The blood vessels and lymphatic vessels of the female reproductive system run alongside each other, with the veins and lymphatic vessels connecting through plexuses and networks between the various organs.
Arteries
The blood supply to the internal and external female reproductive organs primarily originates from the ovarian artery, uterine artery, vaginal artery, and internal pudendal artery.
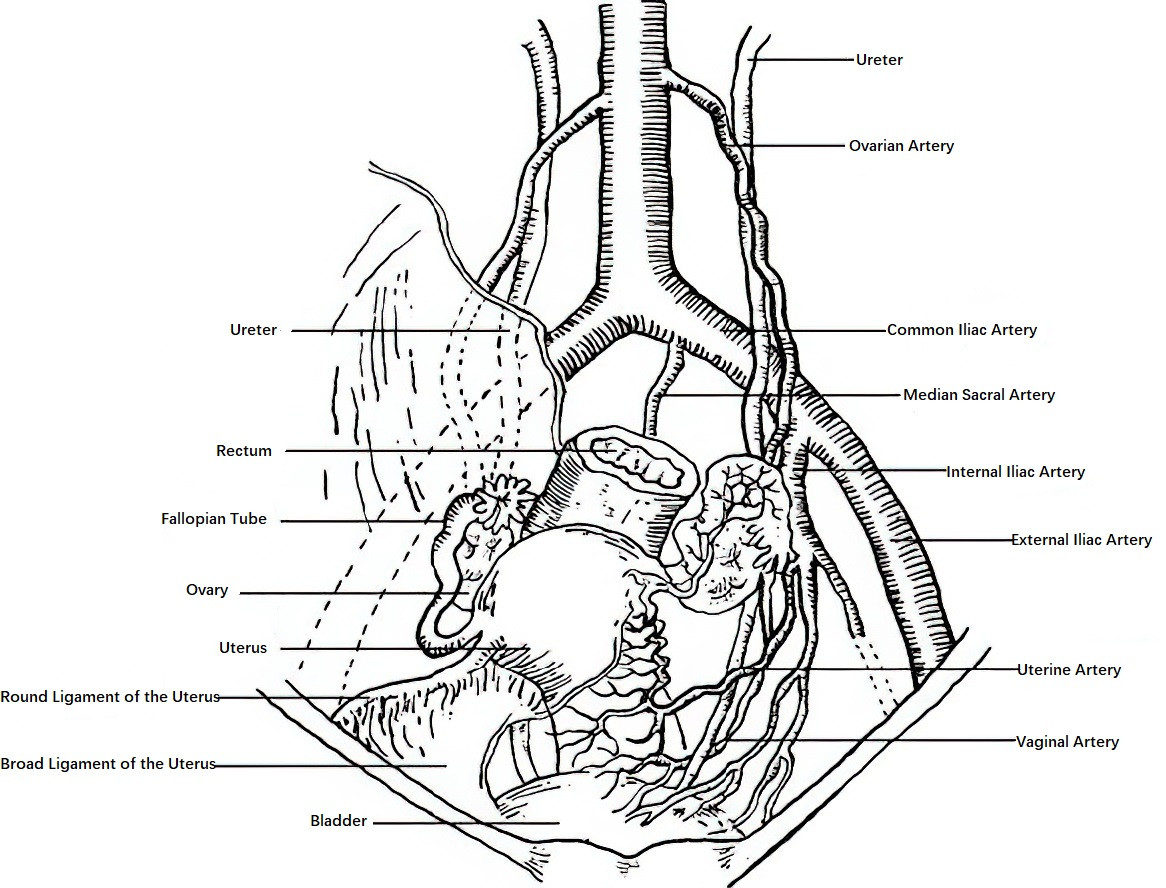
Figure 1 Arteries of the female pelvis
Ovarian Artery
The ovarian artery arises from the abdominal aorta and descends retroperitoneally along the psoas major muscle to the pelvic brim. It then crosses the ureter and the lower segment of the common iliac artery, traverses medially via the infundibulopelvic ligament, and passes posteriorly through the mesovarium to enter the ovary via the ovarian hilum. Before entering the ovary, branches of the ovarian artery travel within the mesosalpinx to supply the fallopian tubes, with distal branches anastomosing near the uterine cornua with the ovarian branches of the ascending portion of the uterine artery.
Uterine Artery
The uterine artery is a branch of the anterior trunk of the internal iliac artery. It descends anteriorly and medially along the pelvic sidewall in the retroperitoneal space, crossing the base of the broad ligament and the parametrium to reach the lateral side of the uterus. At approximately 1.5–2 cm lateral to the uterine cervix at the level of the internal cervical os, it crosses the ureter to reach the side of the uterus. It then divides into two branches:
- The superior branch, which is larger, travels tortuously along the body of the uterus and is known as the uterine body branch. This branch gives rise to 8–11 arcuate arteries along its path and further divides near the uterine cornua into the uterine fundus branch, tubal branch, and ovarian branch.
- The inferior branch, which is smaller, supplies the cervix and the upper portion of the vagina and is referred to as the cervicovaginal branch.
Vaginal Artery
The vaginal artery is a branch of the anterior trunk of the internal iliac artery. It supplies the middle and lower portions of the vaginal anterior and posterior walls, as well as the bladder dome and bladder neck. It anastomoses with the cervicovaginal branch of the uterine artery and branches of the internal pudendal artery. The upper segment of the vagina is supplied by the cervicovaginal branch of the uterine artery, the middle segment by the vaginal artery, and the lower segment primarily by the internal pudendal artery and the middle rectal artery.
Internal Pudendal Artery
The internal pudendal artery is a branch of the anterior trunk of the internal iliac artery. It exits the pelvic cavity via the greater sciatic foramen, passing below the piriformis muscle, and loops around the ischial spine. It then reenters through the lesser sciatic foramen and reaches the ischioanal fossa, where it gives rise to branches such as the inferior rectal artery, perineal artery, and dorsal artery of the clitoris, supplying the anus, perineum, and external genitalia.
Veins
The pelvic veins generally accompany the arteries of the same name, but they are more numerous. They form venous plexuses within and around the corresponding organs and connect to each other. The ovarian veins follow the ovarian artery and drain into the inferior vena cava on the right side and into the left renal vein at a right angle on the left side. This arrangement increases the likelihood of venous reflux obstruction, making left-sided pelvic varices more common.
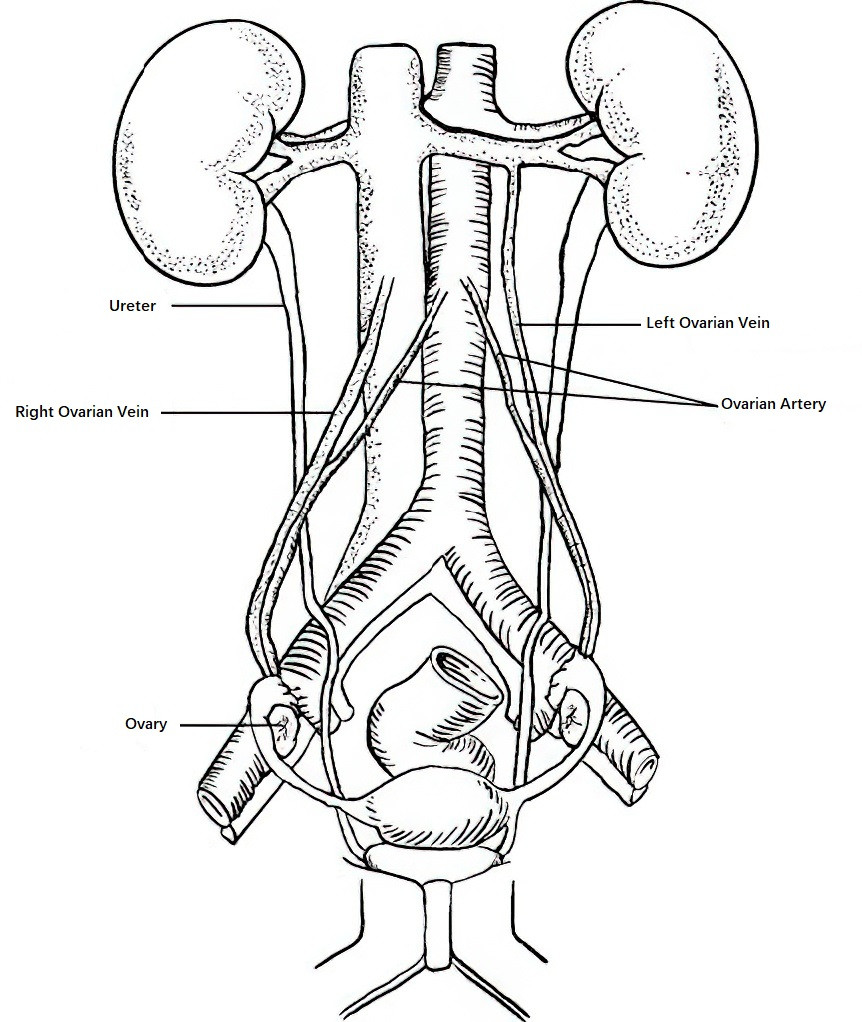
Figure 2 Schematic diagram of ovarian venous drainage
Lymphatics
The female reproductive organs and pelvic tissues have an extensive lymphatic system. Lymph nodes are typically aligned with corresponding blood vessels and distributed in clusters, with considerable variation in number and precise location. During infections or malignancies of the internal or external reproductive organs, lymphatic vessels frequently serve as pathways for the spread or metastasis. The lymphatic drainage of the female reproductive organs is divided into two groups: lymphatics of the external genitalia and lymphatics of the internal genitalia.
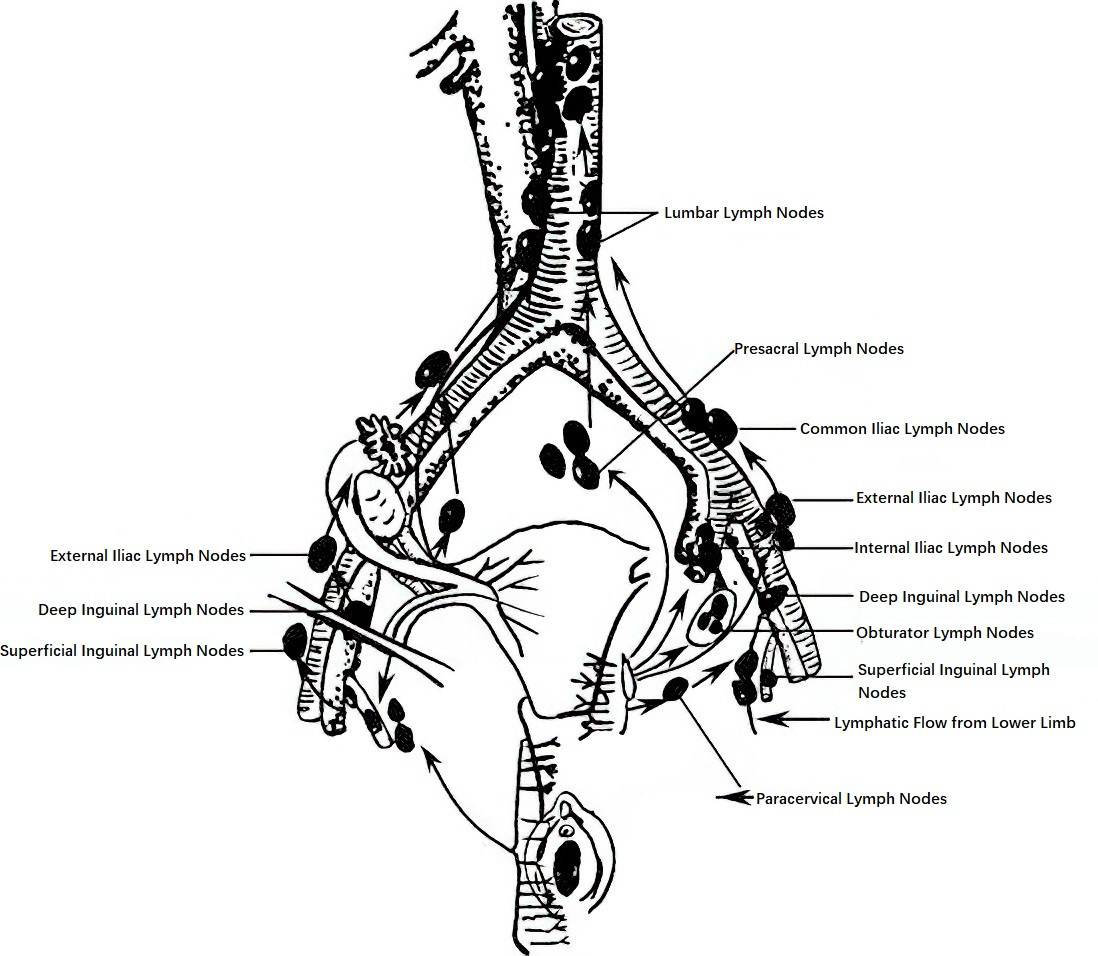
Figure 3 Lymphatic drainage of the female reproductive system
Lymphatic Drainage of the External Genitalia
This is divided into superficial and deep components:
- Superficial Inguinal Lymph Nodes: Positioned in two distinct groups, the upper group is aligned along the inguinal ligament and receives lymph from the external genitalia, lower vagina, perineum, and anal region. The lower group surrounds the terminal portion of the great saphenous vein and receives lymph from the perineum and lower limbs. Most efferent lymphatic vessels drain into the deep inguinal lymph nodes, with a smaller portion flowing into the external iliac lymph nodes.
- Deep Inguinal Lymph Nodes: Located medial to the femoral vein, these nodes receive lymph from the clitoris and superficial inguinal lymph nodes and drain into the external iliac lymph nodes or obturator lymph nodes.
Lymphatic Drainage of the Internal Genitalia
This drainage is categorized into three groups:
- Iliac Group: Composed of obturator, internal iliac, external iliac, and common iliac lymph nodes.
- Presacral Group: Situated on the anterior surface of the sacrum.
- Lumbar Group: Also referred to as the para-aortic lymph nodes, located along the sides of the abdominal aorta.
The lymph from the lower vagina primarily drains into the superficial inguinal lymph nodes. The lymphatic drainage of the upper vagina generally follows a pathway similar to that of the lower portion of the uterine body and cervix, with the majority draining to the internal iliac and obturator lymph nodes and a smaller portion reaching the external iliac lymph nodes. These structures further drain through the common iliac lymph nodes to the lumbar and/or presacral lymph nodes. The lymph from the fallopian tubes and ovaries primarily drains into the lumbar lymph nodes, with some draining into the internal and external iliac lymph nodes. The lymph from the fundus and upper portion of the uterine body primarily drains into the lumbar lymph nodes, with portions draining into the internal and external iliac lymph nodes or along the round ligament to the superficial inguinal lymph nodes. The lymph from the anterior and posterior walls of the uterine body can drain into the bladder and rectal lymph nodes, respectively.
Nerves
The innervation of the internal and external female genitalia is provided by a combination of somatic and autonomic nerves.
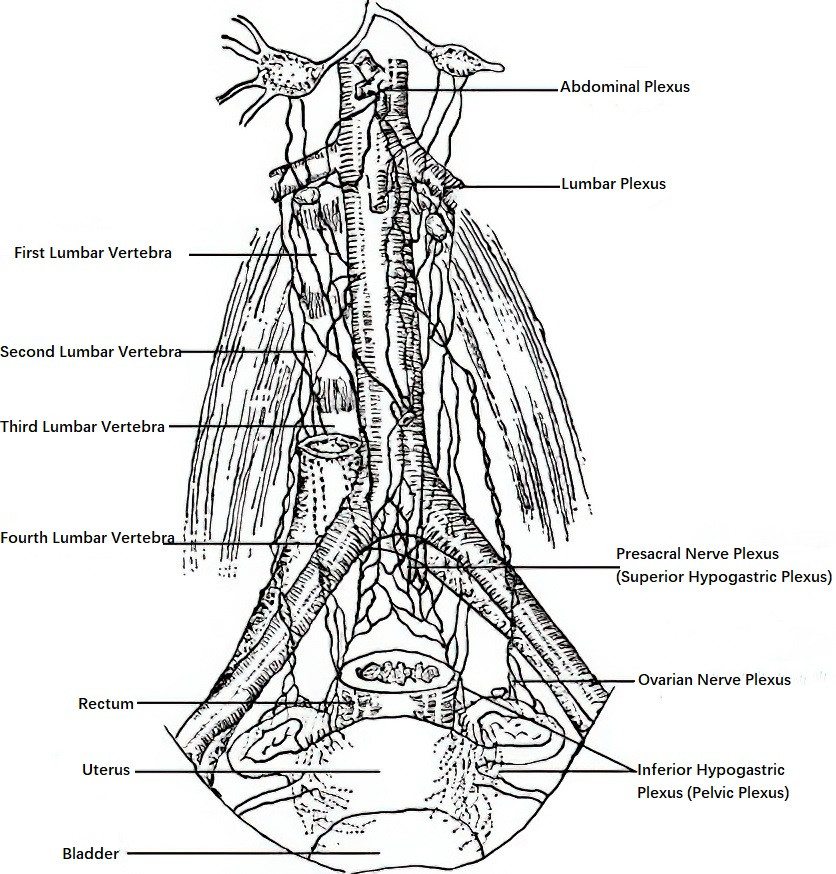
Figure 4 Nerves of the female internal reproductive organs
Innervation of the External Genitalia
The external genitalia are primarily innervated by the pudendal nerve. This nerve is formed by branches from the second to fourth sacral nerves (S2–S4) and contains both sensory and motor fibers. Its path follows that of the internal pudendal artery. Below and medial to the ischial tuberosity, the pudendal nerve divides into three branches: the perineal nerve, the dorsal nerve of the clitoris, and the anal nerve. These branches provide innervation to the perineum, labia, clitoris, and the area around the anus.
Innervation of the Internal Genitalia
The internal genitalia are mainly innervated by the autonomic nervous system, which includes both sympathetic and parasympathetic nerves. Sympathetic fibers originate from the pre-aortic nerve plexus surrounding the abdominal aorta and then enter the pelvic cavity, where they divide into two primary components:
- Ovarian Plexus: This plexus innervates the ovaries and fallopian tubes.
- Presacral Nerve Plexus: Most of these fibers form the inferior hypogastric plexus (also known as the pelvic plexus) near the cervix. Branches from this plexus innervate the body and cervix of the uterus, the upper bladder, rectum, vagina, and clitoris.
The inferior hypogastric plexus contains parasympathetic fibers originating from the second to fourth sacral nerves (S2–S4), as well as afferent sensory fibers. The smooth muscle of the uterus is capable of autonomous rhythmic contractions and retains its ability to contract rhythmically even after complete nerve removal. This autonomic activity enables the uterus to complete processes such as labor and delivery.