Examination of Respiratory Function
The respiratory function of the nasal cavity, including nasal airflow, resistance, and ventilation, along with olfactory function, is evaluated. In addition to routine anterior and posterior rhinoscopy, instrumental methods can also be employed.
Rhinomanometry
Also known as nasal resistance measurement, rhinomanometry evaluates nasal airflow and the corresponding nasal pressure during airflow. This method provides an objective, sensitive, and effective assessment of nasal ventilation. Nasal resistance is defined as the resistance under specific airflow and pressure conditions. Although the clinical application of rhinomanometry has certain limitations, it remains a valuable research tool.
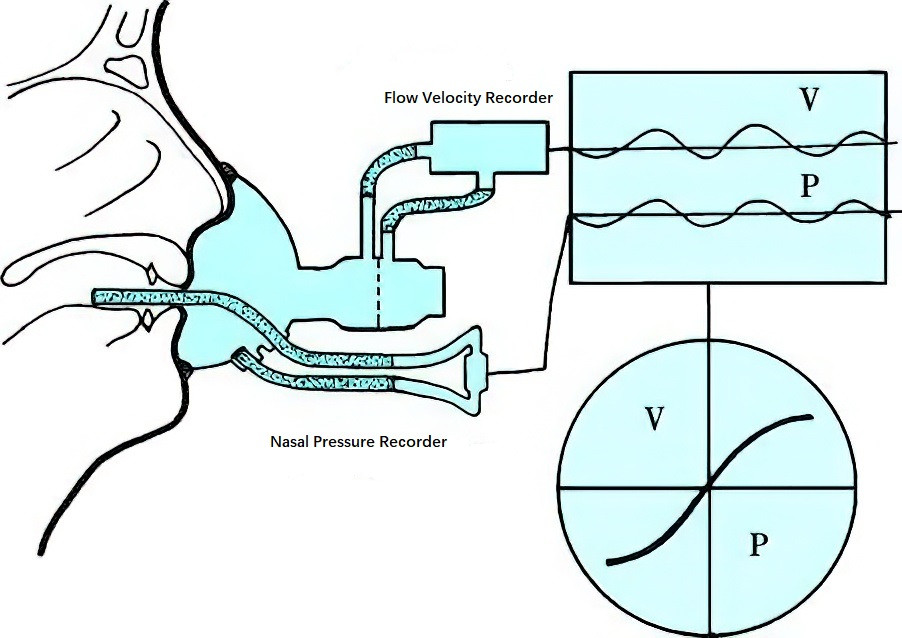
Figure 1 Rhinomanometry schematic diagram
V: Velocity; P: Pressure.
Acoustic Rhinometry
This technique measures the nasal cavity’s volume and cross-sectional area by analyzing the reflection of sound waves, which are converted into an area-distance graph that provides a "two-dimensional topography" of the nasal airway. As an objective measurement, acoustic rhinometry accurately reflects the geometric structure of the nasal cavity and can help determine whether nasal obstruction is caused by structural factors, mucosal factors, or both. It also allows assessment of the severity of obstruction based on reference values. The clinical application of acoustic rhinometry has increased, and it is now commonly used to evaluate both normal nasal passages and pathological conditions, as well as to compare pre- and post-operative conditions when combined with nasal endoscopy.
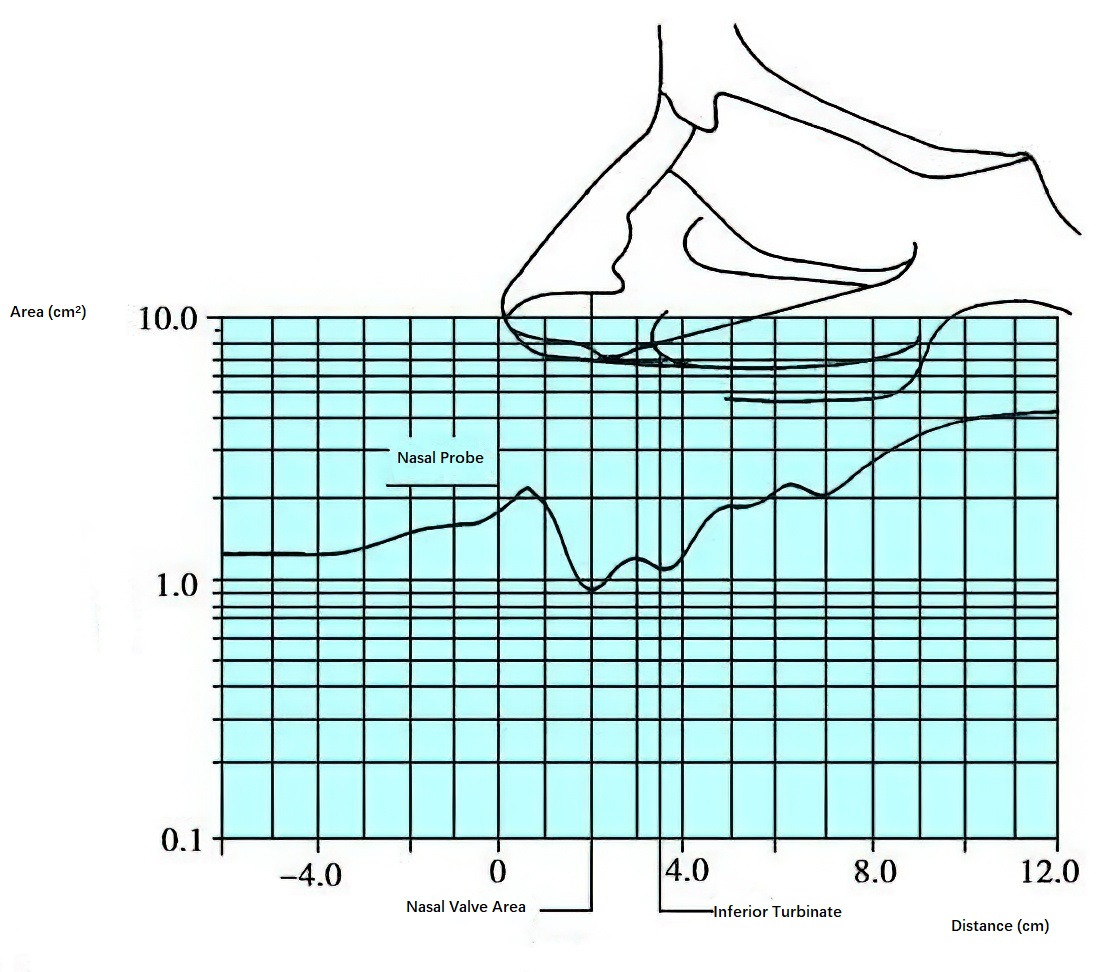
Figure 2 Acoustic rhinometry
Normal curve of acoustic rhinometry measurement.
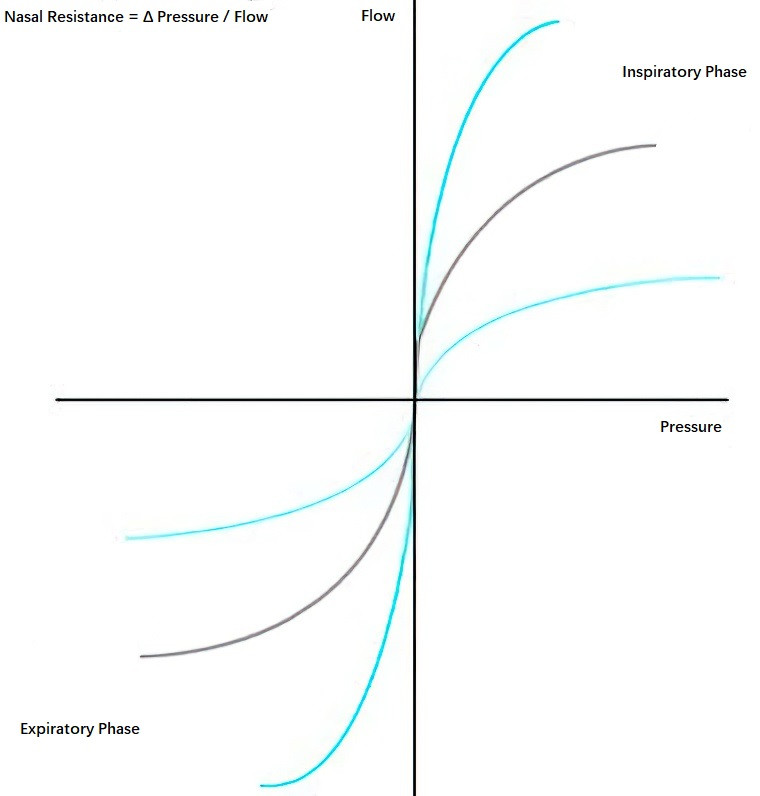
Figure 3 Quadrant diagram of nasal resistance measurement
Each curve of the same color represents the continuous measurement results for both the inspiratory and expiratory phases. The results of both nasal cavities are combined on the coordinate axis to form a quadrant diagram.
Nasal Mucociliary Clearance Test (NMCC)
This test comprehensively evaluates the ciliary function of the nasal mucosa and uses tracers such as soluble particles (e.g., saccharin), insoluble particles (e.g., activated charcoal), or radioactive isotopes. Currently, the saccharin test is the most widely used in vivo NMCC method. It records mucociliary clearance time (MCT) by measuring the length of the nasal cavity and calculating mucociliary clearance velocity (MCV). NMCC can be used to compare nasal mucosal function under physiological and pathological conditions.
Olfactory Examination
Olfactory function is assessed through subjective and objective methods.
Subjective Testing
Simple Method
This method assesses the presence of olfactory function by presenting various odorants (e.g., fragrances, vinegar, camphor oil, kerosene) placed in bottles of identical appearance. Patients are instructed to select a random bottle, block one nostril, and use the other nostril to detect and describe the odor. Each bottle is tested sequentially.
Smell Threshold Test
This test measures the minimum concentration of an odorant that can be detected by the majority of people, referred to as "olfactory units." Seven basic odorants are used: ether, camphor, musk, floral, peppermint, spicy, and putrid odors. These odorants are prepared in 10 concentrations for each, producing a total of 70 bottles ranging from olfactory units 1 to 10.
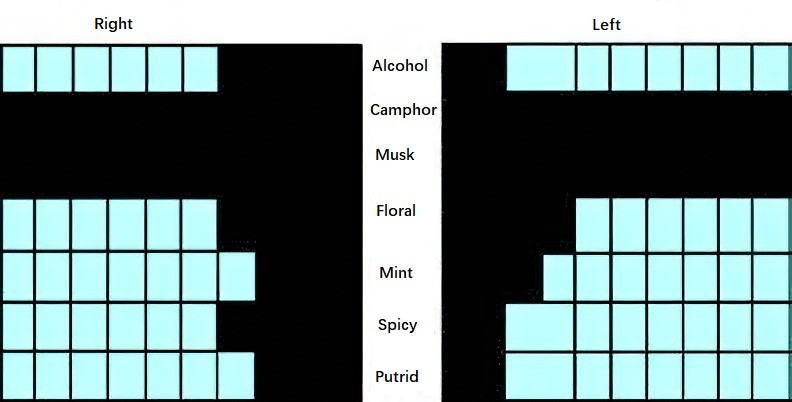
Figure 4 Olfactory spectrogram
Illustration showing anosmic bands for camphor and musk.
During the test, the lowest threshold for each of the seven substances is determined and recorded on a 7×10 grid, resulting in an olfactory spectrogram. If anosmia is detected for a specific odorant, a dark band on the spectrogram represents the odorant-specific anosmia zone.
Objective Testing
Olfactory evoked potentials (OEP) are recorded using a specialized OEP device that delivers odorants with controlled concentration, humidity, temperature, and flow to the olfactory region of the nasal cavity. According to the international 10/20 system for electrode placement, specific brain electrical activity changes are measured on the scalp. Both odorant and electrical pulse stimulation to the olfactory mucosa can elicit specific brain potentials, with those induced by odorants referred to as olfactory event-related potentials (OERP).
This method has been used clinically for diagnosing olfactory disorders, assessing olfactory levels, evaluating surgical outcomes, and aiding in the diagnosis of certain diseases associated with olfactory decline, such as olfactory neuroblastoma and Alzheimer’s disease.