia are damaged, the bladder and urethra may descend along with the cervix and the anterior vaginal wall, potentially resulting in prolapse.
Ureters
The ureters are a pair of cylindrical muscular tubes with walls approximately 1 mm thick. They are composed of a mucosal layer, a muscular layer, and an outer adventitia. Each ureter is about 30 cm long and varies in diameter, with an internal diameter of 3–4 mm at its narrowest and 7–8 mm at its widest. The ureters originate from the renal pelvis and descend retroperitoneally along the anterior surface of the psoas major muscle toward the midline (lumbar segment). At the level of the sacroiliac joint, the ureters cross anteriorly to the origins of the external iliac arteries and enter the pelvic cavity (pelvic segment). Retroperitoneally, the ureters continue descending alongside the internal iliac arteries, reaching the base of the broad ligament where they pass medially beneath the uterine arteries, approximately 1.5–2.0 cm lateral to the internal cervical os. The ureters then traverse the ureteric tunnels obliquely before entering the bladder.
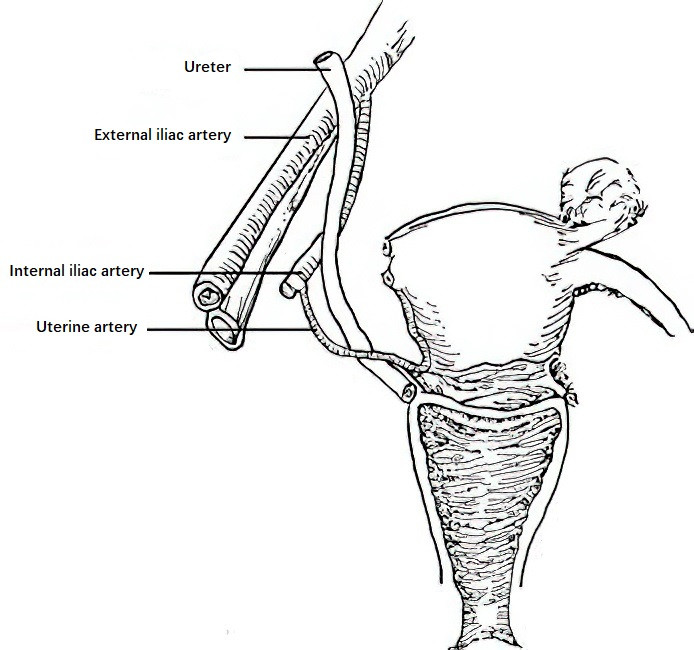
Figure 1 Relationship between the ureter and the uterine artery
During procedures such as ovarian vessel ligation, uterine artery ligation, or opening of the ureteric tunnels, care must be taken to avoid ureteral injury. Throughout their course, the blood supply to the ureters is provided by anastomosing branches from arteries servicing the kidneys, ovaries, uterus, and bladder. These anastomoses form vascular networks around the ureters. Ureteral blood supply must be protected during pelvic surgeries to prevent ischemia-induced ureteral fistulas.
Rectum
The rectum is located in the posterior part of the pelvic cavity, connecting superiorly to the sigmoid colon and inferiorly to the anal canal. Anterior to the rectum lie the uterus and vagina, while posteriorly it is adjacent to the sacrum. The rectum measures 10–14 cm in length. Its anterior wall is closely apposed to the posterior wall of the vagina, and damage to the pelvic floor muscles and fascia frequently causes the rectum and the posterior vaginal wall to prolapse together. The anal canal, measuring 2–3 cm in length, is separated from the lower vaginal segment by the perineal body. During vaginal delivery, care must be taken to protect the perineum and prevent injury to the anal canal.
Vermiform Appendix
The vermiform appendix is a blind tubular structure attached to the medial wall of the cecum, resembling an earthworm in shape. Its exact position, length, and thickness vary significantly, but it is commonly found in the right iliac fossa. In some cases, the lower end of the appendix may extend as far as the region of the right fallopian tube and ovary. In female patients with appendicitis, the condition may affect the right adnexa and uterus, necessitating differential diagnosis. During pregnancy, the enlarging uterus may push the appendix upward and outward, potentially leading to delayed diagnosis.