Before examining the larynx, it is necessary to inquire about the patient's medical history to assess for symptoms such as hoarseness, breathing difficulty, or throat pain. Observations should include the presence of inspiratory retraction signs and stridor during inhalation. A systemic medical history should also be obtained. In urgent situations such as laryngeal obstruction, a preliminary diagnosis should be made based on a concise patient history, symptoms, and signs, followed by decisive interventions, such as tracheotomy, to alleviate breathing difficulties and save the patient's life. After stabilizing the situation, further laryngeal examinations should be conducted as appropriate.
Examinations of the larynx include external examination of the larynx, indirect laryngoscopy, fiberoptic and electronic laryngoscopy, direct and rigid laryngoscopy, dynamic laryngoscopy, imaging studies, voice analysis, and laryngeal electromyography.
External Examination of the Larynx
External examination primarily involves inspection and palpation. Inspection focuses on signs such as inspiratory retraction of soft tissues—specifically in the suprasternal fossa, supraclavicular fossa, and subxiphoid area—respiration rate, and the duration of inhalation. The alignment of the thyroid cartilage at the midline of the neck and its symmetry on both sides should also be observed.
Palpation involves examining the thyroid cartilage, cricoid cartilage, cricothyroid space, and checking for cervical lymph node enlargement. The thyroid cartilage should be grasped on both sides and moved side-to-side while applying slight pressure to generate friction against the cervical spine, which normally produces a friction sound. If the friction sound is absent, it may indicate the presence of a tumor in the post-cricoid region.
Palpation is also critical during procedures such as tracheotomy. The cricoid arch should first be located, and an incision should then be made between the lower edge of the cricoid arch and the suprasternal fossa. For cricothyrotomy, the cricothyroid space should be palpated in advance.
Indirect Laryngoscopy
Indirect laryngoscopy has been used for over a century and remains the most commonly employed and straightforward method for examining the larynx. This procedure requires an indirect mirror and a headlamp.
During the examination, the patient sits upright, opens their mouth, and extends their tongue. The examiner, seated opposite the patient, first adjusts the reflection of light from the headlamp onto the uvula. The tongue is then held by wrapping its anterior third with gauze, and the anterior portion of the tongue is gently pulled forward and downward using the examiner's thumb and middle finger, with the index finger supporting the upper lip.
The indirect mirror is heated slightly over an alcohol lamp to prevent fogging during the procedure, and the temperature is checked on the examiner’s hand before use to ensure it is not too hot. The mirror is then placed into the oropharynx, with the reflective surface angled downward and forward, while the back of the mirror pushes the uvula and soft palate upward and backward.
The base of the tongue, vallecula, lingual surface of the epiglottis, posterior pharyngeal wall, and lateral walls are inspected first. The patient is asked to produce an "e" sound, which raises the epiglottis and exposes the glottis. At this stage, the laryngeal surface of the epiglottis, aryepiglottic folds, vestibular folds, vocal cords, interarytenoid region, and subglottic space can be examined. Occasionally, the upper rings of the tracheal cartilage may also be visible. Movement of the vocal cords can be observed: adduction during phonation and abduction during inhalation.
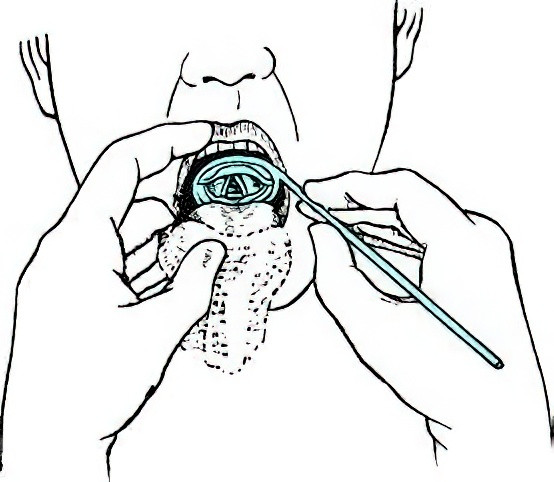
Figure 1 Indirect laryngoscopy
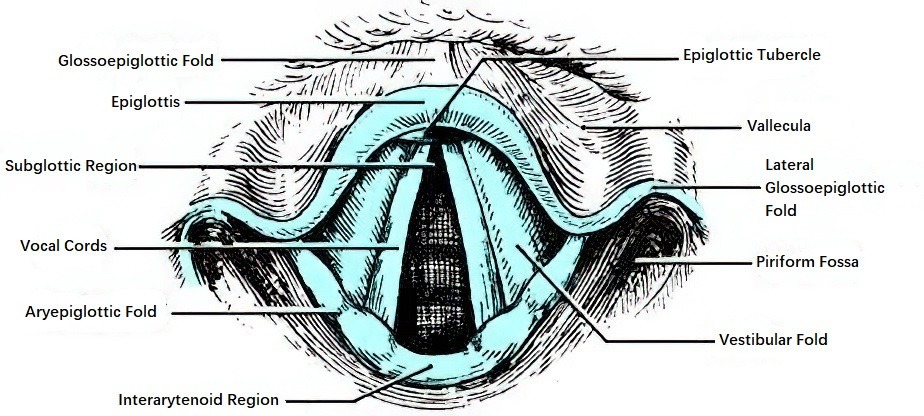
Figure 2 Normal laryngeal view observed via indirect laryngoscopy

Figure 3 Vocal cord adduction during phonation

Figure 4 Vocal cord abduction during inspiration
Under normal conditions, the structures of the hypopharynx and larynx appear symmetric. The mucosa of the piriform recess is pale pink, smooth, and without fluid accumulation. The vocal cords are white and symmetric in movement. The mucosa of the arytenoid region shows no signs of edema.
Most patients tolerate indirect laryngoscopy well; however, those with a sensitive gag reflex may require local anesthesia of the oropharyngeal mucosa to complete the examination. Common anesthetics include 1% tetracaine solution or 2% lidocaine solution. If anesthesia does not facilitate indirect laryngoscopy, or if epiglottic curvature obstructs the view, fiberoptic or electronic laryngoscopy can be considered.
Fiberoptic and Electronic Laryngoscopy
The fiberoptic laryngoscope is a flexible endoscope made from optical glass fibers. It has advantages such as flexibility, strong illumination, and a wide field of view. After local anesthesia is applied to the nasal cavity, oropharyngeal, and hypopharyngeal mucosa, the fiberoptic laryngoscope is inserted through the nasal passage and advanced through the nasopharynx and oropharynx to reach the hypopharynx. This approach allows examination of the hypopharynx and larynx, as well as procedures such as biopsy, polypectomy, or removal of foreign objects.
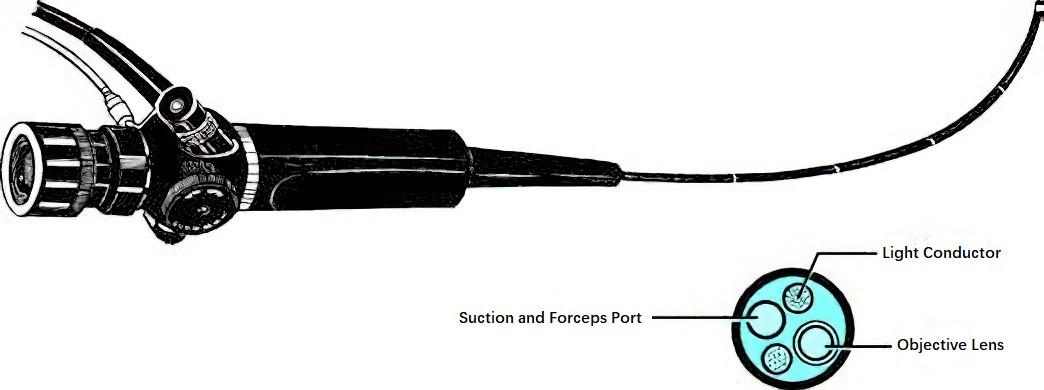
Figure 5 Fiberoptic laryngoscope
The electronic video laryngoscope is a newer type of flexible endoscope that resembles the fiberoptic laryngoscope in appearance but provides significantly improved image quality. Utilizing a charge-coupled device (CCD) and its imaging principles, the electronic laryngoscope offers several advantages:
- High-resolution imaging.
- The ability to lock instant images. Using an image-lock button on the device handle, selected images can be captured in real-time, similar to taking photographs.
- Compatibility with computers, allowing locked images to be saved digitally for later review or printed using a color printer for inclusion in diagnostic reports.
Due to its rigid design, the electronic laryngoscope is generally not recommended for use in infants or must be used with particular caution when examining this population.
Direct Laryngoscopy and Suspension Laryngoscopy
With the widespread adoption of fiberoptic and electronic laryngoscopy, the use of direct laryngoscopy has become less common. However, it still holds value in certain situations, such as introducing a bronchoscope during pediatric bronchoscopic examinations or removing specific types of foreign bodies from the larynx. Direct laryngoscopy is typically performed under local anesthesia, although general anesthesia may be necessary for uncooperative patients.
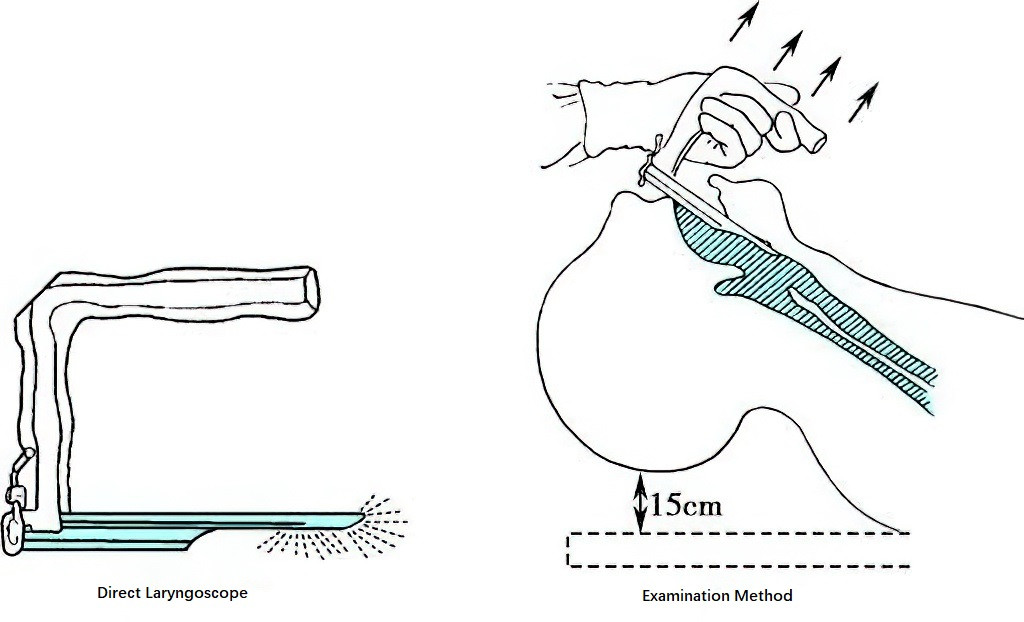
Figure 6 Direct laryngoscopy
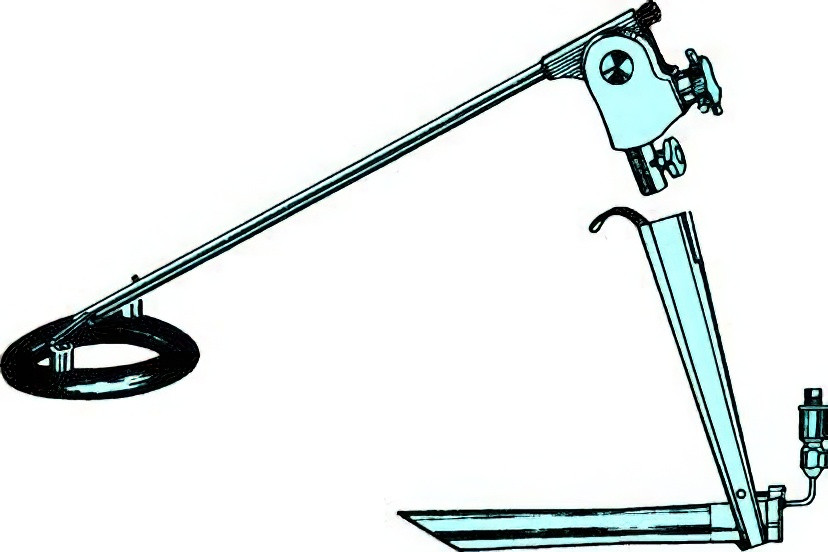
Figure 7 Suspension laryngoscope
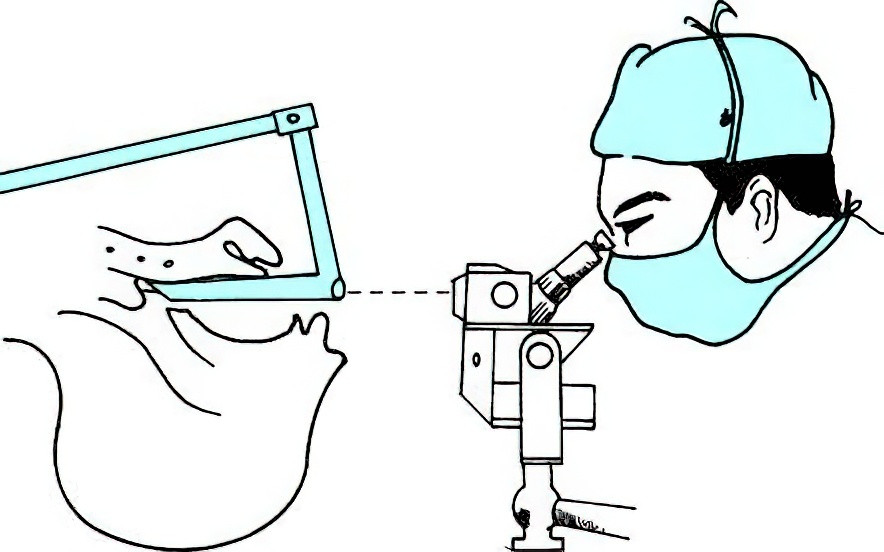
Figure 8 Examination method using a microsurgical suspension laryngoscope
Suspension laryngoscopy is an advancement of direct laryngoscopy, utilizing a suspension frame attached to the direct laryngoscope. This configuration eliminates the need for continuous manual holding to expose the glottis, providing a stable and prolonged view. Suspension laryngoscopy is commonly conducted under general anesthesia, accompanied by cold light illumination and the use of a surgical microscope to observe laryngeal lesions. This setup enhances the precision of the diagnosis and the accuracy of surgical procedures.
Dynamic Laryngoscopy
Dynamic laryngoscopy, also known as stroboscopic laryngoscopy, employs strobe light at varying frequencies directed at the vocal cords to observe vocal cord vibrations and mucosal waves during phonation. When the frequency of the strobe light matches the frequency of vocal cord vibrations, the vocal cords appear stationary. If there is a discrepancy between the strobe light and vocal cord vibration frequencies, a slow-motion effect is observed, allowing visualization of the mucosal wave along with vocal cord movement.
In cases of epithelial hyperplasia, small cysts, or malignancy on the vocal cords, dynamic laryngoscopy can detect abnormalities that may not be evident with other examination methods. Such lesions often present reduced or absent mucosal waves and irregular vocal cord vibrations, providing clues to the depth and potential nature of the pathology.
Imaging Studies for the Larynx
Imaging studies play a crucial role in diagnosing laryngeal diseases. Commonly used methods include conventional X-rays, computed tomography (CT), and magnetic resonance imaging (MRI).
Conventional X-ray Examination
Anteroposterior and lateral X-ray images of the larynx are primarily used to diagnose the extent of laryngeal tumors or stenosis.
CT Scan
CT scans include both plain and contrast-enhanced imaging. Plain CT may reveal laryngeal cartilage fractures, dislocations, submucosal hematomas, mucosal tears, or post-traumatic airway obstruction in cases of laryngeal trauma. In tumor evaluations, CT provides information about the size of the tumor, the extent of invasion, cartilage involvement, and cervical lymph node metastasis. CT findings are instrumental in staging laryngeal cancer (TNM classification) and designing surgical treatment plans.
MRI
MRI offers better visualization of soft tissues than CT but is inferior to CT in displaying laryngeal cartilage. Presently, MRI is primarily used to evaluate tumor size and the extent of invasion. For example, on T1-weighted MRI, the presence of isointense soft tissue within the high-signal fat of the pre-epiglottic space suggests supraglottic laryngeal cancer invading this space. MRI is also more effective than CT in visualizing cervical lymph node metastases.
Other Diagnostic Methods for the Larynx
Acoustic Voice Assessment
Acoustic voice assessment instruments, developed in recent years with advances in computer technology, enable objective and quantitative analysis of voice characteristics. During this test, the patient produces a sustained "e" sound, which is captured via a microphone and analyzed by the assessment device. Parameters evaluated include:
- Fundamental frequency (F₀)
- Jitter, representing frequency variation in the fundamental frequency
- Shimmer, representing amplitude variation in the fundamental frequency
- Noise-to-harmonic ratio (NHR), indicating the degree of noise caused by air leakage during phonation
- Harmonics-to-noise ratio (HNR), representing the ratio of harmonic sound to noise in the voice signal
These parameters reflect the severity of voice disorders and provide a basis for voice assessment.
Laryngeal Electromyography (EMG)
Laryngeal EMG assesses the function of laryngeal nerves and intrinsic laryngeal muscles. This test involves inserting recording electrodes into specific intrinsic laryngeal muscles, and a myograph records both spontaneous and evoked potentials. This method helps determine the presence and severity of nerve or muscle damage in the larynx.
Narrow Band Imaging (NBI)
In human tissues, hemoglobin is the primary pigment within mucosal tissues. Hemoglobin absorbs blue light strongly while absorbing green light to a lesser extent. NBI technology filters ordinary light to release only blue and green light, thereby enhancing the contrast and clarity of mucosal microstructures and submucosal vessels. Endoscopes equipped with NBI systems can reveal minute mucosal lesions, facilitating the early detection and diagnosis of microcarcinomas or precancerous lesions in the larynx and pharynx. NBI is also useful in differentiating laryngitis from precancerous lesions or early-stage laryngeal cancer.