The neck, located between the head and chest, has a cylindrical shape and serves as a connection between the head, trunk, and upper limbs. The anterior region of the neck houses the upper segments of the respiratory and digestive tracts, while the posterior region contains the cervical vertebrae and the upper thoracic vertebrae. On either side are major blood vessels and nerves. At the root of the neck lie the apex of the lung and the cupula of the pleura, along with obliquely oriented large blood vessels and nerves. The structures of the neck are separated by loose connective tissue, forming multiple fascial layers and fascial spaces. This arrangement enables a wide range of neck movements while maintaining the proper positioning and protection of muscles, blood vessels, and nerves during such motions. Additionally, the fascial layers and spaces serve as critical anatomical landmarks and help delineate boundaries within the neck, especially in surgical procedures.
Boundaries, Regions, and Triangles of the Neck
Boundaries of the Neck
The superior boundary is defined by the lower border of the mandible, the angle of the mandible, the tip of the mastoid process, the superior nuchal line, and the external occipital protuberance. The inferior boundary is marked by the suprasternal notch, sternoclavicular joints, clavicles, the acromion process, and the line connecting these points to the spinous process of the seventh cervical vertebra.
Regions and Triangles of the Neck
The trapezius muscle divides the neck into the anterolateral region and the posterior region. The anterolateral region is further divided by the sternocleidomastoid muscle into the anterior cervical region, sternocleidomastoid region, and lateral cervical region. Using additional boundaries such as the sternocleidomastoid muscle, digastric muscle, and omohyoid muscle, the anterolateral region is subdivided into the following triangles:
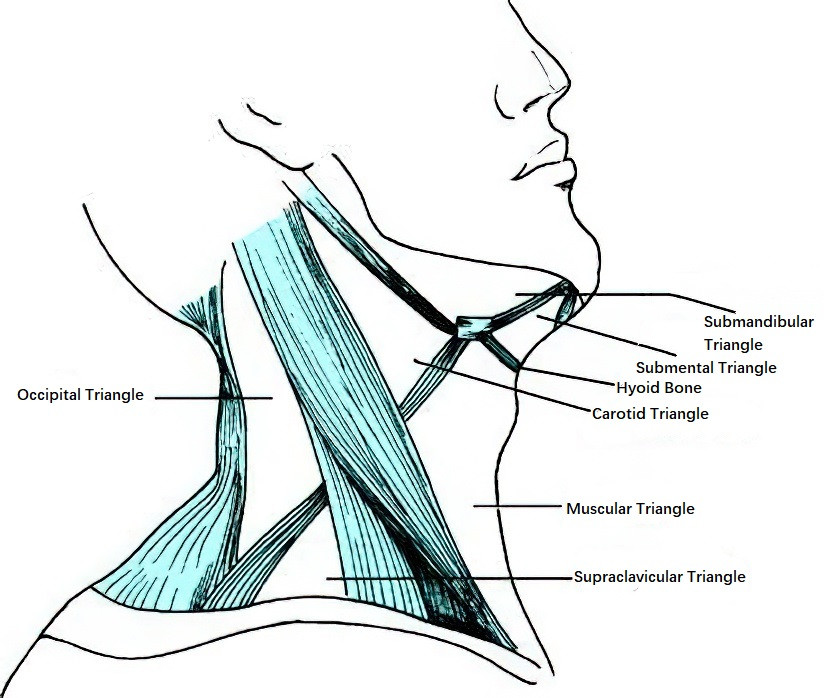
Figure 1 Cervical triangles
Submental Triangle
Located between the anterior bellies of the digastric muscles on either side and the hyoid bone.
Submandibular Triangle
Located between the anterior and posterior bellies of the digastric muscle and the lower border of the mandible.
Carotid Triangle
Bounded by the anterior border of the sternocleidomastoid muscle, the posterior belly of the digastric muscle, and the superior belly of the omohyoid muscle.
Muscular Triangle
Bounded by the anterior border of the sternocleidomastoid muscle, the midline of the anterior neck, and the superior belly of the omohyoid muscle.
Supraclavicular Triangle
Located between the posterior border of the sternocleidomastoid muscle, the inferior belly of the omohyoid muscle, and the clavicle.
Occipital Triangle
Bounded by the posterior border of the sternocleidomastoid muscle, the inferior belly of the omohyoid muscle, and the anterior border of the trapezius muscle.
Important Anatomical Landmarks, Major Blood Vessels, and Nerve Surface Projections
Important Anatomical Landmarks of the Neck
The sternocleidomastoid muscle, located in the lateral cervical region, is the most important muscular landmark for surgical anatomy. Palpable bony or cartilaginous landmarks in the anterior cervical region, from superior to inferior, include the hyoid bone, thyroid cartilage, cricoid cartilage, cervical trachea, and suprasternal notch. The sternoclavicular joints and the trapezius muscle in the posterior region of the neck are also key anatomical landmarks.
Surface Projections of Major Blood Vessels and Nerves
Common Carotid Artery (CCA) and External Carotid Artery (ECA)
The projection line extends from the sternoclavicular joint, along the anterior border of the sternocleidomastoid muscle, to the midpoint between the mastoid process and the angle of the mandible. The segment of the line below the superior border of the thyroid cartilage corresponds to the CCA, while the segment above this point corresponds to the ECA.
Internal Carotid Artery (ICA)
The projection begins at the plane of the superior border of the thyroid cartilage and continues along the anterior border of the sternocleidomastoid muscle to the posterior border of the mandibular condyle.
Internal Jugular Vein (IJV)
The projection is a line from the earlobe along the anterior border of the sternocleidomastoid muscle to the medial end of the clavicle. This line runs parallel to, but lateral to, the projection of the common carotid artery.
Accessory Nerve (CN XI)
The projection is a line connecting the junction of the upper and middle thirds of the sternocleidomastoid muscle's anterior border to the junction of the middle and lower thirds of the trapezius muscle's anterior border.
Brachial Plexus
The projection is slightly medial to the line connecting the junction of the middle and lower thirds of the sternocleidomastoid muscle's posterior border to the junction of the medial and lateral thirds of the clavicle.
Cervical Plexus
The cutaneous branches of the cervical plexus emerge near the midpoint of the posterior border of the sternocleidomastoid muscle, a key landmark for performing nerve block anesthesia during surgery.
Apex of the Lung and Cupula of the Pleura
The apex of the lung and the cupula of the pleura lie above the medial third of the clavicle, in the region between the sternal and clavicular heads of the sternocleidomastoid muscle. The highest point is approximately 2–3 cm above the superior border of the clavicle.
Muscles of the Neck
Sternocleidomastoid Muscle
The sternocleidomastoid muscle runs obliquely along both sides of the neck. Its lower end consists of two heads: one originates from the anterior surface of the manubrium of the sternum, and the other from the medial one-third of the clavicle. These two heads merge upward to form the sternoclavicular end. From this point, the muscle extends obliquely upward and posteriorly, inserting onto the lateral surface of the mastoid process and the lateral portion of the superior nuchal line. The external jugular vein courses obliquely downward along the superficial surface, while the carotid sheath lies deep to the muscle. The sternocleidomastoid muscle is innervated by the accessory nerve and the anterior rami of the second and third cervical nerves. Its function includes lateral flexion of the head toward the same side and rotation of the face toward the opposite side when one side contracts. When both sides contract simultaneously, the head tilts backward.
Suprahyoid and Infrahyoid Muscle Groups
These muscle groups are located above and below the hyoid bone, respectively, and play a role in the movement and stabilization of the neck and oral cavity structures.
Deep Muscles of the Neck
The deep muscles of the neck are divided into medial and lateral groups:
- Medial Group of Deep Neck Muscles: This group includes the longus capitis and longus colli muscles, which are located anterior to the cervical spine and collectively referred to as prevertebral muscles.
- Lateral Group of Deep Neck Muscles: This group includes the anterior, middle, and posterior scalene muscles. All originate from the transverse processes of cervical vertebrae and insert on the ribs. The space between the anterior and middle scalene muscles and the first rib is known as the scalene triangle, within which the brachial plexus and subclavian artery pass. The phrenic nerve courses along the surface of the anterior scalene muscle, and the subclavian vein runs anteriorly and inferiorly near the rib margin of the same muscle.
Cervical Fascia and Fascial Spaces
The cervical fascia is composed of dense connective tissue, which envelops the muscles, nerves, blood vessels, and organs of the neck, while forming several potential spaces between fascial layers. These spaces contain small amounts of loose connective tissue, facilitating significant movement between adjacent fascial layers without disrupting the structural integrity of the neck. This provides an anatomical basis for the high mobility of the neck. The cervical fascia also helps limit the spread of infections or tumors to a certain extent, although pathological processes breaching the fascia can potentially spread rapidly through fascial spaces. Understanding the anatomy and relationships of cervical fascia and spaces is critical for comprehending the extent of cervical infections, their potential pathways of spread, and principles of treatment. It also aids in accurate identification of anatomical structures during surgery, minimizing unnecessary tissue damage and bleeding.
The cervical fascia is classified into superficial and deep layers, the latter of which is further divided into superficial, middle, and deep layers.

Figure 2 Cervical fascia
Superficial Cervical Fascia
As part of the superficial fascia of the entire body, this layer lies deep to the subcutaneous tissue of the neck and envelops the entire neck. In the anterior cervical region, it contains the platysma muscle.
Deep Cervical Fascia
The deep cervical fascia is subdivided into three layers:
Superficial Layer of Deep Cervical Fascia
Also known as the investing fascia, this layer extends upward and downward, continuous with the investing fascia of the head, face, chest, and back, and forms a surrounding sheath for the neck. It encloses the sternocleidomastoid muscle, trapezius muscle, and infrahyoid muscle groups, forming their individual muscle sheaths. Above the hyoid bone, the fascia also surrounds the submandibular and parotid glands, forming their capsules. At the midline of the anterior neck, it forms the "white line of the neck," a vascular-poor area that appears white in color and is often utilized as an entry point for neck surgeries.
Middle Layer of Deep Cervical Fascia
Also known as the visceral fascia, it consists of a visceral layer and a parietal layer. The visceral layer adheres to the surfaces of organs such as the thyroid gland, larynx, trachea, pharynx, and esophagus, while the parietal layer folds back around these organs, creating potential spaces between the two. This fascial layer also envelops the common carotid artery, internal jugular vein, and vagus nerve, forming the carotid sheath.
Deep Layer of Deep Cervical Fascia
Also known as the prevertebral fascia, it covers the anterior surface of the vertebral bodies and the prevertebral muscles. It creates the prevertebral space between the fascia and the vertebral bodies. This fascia extends laterally to the transverse processes and the anterior surfaces of the scalene muscles. Laterally, it envelops the subclavian vessels and brachial plexus, forming the axillary sheath, which extends into the axilla. Superiorly, it attaches to the skull base posterior to the jugular foramen, and inferiorly, it extends to the cervicothoracic junction.
Fascial Spaces of the Neck
The cervical fascial layers form potential spaces between them, containing small amounts of loose connective tissue. These spaces are prone to abscess formation during infections when resistance decreases. Based on their relationship with the hyoid bone, these spaces are categorized into suprasternal spaces, infrahyoid spaces, and spaces occupying the entire length of the neck.
Suprasternal Spaces
These include the sublingual space, submandibular space, parapharyngeal space, peritonsillar space, masseteric space, and parotid space. Among these, the parapharyngeal space and peritonsillar space have higher infection rates.
Infrahyoid Space
Also known as the pretracheal space, this space is formed between the visceral and parietal layers of the middle layer of deep cervical fascia in front of the trachea. It is closely adjacent to the esophagus posteriorly, reaches the carotid sheaths bilaterally, and communicates inferiorly with the anterior mediastinum. Infections here can potentially spread downward into the anterior mediastinum.
Spaces Occupying the Entire Length of the Neck
Prevertebral Space
Located between the prevertebral fascia and the cervical vertebrae, this space may harbor cold abscesses resulting from tuberculosis of the cervical spine.
Carotid Sheath
Formed by the middle layer of deep cervical fascia, this sheath contains the common carotid artery, internal jugular vein, and vagus nerve.
Retropharyngeal Space
Positioned posterior to the pharynx and anterior to the prevertebral fascia, this space is a potential site for deep infections that may spread to the mediastinum.
Cervical Blood Vessels
Common Carotid Artery
The common carotid artery is the primary artery supplying the head and neck. On the right side, it originates from the brachiocephalic artery, while on the left side, it arises from the aortic arch. Both arteries pass posterior to the sternoclavicular joint and ascend along the deep surface of the anterior border of the sternocleidomastoid muscle, running obliquely upward and posteriorly along the lateral side of the trachea and larynx. At the level of the superior border of the thyroid cartilage, each bifurcates into the internal carotid artery and the external carotid artery. The internal jugular vein is positioned laterally to the common carotid artery, with the vagus nerve located posteriorly. All three are enclosed within the carotid sheath.
Internal Carotid Artery (ICA)
After branching from the common carotid artery, the internal carotid artery ascends on the lateral and posterior side of the external carotid artery and then courses medially and posteriorly to it. It runs along the lateral wall of the pharynx and the anterior side of the prevertebral fascia, extending vertically upward to the base of the skull. It enters the cranial cavity through the carotid canal and passes through the cavernous sinus via the carotid groove on either side of the sphenoid body. Within the brain, it gives off the ophthalmic artery, anterior cerebral artery, and middle cerebral artery, providing blood primarily to most parts of the brain and the visual apparatus. Notably, the internal carotid artery has no branches within the cervical region.
Carotid Body and Carotid Sinus
The carotid body is located posterior to the bifurcation of the internal and external carotid arteries and is attached to the arterial wall by connective tissue. It functions as a chemoreceptor, sensing changes in carbon dioxide concentration in the blood and reflexively regulating respiratory activity. The carotid sinus, a dilated portion at the origin of the internal carotid artery, contains specialized sensory nerve endings and functions as a baroreceptor. When arterial blood pressure increases, the carotid sinus expands, stimulating the baroreceptors. This triggers reflex nerve impulses at the central level, resulting in a slowing of the heart rate and dilation of peripheral blood vessels, thereby contributing to blood pressure regulation.
External Carotid Artery
The external carotid artery branches off the common carotid artery and initially lies medial to the internal carotid artery. It subsequently courses laterally and ascends, passing deep to the posterior belly of the digastric muscle and the stylohyoid muscle. At the level of the neck of the mandible, it passes through the parotid gland and divides into its two terminal branches: the superficial temporal artery and the maxillary artery. Along its course, the major branches of the external carotid artery include the thyroid superior artery, lingual artery, and facial artery (anterior branches); the occipital artery and posterior auricular artery (posterior branches); the ascending pharyngeal artery (an upward branch); and the terminal branches, namely the superficial temporal artery and maxillary artery. These branches primarily supply the neck, face, dura mater, and cranium.
Internal Jugular Vein
The internal jugular vein begins at the jugular foramen as the continuation of the sigmoid sinus. Immediately after exiting the skull, it enters the carotid sheath, initially positioned posterior to the internal carotid artery and then located laterally to it. It descends along the lateral side of the common carotid artery and joins the subclavian vein at its inferior end to form the brachiocephalic vein. Just below the greater horn of the hyoid bone, the internal jugular vein receives tributaries such as the common facial vein and lingual vein. At the level of the superior border of the thyroid cartilage, it also receives tributaries from the superior thyroid vein.
Cervical Nerves
Cervical Plexus
The cervical plexus is formed by the anterior rami of the first to fourth cervical nerves. It is situated deep to the sternocleidomastoid muscle and the prevertebral fascia, and superficial to the middle scalene and levator scapulae muscles. The cervical plexus gives off both cutaneous and muscular branches. The major cutaneous branches include the lesser occipital nerve, great auricular nerve, transverse cervical nerve, and supraclavicular nerves, which innervate the skin of the occipital region, areas around the auricle, the anterior neck, and the clavicular region. These branches emerge from the midpoint of the posterior border of the sternocleidomastoid muscle, a site often used for nerve block anesthesia during neck surgeries. The muscular branches include the descending cervical nerve and the phrenic nerve, which supply the deep neck muscles, levator scapulae, infrahyoid muscles, and the diaphragm.
Phrenic Nerve
The phrenic nerve arises from the muscular branches of the cervical plexus. It descends from the lateral side of the upper part of the anterior scalene muscle, runs along its anterior surface, and courses medially between the subclavian artery and vein before entering the mediastinum to reach the diaphragm. Phrenic nerve injury primarily results in diaphragmatic paralysis, leading to weakened or absent abdominal breathing. Stimulation of the phrenic nerve may result in hiccups.
Brachial Plexus
The brachial plexus is formed by the anterior rami of the fifth to eighth cervical nerves and the first thoracic nerve. It emerges from the interscalene space and subsequently forms the superior, middle, and inferior trunks. Each trunk splits into anterior and posterior divisions: the anterior divisions of the superior and middle trunks form the lateral cord; the anterior division of the inferior trunk forms the medial cord; and the posterior divisions of all three trunks combine to form the posterior cord. The cords converge around the axillary artery near the midpoint of the clavicle as they enter the axilla. Major branches of the brachial plexus include the long thoracic nerve, thoracodorsal nerve, anterior thoracic nerves, musculocutaneous nerve, and median nerve, which supply the chest, shoulder, neck, and upper limb. The brachial plexus is relatively superficial and concentrated above the midpoint of the clavicle, making it a common site for conduction block anesthesia in clinical settings.
Cervical Sympathetic Nerve
The cervical sympathetic nerve is located posterior to the carotid sheath and anterior to the transverse processes of the cervical vertebrae. It extends superiorly to below the mastoid process and inferiorly to the first rib. Each side contains three sympathetic ganglia: superior, middle, and inferior. The superior cervical ganglion is the largest and spindle-shaped, located anterior to the transverse processes of the second and third cervical vertebrae. Its major branches include the internal carotid nerve plexus, which enters the cavernous sinus alongside the internal carotid artery. At the internal carotid artery's opening, the nerve plexus gives rise to the deep petrosal nerve, which joins the nerve of the pterygoid canal and reaches the pterygopalatine ganglion to innervate glands and blood vessels of the mouth and nasal mucosa. Within the cavernous sinus, it also gives off branches that pass through the superior orbital fissure to the orbit, innervating the dilator pupillae and the smooth muscles of the upper and lower eyelids. The middle cervical ganglion is the smallest and often absent, located anterior to the transverse process of the sixth cervical vertebra. The inferior cervical ganglion, irregularly shaped, is situated anterior to the transverse process of the seventh cervical vertebra and the first rib cartilage, posterior to the subclavian artery, and often fuses with the first thoracic ganglion to form the stellate ganglion. Damage or compression of the cervical sympathetic nerve due to trauma or tumors can result in Horner syndrome, characterized by ptosis, miosis, ipsilateral facial vasodilation, and anhidrosis.
Glossopharyngeal Nerve
The glossopharyngeal nerve, a mixed cranial nerve, exits the skull via the jugular foramen. It is composed of five types of nerve fibers:
- Special visceral motor fibers arising from the nucleus ambiguus, which innervate the stylopharyngeus muscle.
- General visceral motor fibers originating from the inferior salivatory nucleus, which control secretions from the parotid gland.
- Special visceral sensory fibers responsible for taste sensation from the posterior one-third of the tongue.
- General visceral sensory fibers, which innervate the mucosa of the pharynx, posterior one-third of the tongue, eustachian tube, and tympanic cavity.
- General somatic sensory fibers, which are few in number and play a minor role in the nerve's overall function.
Vagus Nerve
The vagus nerve emerges from the posterolateral aspect of the medulla oblongata and exits the skull through the jugular foramen. It descends in the carotid sheath posterior to the internal carotid artery and internal jugular vein. Near the greater horn of the hyoid bone, it gives off the superior laryngeal nerve, which divides into internal and external branches. The internal branch travels alongside the superior laryngeal artery, passes through the thyrohyoid membrane into the larynx, and provides sensory innervation to the mucosa above the glottis. The external branch is smaller and innervates the cricothyroid muscle. The vagus nerve then continues downward, entering the thoracic cavity where it gives rise to the recurrent laryngeal nerve. The course of the recurrent laryngeal nerve differs on each side: on the right, it loops around the subclavian artery, while on the left, it loops around the aortic arch. Both ascend along the tracheoesophageal groove and enter the larynx posterior to the cricothyroid joint, providing motor innervation to all intrinsic laryngeal muscles except the cricothyroid muscle and sensory innervation to the mucosa below the glottis.
Accessory Nerve
The accessory nerve consists of a cranial root and a spinal root. The cranial root exits the skull via the jugular foramen and merges with the vagus nerve to innervate the striated muscles of the pharynx and larynx. The spinal root exits the skull and descends anterolaterally along the internal jugular vein. It then courses downward along the deep surface of the sternocleidomastoid muscle, emerging near the midpoint of its posterior border. It travels obliquely downward and outward between the superficial layer of the deep cervical fascia and the prevertebral fascia, reaching the deep surface of the trapezius muscle at the junction of its middle and lower thirds. The accessory nerve provides motor innervation to the sternocleidomastoid and trapezius muscles and is surrounded along its course by deep cervical lymph nodes.
Hypoglossal Nerve
The hypoglossal nerve is the motor nerve of the tongue muscles. It arises from the hypoglossal nucleus and exits the skull through the hypoglossal canal, descending between the internal carotid artery and internal jugular vein lateral to the vagus nerve. It courses around the anterior surface of the internal and external carotid arteries and enters the submandibular space deep to the posterior belly of the digastric muscle. Within the submandibular gland, it ascends anteriorly and superiorly to reach the tongue, innervating all intrinsic muscles and some extrinsic muscles of the tongue. Damage to one hypoglossal nerve results in tongue deviation toward the affected side upon protrusion and atrophy of the ipsilateral tongue muscles.
The glossopharyngeal nerve, vagus nerve, accessory nerve, and hypoglossal nerve are collectively referred to as the posterior cranial nerves. Lesions near the jugular foramen, such as those caused by nasopharyngeal carcinoma or trauma, may result in posterior cranial nerve symptoms involving the glossopharyngeal, vagus, and accessory nerves.
Cervical Lymph Nodes
Cervical lymph nodes are categorized into five major groups: submental lymph nodes, submandibular lymph nodes, anterior cervical lymph nodes, superficial cervical lymph nodes, and deep cervical lymph nodes.
Submental Lymph Nodes
These lymph nodes are located within the submental triangle and typically consist of 2–3 nodes. They primarily collect lymph from the chin, tip of the tongue, and mandibular incisors, with their efferent vessels draining into the submandibular lymph nodes.
Submandibular Lymph Nodes
These lymph nodes are situated in the submandibular triangle and consist of 4–6 nodes. They collect lymph from the cheek, gums, anterior tongue, submental area, and other surrounding regions, and primarily drain into the upper deep cervical lymph nodes.
Anterior Cervical Lymph Nodes
These lymph nodes are divided into superficial and deep groups. The superficial group follows the anterior jugular vein, while the deep group is located around the larynx, cricothyroid membrane, and anterior trachea. They collect lymph from the larynx, trachea, thyroid gland, and adjacent structures. Their efferent vessels drain into the lower deep cervical lymph nodes.
Superficial Cervical Lymph Nodes
These lymph nodes are located on the superficial surface of the sternocleidomastoid muscle and aligned along the external jugular vein. They collect lymph from the occipital region, ears, and parotid area and drain into the upper deep cervical lymph nodes.
Deep Cervical Lymph Nodes
These lymph nodes lie deep to the sternocleidomastoid muscle and are arranged along the internal jugular vein. They are divided into upper and lower deep cervical lymph nodes, demarcated at the point where the omohyoid muscle crosses the internal jugular vein.
Upper Deep Cervical Lymph Nodes
These nodes collect lymph from the nasopharynx, palatine tonsils, tongue, submental lymph nodes, and submandibular lymph nodes and drain into the lower deep cervical lymph nodes.
Lower Deep Cervical Lymph Nodes
These nodes may extend around the subclavian artery, brachial plexus, and transverse cervical artery. The nodes in this region are referred to as supraclavicular lymph nodes. The lower deep cervical lymph nodes primarily collect lymph from the cervical region and, additionally, from parts of the thorax and upper abdomen. Their efferent vessels on the left side drain into the thoracic duct, while those on the right side drain into the right lymphatic duct or directly into the internal jugular vein. Malignant tumor cells in the thoracic or abdominal regions may retrogradely metastasize via the thoracic duct to the supraclavicular lymph nodes. Malignant tumors in the abdomen and the left thoracic region often metastasize to the left supraclavicular lymph nodes, while tumors in the right thoracic region primarily metastasize to the right supraclavicular lymph nodes.
Thyroid and Parathyroid Glands
Thyroid Gland
The thyroid gland is H-shaped and reddish-brown, consisting of two lateral lobes and an isthmus. The lateral lobes are pyramidal in shape and lie on the lateral surfaces of the larynx and trachea, extending from the middle of the thyroid cartilage superiorly to the sixth tracheal ring inferiorly. The medial surfaces of the lateral lobes are attached to the cricoid cartilage via lateral ligaments, allowing the thyroid gland to move with the larynx during swallowing. The isthmus connects the two lateral lobes and is located anteriorly to the second through fourth tracheal rings. In some cases, a pyramidal lobe extends upward from the isthmus. The thyroid gland is covered by two layers of connective tissue: the outer layer, known as the false thyroid capsule, is formed by the pretracheal fascia, and the inner layer, known as the true thyroid capsule, closely adheres to the glandular tissues and extends into the substance of the gland, dividing it into lobules.
The thyroid gland has a rich blood supply, with three pairs of arteries and three pairs of veins. The arteries are interconnected, and the veins form a plexus on the glandular surface, featuring arteriovenous anastomoses within the gland.
- Superior Thyroid Artery: This artery typically originates from the external carotid artery at the level of the superior border of the thyroid cartilage. It courses anteromedially and inferiorly to the upper end of the lateral lobe, where it branches into anterior and posterior divisions that enter the gland. The external branch of the superior laryngeal nerve runs close to this artery before it enters the thyroid, necessitating precise ligation of the artery during thyroid surgery to avoid damaging the nerve.
- Inferior Thyroid Artery: This artery typically arises from the thyrocervical trunk. It ascends to just below the sixth cervical vertebra and then turns medially, crossing posterior to the carotid sheath and sympathetic trunk before reaching the posterior surface of the thyroid gland and giving off branches to the gland.
- Thyroid Ima Artery: This artery is less common and usually arises from the aortic arch or brachiocephalic trunk. It ascends anterior to the trachea to supply the isthmus of the thyroid gland.
- Thyroid Veins: Venous drainage of the thyroid is via a venous plexus on its anterior surface, which forms the superior, middle, and inferior thyroid veins. The superior thyroid vein drains the upper pole of the thyroid gland and runs alongside the superior thyroid artery, emptying into the internal jugular vein or facial vein. The middle thyroid vein collects blood from the middle and lower thirds of the lateral lobe and drains into the internal jugular vein. The inferior thyroid vein drains the lower poles of the thyroid gland and empties into the brachiocephalic vein.
Parathyroid Glands
The parathyroid glands are small, flattened, ovoid structures that vary in color from pale red to brownish-yellow. Resembling soybeans or rice grains, they have a smooth surface and are surrounded by a thin fibrous capsule. The number of parathyroid glands varies, but there are typically two pairs. The superior parathyroid glands are usually located near the junction of the upper and middle thirds of the posterior surface of the lateral lobes of the thyroid gland, while the inferior parathyroid glands are generally situated on the posterior and lateral surfaces near the lower poles of the thyroid gland.