The cardiovascular system consists of the heart, arteries, veins, and capillaries, with blood circulating within the vessels. Its primary function is the transport of substances. Blood delivers nutrients absorbed by the digestive system and oxygen absorbed by the lungs to the tissues and cells of various organs throughout the body, while simultaneously transporting metabolic byproducts, excess water, and carbon dioxide from tissues and cells to the kidneys, lungs, and skin for excretion. This ensures the normal progression of the body's metabolism. Hormones and biologically active substances secreted by endocrine organs and dispersed endocrine cells throughout the body are also transported by the cardiovascular system to corresponding target organs for humoral regulation. Additionally, the cardiovascular system plays an important role in maintaining acid-base balance in the body, regulating body temperature, and contributing to defense mechanisms. Furthermore, the cardiovascular system itself has endocrine functions; myocardial cells, vascular smooth muscle cells, and endothelial cells produce various biologically active substances, such as atrial natriuretic peptide (ANP), renin, and angiotensin, which participate in regulating bodily functions.
Anatomy of the Heart
Heart Structure
The heart is a hollow organ divided into four chambers: the left and right atria and left and right ventricles. Venous blood from the body enters the right atrium via the superior and inferior vena cava, while the heart's venous blood enters the right atrium through the opening of the coronary sinus. From the right atrium, venous blood flows into the right ventricle through the tricuspid valve and is then ejected through the pulmonary valve located at the anterosuperior portion of the right ventricle into the pulmonary artery. After gas exchange occurs in the lungs, the oxygenated arterial blood returns to the left atrium through four pulmonary veins (two from each lung). It then flows into the left ventricle via the mitral valve and is finally ejected into the aorta through the aortic valve located at the superior portion of the left ventricle.
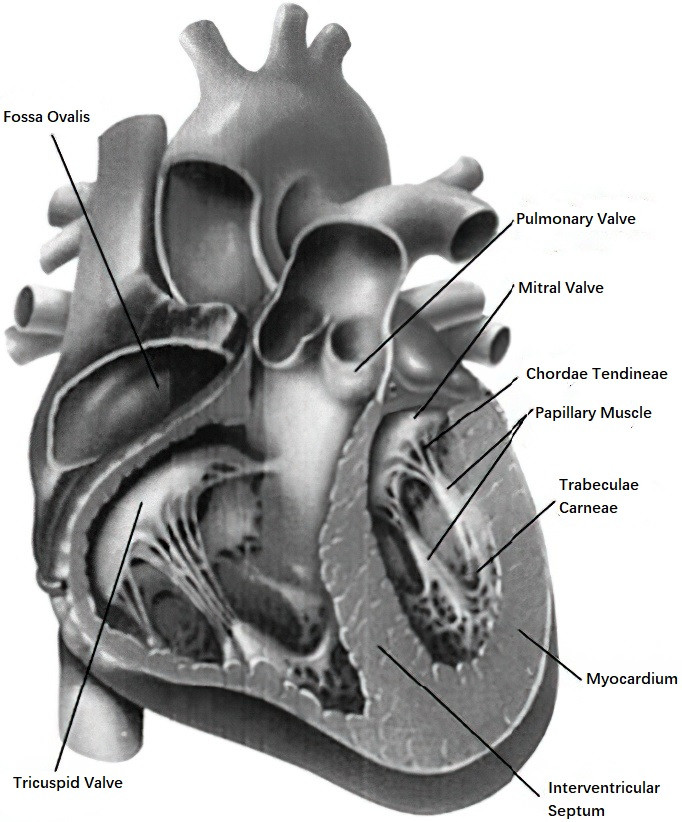
Figure 1 Structure of the heart
Cardiac Conduction System
Certain myocardial cells possess the ability to spontaneously generate action potentials, exhibiting automaticity and excitability. The cardiac conduction system consists of the sinoatrial (SA) node, atrioventricular (AV) node, atrioventricular bundle, and Purkinje fibers. The SA node, located in the wall of the right atrium, serves as the primary pacemaker of the heart due to its highest level of automaticity. Electrical excitation generated in the SA node spreads to the atrial myocardium, causing contraction of the atrial muscles. Simultaneously, the excitation is transmitted via internodal tracts to the AV node located in the lower part of the atrial septum. The AV node gives rise to the atrioventricular bundle, which traverses the ventricular septum and divides into left and right bundle branches. These branches travel along the subendocardium of their respective ventricles and terminate in fine branches known as Purkinje fibers, which distribute excitation to the ventricular muscles and trigger ventricular contraction.
Coronary Arteries
The coronary arteries are the blood vessels responsible for supplying blood directly to the heart. They are classified into the left and right coronary arteries.
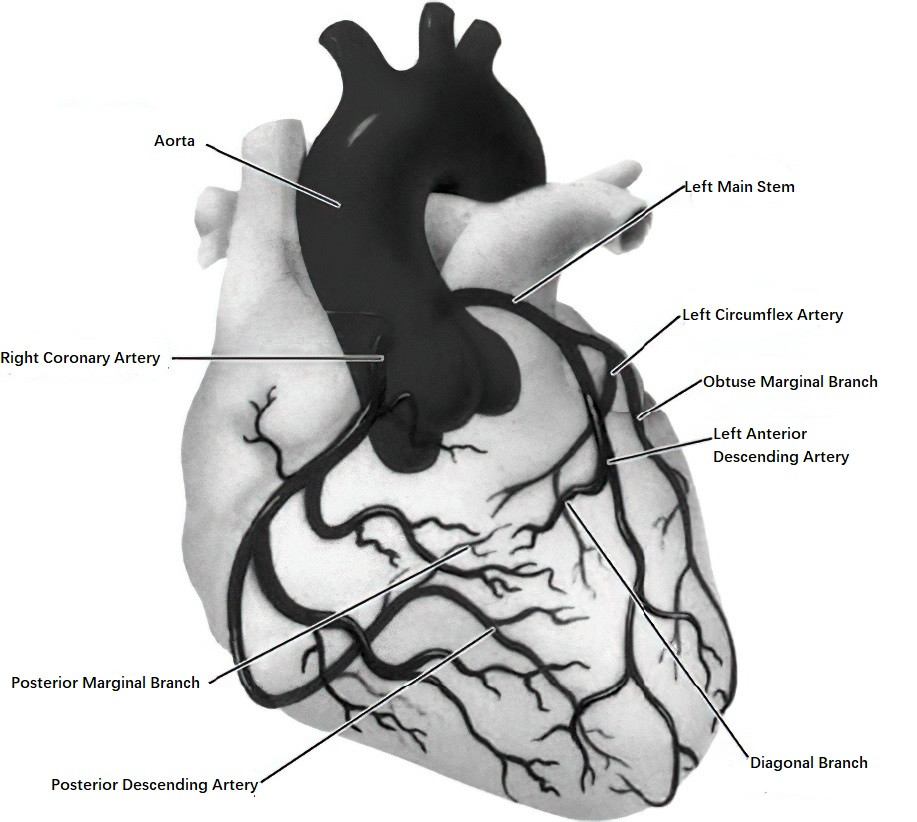
Figure 2 Coronary arteries
Left Coronary Artery
Left Main Stem
This originates from the aortic root in the coronary left sinus and branches into the left anterior descending (LAD) artery and the left circumflex artery (LCX). Occasionally, a third branch, the intermediate artery, may also arise.
Left Anterior Descending (LAD) Artery
This travels along the pulmonary artery to the anterior interventricular groove and descends toward or around the apex of the heart. Its major branches include septal perforating arteries and diagonal branches.
Left Circumflex (LCX) Artery
This courses posteriorly beneath the left atrial appendage, reaching the left atrioventricular groove. Its significant branches include obtuse marginal arteries.
Right Coronary Artery (RCA)
Most often originates from the aortic root in the coronary right sinus and descends along the right atrioventricular groove, extending to the posterior interventricular groove in the majority of cases. Its branches include the conus artery, sinoatrial nodal artery, and acute marginal artery. Distally, it bifurcates into the posterior descending artery (PDA) and the posterior lateral branches.
Cardiac Physiology
Myocardial Action Potential
The myocardial action potential can be divided into the following phases:
- Depolarization phase (Phase 0).
- Repolarization process:
- Phase 1 (early rapid repolarization),
- Phase 2 (plateau phase),
- Phase 3 (late rapid repolarization),
- Phase 4 (resting phase).
Understanding these action potential phases provides significant insights into the mechanisms of antiarrhythmic drugs and ion channel disorders.
Pressure and Volume Curve Dynamics
The pressure and volume changes observed in the atria, ventricles, and aorta provide a comprehensive understanding of the cardiac systolic and diastolic processes.
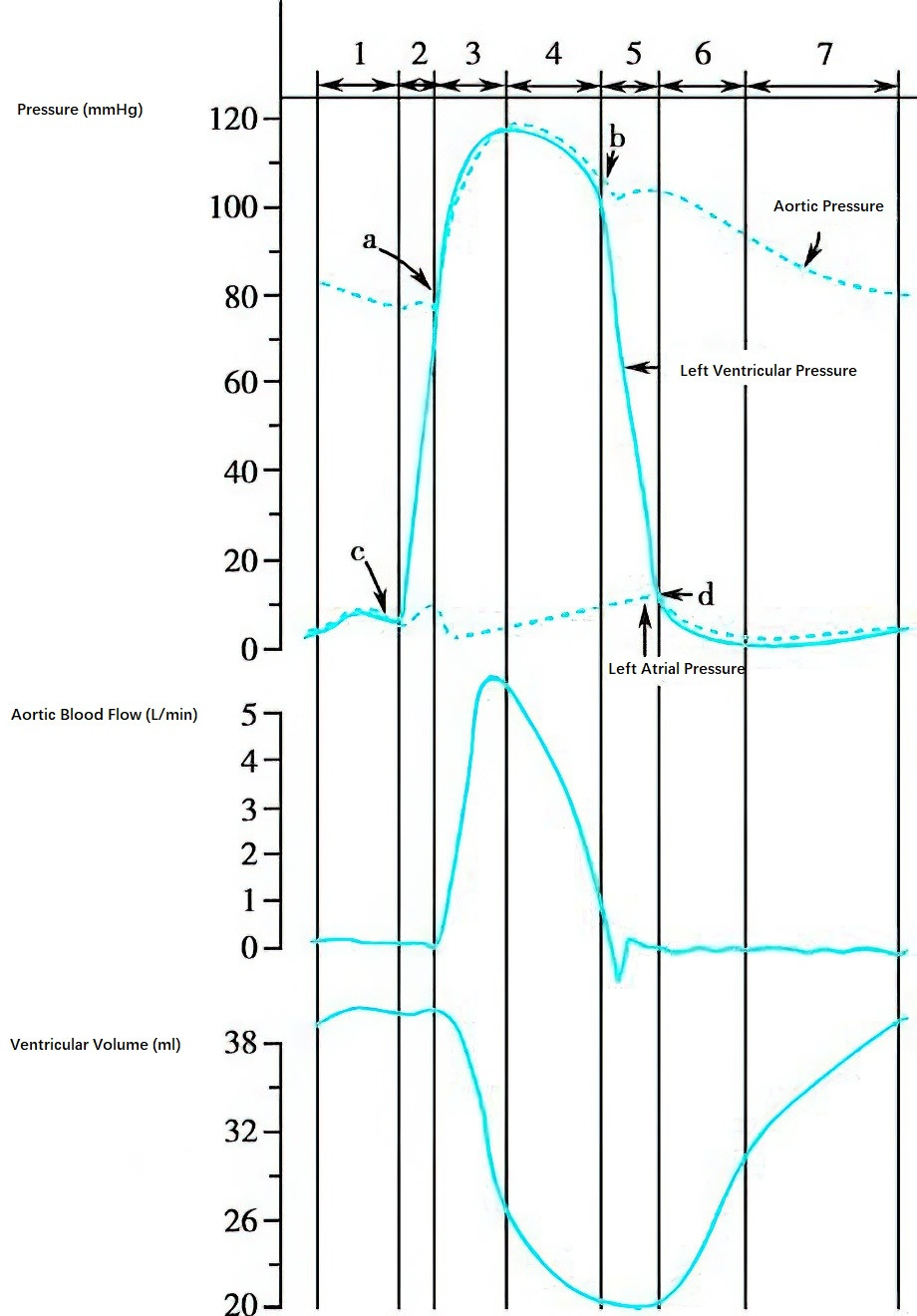
Figure 3 Pressure and volume changes in the atria, ventricles, and aorta
a. Aortic Valve Opens
b. Aortic Valve Closes
c. Mitral Valve Closes
d. Mitral Valve Opens
Ventricular Systole
Isovolumetric Contraction Phase
A sharp increase in intraventricular pressure occurs without changes in ventricular volume.
Rapid Ejection Phase
Large volumes of blood are ejected into the aorta, leading to a corresponding increase in aortic pressure. This accounts for approximately 70% of total ejection volume and is accompanied by a rapid decrease in ventricular volume.
Reduced Ejection Phase
Both intraventricular pressure and aortic pressure gradually decline from their peak, ejecting the remaining 30% of total ejection volume while ventricular volume further reduces.
Ventricular Diastole
Isovolumetric Relaxation Phase
A rapid decrease in intraventricular pressure occurs without changes in ventricular volume.
Rapid Filling Phase
Blood flows quickly from the atria into the ventricles, resulting in an increase in ventricular volume.
Reduced Filling Phase
The rate of blood inflow slows, further increasing the ventricular volume.
Symptoms, Signs, and Laboratory Tests
The diagnosis of cardiovascular diseases should be based on a comprehensive analysis of data from medical history, clinical symptoms and signs, laboratory tests, and instrumental examinations.
Symptoms
Common symptoms of cardiovascular diseases include cyanosis, dyspnea, chest tightness, chest pain, palpitations, edema, and syncope. Other symptoms may include cough, headache, dizziness or vertigo, upper abdominal distension or pain, nausea, vomiting, and hoarseness. These symptoms may also occur in diseases of other systems, necessitating careful differential analysis during evaluation.
Signs
The signs of cardiovascular diseases often show specificity and are particularly valuable in diagnosing conditions such as valvular heart disease, congenital heart disease, pericarditis, heart failure, and arrhythmias. Common cardiovascular signs are described as follows:
Inspection
Observation focuses on general condition, respiratory status (e.g., presence of orthopnea), as well as the presence of cyanosis, anemia, jugular vein distension, edema, precordial bulging, or abnormal pulsations in the apex and precordial regions. Additionally, signs such as annular erythema and subcutaneous nodules can assist in diagnosing rheumatic fever. A purple-red flush on the malar region is useful for diagnosing mitral stenosis and pulmonary hypertension. Petechiae of the skin and mucosa, Osler's nodes, and Janeway lesions are indicative of infective endocarditis. Clubbing of the fingers and toes suggests congenital heart disease with right-to-left shunting.
Palpation
Palpation is initially performed with the entire palm followed by the thenar eminence, aiming to determine abnormalities such as deviations in the apex beat, the presence of thrills or pericardial friction rubs, capillary pulsations, venous distension or abnormal pulsations, irregularities in pulse morphology, hepatojugular reflux, hepatosplenomegaly, or lower limb edema.
Percussion
Percussion is used to determine the relative cardiac dullness by noting changes in the percussion tone from clear to dull. This helps assess whether there is cardiac enlargement. The left border is percussed first, followed by the right border. Percussion begins 2-3 cm lateral to the point of maximum left apical impulse, moving inward through intercostal spaces toward the second intercostal space. For the right border, percussion starts at the liver's superior boundary, then proceeds one intercostal space above that point. Percussion is continued inward and upward through the intercostal spaces to the second intercostal space.
Auscultation
Auscultation involves assessing heart rate, rhythm, heart sound intensity, heart sound splitting, heart murmurs, extra heart sounds, pericardial friction rubs, pulmonary rales, peripheral arterial murmurs, or gunshot-like sounds. Auscultation follows an order through specific regions, namely the apex area (mitral valve auscultation area), the pulmonary valve area, the aortic valve area, the second aortic valve area, and the tricuspid valve area.
Laboratory Tests
Laboratory testing primarily includes complete blood counts, urinalysis, and various biochemical analyses, such as lipid profiling and measurements of cardiac injury markers like serum cardiac troponin, myoglobin, and cardiac enzymes. Measurements of heart failure markers, such as brain natriuretic peptide (BNP), are also performed. Additionally, microbiological and immunological testing is important. For infective endocarditis, microbial cultures, viral nucleic acids, and antibody testing are conducted. For rheumatic heart disease, tests for streptococcal antibodies and inflammatory markers such as antistreptolysin O (ASO), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) are utilized.
Auxiliary Examinations
Non-Invasive Examinations
Blood Pressure Measurement
This category includes clinic blood pressure measurements, ambulatory blood pressure monitoring, and home self-measured blood pressure. Clinic blood pressure encompasses conventional physician-measured blood pressure as well as self-measured clinic blood pressure, the latter generally yielding slightly lower readings than physician-measured values. Ambulatory 24-hour blood pressure monitoring aids in the early diagnosis of hypertension and assists with distinguishing secondary hypertension, resistant hypertension, white-coat hypertension, and masked hypertension. This approach also provides guidance for personalized medication regimens. Home self-measured blood pressure is simple and convenient, making it suitable for patient self-monitoring.
Electrocardiography (ECG)
This includes routine ECG, 24-hour ambulatory ECG (Holter monitoring), exercise stress testing, telemetry ECG, ventricular late potential analysis, and heart rate variability analysis.
Routine ECG
Analysis typically focuses on heart rate, rhythm, conduction intervals, waveform amplitudes, and morphology. It is used to determine the presence of conditions such as arrhythmias, myocardial ischemia/infarction, atrial or ventricular enlargement, and electrolyte imbalances.
Exercise Stress Testing
This is the most commonly used auxiliary method for diagnosing coronary artery disease. It involves inducing myocardial ischemia by increasing cardiac workload through exercise, which triggers ischemic changes on the ECG. Treadmill exercise tests are often employed.
Holter Monitoring
Also known as ambulatory ECG, this technique continuously records heart signals over 24–72 hours to improve the detection rate of transient arrhythmias and brief episodes of myocardial ischemia.
Echocardiography
M-Mode Echocardiography
This method displays the echoes from cardiac anatomical structures as motion curves, aiding in detailed analysis of cardiac activity. It is primarily used to examine the function and movement of the aortic root, mitral valve, and left ventricle.
Two-Dimensional Echocardiography
This is the most essential and widely applied cardiac ultrasound technique. It provides real-time visualization of cardiac structures and their motion. Common imaging planes include the parasternal long-axis view, parasternal short-axis view of the aorta, and the apical four-chamber view.
Doppler Echocardiography
This encompasses techniques such as color Doppler flow imaging (CDFI) and spectral Doppler, which analyze blood flow timing, direction, velocity, and properties. When combined with two-dimensional echocardiography, Doppler technology allows for detailed assessment of valvular function. Additionally, tissue Doppler imaging (TDI) has seen rapid advancements and is becoming a key quantitative tool for evaluating cardiac systolic and diastolic function as well as left ventricular filling hemodynamics.
Transesophageal Echocardiography (TEE)
Because the esophagus lies close to the heart, TEE enhances the visualization and resolution of cardiac structures, especially those located posteriorly, such as the atrial septum, left-sided cardiac valves, and left-sided heart chambers (e.g., for the detection of left atrial thrombi).
Contrast Echocardiography: This method involves injecting a contrast agent containing microbubbles into the bloodstream, which allows specific target organs to be highlighted. It provides important diagnostic evidence. Contrast echocardiography of the right heart system retains significant value in diagnosing cyanotic congenital heart disease, while studies of the left heart system and coronary arteries assist in evaluating myocardial perfusion areas, coronary blood flow and reserve capacity, viable myocardium, collateral circulation, and the effectiveness of revascularization.
Real-Time Three-Dimensional Echocardiography
This technique enables more precise quantitative analysis of cardiac size, shape, and function. It is particularly useful for localizing abnormal lesions in surgical planning and guiding certain cardiac catheter procedures, including right ventricular myocardial biopsy.
Chest X-Ray
Chest X-rays provide visual assessments of the size, shape, position, and contours of the heart and great vessels. This modality also allows the evaluation of cardiac relationships with adjacent structures and changes in pulmonary vasculature.
Cardiac CT
Cardiac CT was conventionally used to observe changes in cardiac structures, myocardium, pericardium, and large vessels. In recent years, coronary CT angiography (CTA) has become a widely used non-invasive imaging technique for assessing coronary atherosclerosis. This method allows visualization of coronary artery branches, anatomical anomalies, and bypass grafts and serves as an important tool for screening and diagnosing coronary artery disease.
Cardiac MRI
Cardiac MRI offers insights into cardiac anatomy, function, myocardial, and pericardial abnormalities. Using delayed enhancement techniques, it quantifies myocardial scar size, identifies viable myocardium, and aids in the differential diagnosis of various myocardial diseases.
Cardiac Nuclear Medicine
Normal or functional myocardial cells selectively uptake certain radiopharmaceuticals, with uptake proportional to coronary perfusion at a given site and closely related to local myocardial cell functionality or metabolic activity. This modality allows quantitative analysis of myocardial perfusion, viability, and cardiac function. Imaging techniques include cardiac blood pool imaging, myocardial perfusion imaging, and myocardial metabolism imaging. Common radiotracers include 201Tl, 99mTc-MIBI, and 18F-FDG. The commonly used imaging technologies include single-photon emission computed tomography (SPECT) and positron emission tomography (PET). Compared to SPECT, PET offers higher specificity and sensitivity.
Invasive Examinations
Right Heart Catheterization
This is a minimally invasive interventional technique involving the insertion of a catheter through peripheral veins into the superior or inferior vena cava, right atrium, right ventricle, pulmonary artery, and its branches. It enables hemodynamic measurements, blood oxygen analysis, and determination of cardiac output in the vena cava and right heart chambers. Contrast agents can also be injected via the catheter for imaging of the vena cava, right atrium, right ventricle, and pulmonary arteries to assess hemodynamic changes. It is used for diagnosing congenital heart diseases, determining surgical indications, and evaluating cardiac function. Clinically, a Swan-Ganz catheter (floating catheter) can be guided into the distal pulmonary artery via venous access (commonly the femoral or internal jugular vein) to provide continuous bedside hemodynamic monitoring. This technique is primarily applied in critically ill patients with significant hemodynamic changes, such as those with acute myocardial infarction, heart failure, or shock.
Left Heart Catheterization
Left Heart Catheterization
This involves inserting a catheter through a peripheral artery into locations such as the aorta and left ventricle to measure pressures and perform cardiovascular imaging. This examination provides information about left ventricular function, wall motion, cardiac chamber size, and the function of the aortic and mitral valves.
Selective Coronary Angiography
This procedure records the path, distribution, anatomy, and functional abnormalities of the coronary arteries and their branches, including atherosclerosis, thrombosis, congenital anomalies, or coronary artery spasms. Additionally, it assesses coronary artery collateral circulation. It remains the conventional “gold standard” for diagnosing coronary artery diseases and is widely used for treatment planning, despite the rapid advancements in non-invasive imaging technologies such as coronary CTA.
Electrophysiological Study (EPS)
This method involves recording intracardiac electrograms and applying specific electrical impulses to diagnose and study arrhythmias. It is also essential for catheter ablation procedures to treat certain arrhythmias.
Intravascular Imaging Techniques
Intracardiac Echocardiography (ICE)
A catheter with an ultrasound probe is introduced through a peripheral vein into the right heart system, producing clear images of cardiac structures. This technique is particularly beneficial for interventional procedures involving valves or atrial septum puncture.
Intravascular Ultrasound (IVUS)
A miniature ultrasound transducer mounted at the tip of a catheter is inserted into the vascular lumen. This technology provides cross-sectional images of coronary arteries and evaluates lesion characteristics, vessel diameter, plaque size, plaque composition, and plaque burden. It is valuable for assessing the severity of coronary lesions, guiding and optimizing interventional treatments, evaluating treatment efficacy, and predicting outcomes.
Optical Coherence Tomography (OCT)
This method uses infrared-based imaging guidewires inserted into the vessel, producing cross-sectional images of coronary arteries with a resolution approximately ten times higher than that of IVUS. Its applications in assessing lesion severity, guiding interventional strategies, and evaluating treatment outcomes are comparable to those of IVUS.
Functional Assessment of Vascular Stenosis
Fractional Flow Reserve (FFR)
This parameter represents the ratio of maximum blood flow achievable in a myocardial region supplied by a stenosed coronary artery to the maximum blood flow under normal conditions. It is determined by inserting a pressure wire to measure pressure across the lesion. FFR is commonly used to evaluate whether interventional therapy is necessary for borderline or multi-vessel lesions.
Quantitative Flow Ratio (QFR)
This is a novel technique that calculates FFR from three-dimensional reconstruction and hemodynamic analysis based on coronary angiography, without the need for pressure wires or adenosine administration. QFR provides high accuracy, sensitivity, and specificity, demonstrating a strong consistency with FFR results. Since QFR does not require intracoronary devices, it reduces procedural time and cost and is considered a potential alternative for evaluating myocardial ischemia, further optimizing interventional treatment strategies for coronary artery disease.
Endomyocardial Biopsy
This procedure involves extracting small cardiac tissue samples using biopsy forceps to study the structure and pathological changes of the heart. It plays a crucial role in diagnosing myocarditis, cardiomyopathy, cardiac amyloidosis, myocardial fibrosis, and related conditions. It is also essential for assessing rejection and treatment outcomes after heart transplantation. The procedure is typically performed through a venous approach to the right ventricle under fluoroscopic guidance, with occasional use of an arterial approach to the left ventricle. The most common biopsy site is the right ventricular septum, as this reduces the risk of cardiac perforation and avoids complications like stroke.
Pericardiocentesis
Pericardiocentesis involves inserting a needle into the pericardial cavity with or without X-ray or echocardiographic guidance. Its purposes include:
- Draining pericardial effusion to relieve increased intrapericardial pressure, which serves as an emergency intervention for acute cardiac tamponade.
- Collecting pericardial fluid for biochemical analysis, bacteriological/cytological examinations, bacterial cultures, and determination of the underlying cause of pericardial effusion to aid in differential diagnosis of various pericardial diseases.
- Administering medications (e.g., antibiotics) into the pericardial cavity for therapeutic purposes through pericardiocentesis.
Treatment of Cardiovascular Diseases
Pharmacological Therapy
Although there are an increasing number of treatment approaches for cardiovascular diseases, pharmacological therapy remains fundamental, essential, and one of the most important first-line options. Common drugs for treating cardiovascular diseases are often classified based on their mechanisms of action, including angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), β-blockers, nitrates, diuretics, α-blockers, positive inotropic agents, lipid-modifying drugs, antiarrhythmic drugs, calcium channel blockers, and antithrombotic agents. Newer cardiovascular drugs include novel oral anticoagulants, cholesterol absorption inhibitors (e.g., ezetimibe), proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, small interfering RNA (siRNA) drugs (e.g., inclisiran), as well as angiotensin receptor-neprilysin inhibitors (ARNI) and sodium-glucose cotransporter-2 (SGLT2) inhibitors for heart failure treatment. Clinical considerations such as pharmacological effects, indications, contraindications, side effects, and precautions remain critical, while individualized treatment is a key factor in achieving successful outcomes with drug therapy.
Interventional Therapy
Interventional therapy has become a highly significant approach to treating cardiac diseases. Continuous advancements in techniques and expanding indications have greatly improved patient prognosis and quality of life.
Percutaneous Coronary Intervention (PCI)
This is one of the most common and well-established interventional techniques for treating coronary artery disease. Under the guidance of angiography, specialized devices such as catheters, guidewires, balloons, and stents are used for coronary revascularization in stenotic or occluded coronary arteries. Device improvements, especially drug-eluting stents, have significantly enhanced the prognosis and quality of life of patients with coronary artery disease. Emerging technologies such as drug-coated balloons and bioabsorbable stents are also being applied in clinical practice.
Catheter Radiofrequency Ablation
This involves inserting an electrode catheter through veins or arteries to specific intracardiac locations, where radiofrequency currents are released to induce coagulative necrosis of the endocardium and subendocardial myocardium. This process interrupts the conduction pathways and origins of abnormal rapid arrhythmias. The procedure is minimally invasive, and the introduction of three-dimensional mapping systems has markedly increased the success rate. It is now a key strategy for treating various tachyarrhythmias, including atrial fibrillation.
Cryoablation
Cryoablation represents a newer technique for treating arrhythmias. By using liquid refrigerants to induce heat absorption and evaporation, tissue temperature at the target site is lowered, destroying cells responsible for abnormal electrophysiological activity to eliminate arrhythmias. Compared to conventional radiofrequency ablation, cryoablation offers easier manipulation for physicians, shorter procedural times, high efficacy, and reduced risks of severe complications such as thrombosis while minimizing patient discomfort. It is currently primarily applied in the interventional treatment of paroxysmal atrial fibrillation.
Pulsed Field Ablation (PFA)
PFA is an advanced ablation system that uses pulsed electric fields as its energy source. It delivers short-duration, high-voltage electrical pulses designed to induce non-thermal cellular ablation by inducing electroporation. This allows extracellular ions to enter cells, and when high concentrations of calcium ions (Ca2+) enter, the cells rupture and die. Because PFA-induced damage to tissues with a high electric field threshold is reversible, while myocardial tissue has a low electric field damage threshold (around 400 V/cm), myocardial cells can be selectively targeted without heat generation. PFA protects critical structures surrounding ablation sites and is considered a safer, more effective, and efficient option compared to existing cardiac ablation technologies.
Catheter-Based Renal Sympathetic Denervation (RDN)
RDN is a technique that interrupts renal efferent nerves to suppress the sympathetic nervous system, inhibit the renin-angiotensin system, and break the vicious cycle of elevated blood pressure. It is primarily used to treat resistant hypertension, though its efficacy and safety require further validation through clinical research.
Cardiac Pacing
Cardiac pacing, collectively referred to as cardiovascular implanted electronic devices (CIED), includes conventional pacemakers for bradyarrhythmias, cardiac resynchronization therapy (CRT) devices, and implantable cardioverter-defibrillators (ICDs). Conventional pacemakers involve single-chamber or dual-chamber pacing modes. In recent years, leadless pacemakers and conduction system pacing have gained popularity. CRT devices deliver pacing to the left ventricular epicardial myocardium via the coronary sinus or stimulate the conduction system to correct ventricular dyssynchrony, improving cardiac function in patients with systolic heart failure and reducing mortality. ICDs significantly reduce the risk of sudden cardiac death (SCD) and overall mortality in high-risk patients. Recent advancements have been made in ICD algorithms, programming, and non-venous implantation approaches.
Percutaneous Closure of Congenital Heart Defects
This includes closure procedures for ventricular septal defects, atrial septal defects, and patent ductus arteriosus. These minimally invasive interventions offer rapid recovery and outcomes comparable to surgical repairs. The interventional treatment of congenital heart defects has reached a globally leading level.
Interventional Treatment of Cardiac Valvular Diseases
Since the introduction of balloon valvuloplasty in the 1980s and percutaneous valve implantation or repair techniques in the early 2000s, interventional treatments for valvular diseases have seen rapid advancements and expanding indications. Techniques for aortic, mitral, and pulmonary valve stenosis have matured, while interventions for valve regurgitation continue to be explored further.
Surgical Therapy
Surgical therapy encompasses coronary artery bypass grafting (CABG), cardiac valve repair and replacement, correction of congenital heart defects, pericardiectomy, and heart transplantation.
Other Therapies
Genetic screening plays a significant role in the prevention and treatment of hereditary or familial cardiovascular diseases. Stem cell transplantation and angiogenesis have demonstrated considerable progress in animal studies and show promising potential for clinical applications. Molecular cardiology is expected to contribute further novel diagnostic and therapeutic approaches to clinical practice in the future.