Cervical imaging examinations encompass various modalities, including B-ultrasound, X-ray, CT, MRI, PET/CT, DSA, and radionuclide imaging.
Cervical B-ultrasound Examination
B-ultrasound provides information about the size, shape, and number of masses, as well as their internal echogenicity, surrounding capsule structure, and relationship with adjacent tissues. Common cervical conditions present the following sonographic features:
Thyroglossal Duct Cyst
Masses are located beneath the hyoid bone and appear as round or near-round shapes on ultrasound. They are well-encapsulated with hypoechoic areas internally, indicating homogeneity of the medium and good translucency, typically without adhesion to surrounding tissues.
Thyroid Adenomas or Cancer
Thyroid adenomas typically appear as round or oval shapes with well-defined, smooth boundaries and a capsule. They often exhibit hypoechoic or isoechoic areas internally, with anechoic features possible in the presence of hemorrhage or cystic changes. Tumors with irregular internal echo patterns, poorly defined margins, absence or incomplete capsules, and rapid enlargement are suggestive of thyroid cancer.
Carotid Body Tumor
Masses are located at the bifurcation of the internal and external carotid arteries, presenting as hypoechoic regions. The distance between the internal and external carotid arteries is widened, with the tumor encasing the carotid artery. Localized thickening of the arterial wall and lumen narrowing may be observed.
Schwannoma
Masses appear as round or oval, with uniform hyperechoic regions internally. Anechoic areas may occasionally appear due to fluid. The tumor is encapsulated, has clear boundaries with surrounding tissues, exhibits no invasiveness, but may exert compression on adjacent structures.
Metastatic Cervical Lymph Nodes and Malignant Tumors
Sonographic features include heterogeneous internal echoes with variable intensity. The majority exhibit hypoechoic or low-echo areas with posterior echo attenuation. Hemorrhage, necrosis, and liquefaction may be observed. Tumors usually have poorly defined boundaries, absent or incomplete capsules, irregular margins, and an atypical shape.
Pleomorphic Adenoma and Malignant Tumors of the Parotid Gland
Pleomorphic adenomas appear as round or near-round masses with moderate hypoechoic regions internally, displaying relatively homogeneous echogenicity. Anechoic areas may be present in cases of cystic transformation or hemorrhage within the tumor. These masses typically have well-defined boundaries and are encapsulated. Irregular shapes, poorly defined margins, absent capsules, heterogeneous internal echoes, and attenuation are suggestive of malignancy.
Cervical X-ray
Cervical X-ray imaging in the anteroposterior and lateral positions reveals the presence of laryngeal or tracheal stenosis, obstruction, deviation, or displacement. Opaque foreign bodies within the larynx, trachea, or esophagus are identified. Swelling, abscesses, emphysema, or opaque foreign bodies within the cervical soft tissues are also evaluated. Soft tissue swelling or accumulation of abscesses in the retropharyngeal or retroesophageal spaces is noted. Dislocations in the atlantoaxial joint of the cervical spine, as well as changes in intervertebral disk spaces (either widening or narrowing), and alterations in cervical spine curvature are assessed. Oblique views can further examine intervertebral foramen sizes and bony spurs.
Computed Tomography (CT)
CT imaging provides clearer visualization of bony structures compared to MRI. Cervical CT scans reveal the location, size, shape, and relationship of masses with surrounding tissues. Measurements of CT values offer approximate determinations of mass characteristics (solid, cystic, mixed, or fatty tissue). Contrast-enhanced CT distinguishes vascular tumors from enlarged lymph nodes, evaluates tumor blood supply, and assesses relationships between tumors and adjacent blood vessels. Bone destruction in the cervical spine is also clearly depicted with CT imaging.
Magnetic Resonance Imaging (MRI)
MRI offers higher resolution for soft tissue than CT. Characteristics based on signal intensity, T1, and T2 values include:
- Signal Intensity: Higher signal intensity corresponds to brighter images, appearing whiter; lower signal intensity appears darker. The grayscale ranking of normal cervical tissues from white to black is as follows: fat, viscera, muscle, rapidly flowing blood, bone, and air.
- T1 and T2 Correlation with Signal Intensity: Longer T1 values result in lower signal intensity and darker images. Longer T2 values result in higher signal intensity and brighter images. Congenital cervical cysts are typically characterized by markedly long T1 and T2 values. Cervical masses are often associated with long T1 and short T2 values.
- Flow Void Effect: Flowing fluids within the body do not produce any signal. The flow void effect allows differentiation of vascular structures, such as carotid aneurysms, carotid body tumors, and vascular malformations, without the need for vascular contrast agents. It further aids in distinguishing blood vessels from masses or enlarged lymph nodes.
CT and MRI appearances of common cervical diseases are as follows:
Lymph Node Metastases
On CT scans, metastatic lymph nodes appear as solitary or multiple nodular opacities, round or spherical in shape, with variable sizes. Central hypodense areas within the nodules may indicate necrosis. Contrast-enhanced CT displays irregular annular enhancement of the nodules, with unclear boundaries between the nodes and surrounding tissues. On MRI, the T1-weighted images show signal intensity similar to surrounding muscle, while T2-weighted images exhibit higher signal intensity than muscle. Central necrosis appears as low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Contrast-enhanced T1-weighted images resemble the findings in CT.
Neurogenic Tumors
This category includes schwannomas and neurofibromas. On CT scans, these tumors are often round or oval with clear boundaries and smooth capsules. Schwannomas usually have a thicker capsule and display homogeneous density; some may reveal cystic degeneration or calcifications within the tumor. After contrast administration, schwannomas show minimal enhancement. Neurofibromas have less distinct capsules, are usually multiple, appear as plexiform nodules, and exhibit lower density compared to adjacent blood vessels, with minimal post-contrast enhancement. On MRI, axial imaging shows round or oval tumors with smooth boundaries. T1-weighted images show signal intensity similar to muscle, while T2-weighted images display slightly higher signal intensity. Necrotic areas within the tumor exhibit long T2 signals and thick walls. Sagittal and coronal images help delineate the relationship between the tumor and nearby major blood vessels.
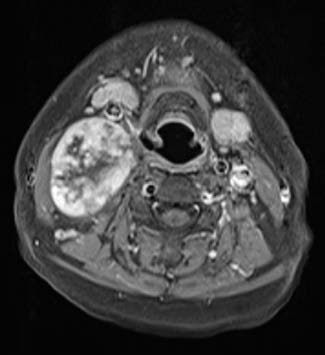
Figure 1 Axial MRI of the neck showing a schwannoma on the right side
Thyroid Adenomas
On CT scans, thyroid adenomas typically appear as round or near-round lesions, single or multiple, with variable sizes and clear boundaries. Intratumoral hypodense changes and occasional calcifications are observed. Post-contrast, the lesion may show enhancement, but with densities still lower than normal thyroid tissue. On MRI, adenomas demonstrate clear boundaries. Compared to thyroid tissue, T1-weighted images show low or isointense signals, while T2-weighted images display high signals. Hemorrhage within the adenoma may present as high signal intensity on both T1- and T2-weighted images.
Thyroid Carcinoma
Early-stage thyroid cancer appears as multiple nodules on CT imaging, which rapidly progress to form masses or lobulated soft tissue opacities. The internal density of the tumor is uneven, with poorly defined boundaries, calcifications, and areas of necrosis without post-contrast enhancement. On MRI, T1-weighted images show slightly high, slightly low, or isointense signals, with possible high signal intensity in cases of intratumoral hemorrhage. T2-weighted images reveal heterogeneous high signal intensities.
Malignant Lymphomas
On CT scans, malignant lymphomas initially manifest as single or multiple nodules that later merge into larger, poorly defined masses. Surrounding tissue may also be compressed or displaced. Tumors often exhibit heterogeneous density and uneven contrast enhancement. On MRI, T1-weighted images display low or isointense signals, while T2-weighted images show heterogeneous high signal intensity.
Carotid Body Tumors
On CT scans, carotid body tumors appear as round or oval masses in the carotid triangle with well-defined boundaries. The tumors show soft tissue density and significant, homogeneous enhancement upon contrast administration, with CT values reaching 90–130 HU, further clarifying tumor margins. On MRI, T1-weighted images show signal intensity equal to or slightly higher than adjacent muscle, while T2-weighted images display higher signal intensity compared to muscle.
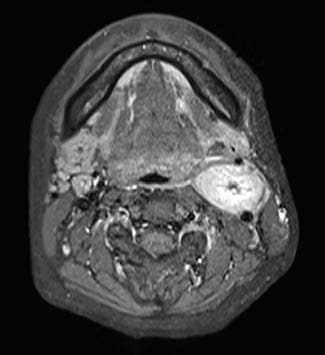
Figure 2 Axial MRI of the neck showing a carotid body tumor on the left side
Lipomas
The characteristic CT values of lipomas range from -80 to -100 HU, distinguishing them from other tissues. These tumors may have unclear boundaries with surrounding normal fat tissue and possibly internal septations. Nearby tissues may appear compressed or displaced. Small lipomas lack clear capsules, making differentiation from normal fat on CT challenging; comparison with the contralateral side at the same location may be necessary. On MRI, lipomas exhibit signal intensity equal to or slightly higher than normal fat on both T1- and T2-weighted images.

Figure 3 Axial MRI of the neck showing a lipoma on the right side
(T1-TSE without fat suppression, with the lipoma displaying high signal intensity.)
Liposarcomas
CT values of liposarcomas range from -50 to 20 HU, with heterogeneous densities due to necrosis, hemorrhage, or other internal changes. The tumors often have indistinct margins and show significant peripheral enhancement after contrast administration. Adjacent tissues are frequently infiltrated. On MRI, T1-weighted images indicate lower signal intensity compared to normal fat, while T1- and T2-weighted images show slightly higher signal intensity than normal fat. Tumor margins are irregular, and adjacent tissues may show infiltration.
Positron Emission Tomography (PET)
PET is one of the most advanced imaging modalities in modern medical imaging and exhibits the following characteristics:
- The device itself offers high spatial resolution.
- It employs electronic collimation coincidence counting, resulting in high sensitivity.
- It facilitates attenuation correction and quantitative analysis.
The commonly used positron-emitting radionuclides are elements essential to human life, such as components of glucose, fatty acids, and amino acids, which naturally participate in metabolic processes.
Clinically, glucose metabolism imaging is frequently used to reflect the metabolic state of the human body at both normal and pathological conditions on a molecular level. Since metabolic changes occur in tumors at a very early stage, metabolic abnormalities are detectable before structural changes manifest. For this reason, fluorodeoxyglucose (FDG) PET is more sensitive than CT in detecting tumors. However, due to the lack of detailed anatomical localization, the diagnostic accuracy of PET alone is relatively low. FDG PET/CT combines the functional imaging of PET and the anatomical imaging of CT, leveraging the strengths of both techniques. This integration holds significant importance in the early diagnosis of tumors.
Digital Subtraction Angiography (DSA)
DSA works on the principle of injecting contrast agents and utilizing computer subtraction to enhance arterial imaging. After subtraction, the contrast sensitivity of the resulting images is significantly higher than that of non-subtracted images. DSA plays an essential role in diagnosing vascular-related cervical masses.
Indications
Vascular Disorders
DSA is used to further confirm the diagnosis of vascular lesions, such as arterial and venous malformations or arteriovenous fistulas.
Vascular-Associated Tumors
For tumors such as carotid body tumors, jugular body tumors, and cavernous hemangiomas, DSA helps confirm the diagnosis, assess tumor blood supply, and plan endovascular interventions.
Interventional Therapy
Besides diagnosis, DSA facilitates endovascular interventional treatments. With DSA guidance, embolization materials are delivered via intravascular catheters to block blood supply to the tumor, reducing intraoperative blood loss or treating the tumor itself. Preoperative embolization is often performed for highly vascularized tumors, such as nasopharyngeal angiofibromas and cavernous hemangiomas, to minimize bleeding during surgery. Common embolization materials include absorbable gelatin sponge, stainless steel balls, and polyvinyl alcohol (PVA).
Assessment of Intracranial Arterial Collateral Circulation
Preoperative bilateral carotid artery and vertebrobasilar artery imaging is used to assess the presence of intracranial arterial collateral branches and evaluate whether intraoperative internal carotid artery ligation is feasible.
Contraindications
Patients with poor general health or severe cardiac, renal, or hepatic dysfunction, coagulation disorders, or significant arterial plaques are contraindicated for DSA.
Common Findings in Cervical Masses on DSA
Characteristic Features of Carotid Body Tumors
Richly vascularized masses are found at the bifurcation of the common carotid artery, separating the external and internal carotid arteries, and causing the bifurcation to widen. The mass compresses and displaces the internal and external carotid arteries into an arc-like or globular formation, pushing the bifurcation anteriorly.
Benign Cervical Tumors (Schwannomas and Pleomorphic Adenomas)
Larger tumors may compress and displace the carotid artery, while the tumor itself shows little to no vascular imaging.
Malignant Cervical Tumors
Larger or vascular-adjacent malignant tumors may encase and compress blood vessels, leading to vascular narrowing or occlusion, particularly in veins, which are more susceptible to compression.
Radionuclide Imaging
Radionuclide imaging plays a crucial role in diagnosing thyroid diseases.
Thyroid Iodine Uptake Test
After oral administration of the radionuclide iodine-131 (131I) on an empty stomach, thyroid iodine uptake values are measured at 2 hours and 24 hours. An iodine uptake exceeding 25% at 2 hours or 50% at 24 hours, with an early peak uptake of ¹³¹I, is indicative of hyperthyroidism.
Thyroid Radionuclide Imaging
This diagnostic method visualizes the thyroid externally using scanning equipment or gamma cameras to analyze the distribution of radionuclides in the thyroid. Common radionuclides include 131I and technetium-99m (99mTc). Imaging instruments include gamma cameras and emission computed tomography (ECT) scanners. ECT provides three-dimensional imaging, superior to the planar imaging of gamma cameras. ECT includes single-photon emission computed tomography (SPECT) and positron emission tomography (PET). SPECT uses single-photon-emitting radionuclides, such as 99mTc or 131I, which are relatively cost-effective and widely applied in clinical imaging.
Abnormal Thyroid Scintigraphy Findings
- Hot Nodules: Areas with higher 131I uptake than surrounding normal thyroid tissue, commonly seen in benign conditions such as autonomous thyroid adenomas, nodular goiter, and chronic lymphocytic thyroiditis.
- Warm Nodules: Areas with 131I uptake equivalent to normal thyroid tissue, often associated with nodular goiter.
- Cold Nodules: Areas with significantly lower or absent 131I uptake compared to normal thyroid tissue. Solitary cold nodules may indicate thyroid cancer.
Imaging of Thyroid Cancer Metastases
Whole-body imaging with ¹³¹I can help identify metastatic thyroid lesions, which usually show low iodine uptake. To enhance uptake in metastatic lesions, complete removal of thyroid tissue or administration of a large dose of ¹³¹I to ablate normal thyroid tissue is necessary. Subsequent whole-body imaging with ¹³¹I determines the location of metastases and evaluates their suitability for ¹³¹I therapy.
Bone Metastasis Imaging
Technetium-99m methylene diphosphonate (99mTc-MDP) is used as a bone imaging agent to detect bone metastases at an early stage.