Depending on the situation, patients may adopt a seated or semi-recumbent position. Typically, the examinee sits upright facing the examiner, with their upper body slightly leaned forward and their neck relaxed to allow the head position to be adjusted as needed. The head mirror is adjusted so that the focus of the light is concentrated on the area being examined. During history-taking, the examiner should differentiate whether the patient exhibits hypernasality (open nasal resonance) or hyponasality (closed nasal resonance) and assess whether exhalation produces an abnormal odor. Diseases of the nasal cavity and sinuses can interact with certain systemic conditions. Symptoms such as nasal itching, nasal obstruction, sneezing, rhinorrhea, impaired sense of smell, epistaxis, localized pain, or headache may often represent manifestations of systemic diseases involving the nasal region.
External Nose Examination
The shape of the external nose and nearby areas should be inspected for abnormalities (such as nasal deformities or narrowing of the anterior nostrils), skin color (e.g., localized redness in the early stages of rosacea), and movement (e.g., nasal wing collapse and a shallower nasolabial groove in cases of facial nerve paralysis). Necessary palpation may occasionally be performed, such as detecting nasal bone depression, displacement, and tenderness in nasal fractures; pronounced tenderness in nasal vestibulum inflammation; pressure points associated with sinusitis; or a "ping-pong ball-like" elastic sensation in cases of sinus cysts. It is also important to note whether the patient exhibits hypernasality or hyponasality.
Nasal Cavity Examination
Examination of the Nasal Vestibule
Manual Method
The nasal tip is raised using the thumb and gently moved sideways to observe the nasal vestibule using reflected light. Alternatively, anterior rhinoscopy can be performed, which is suitable for individuals with narrow nostrils or collapsed nasal wings.
Anterior Rhinoscopy
The leaves of the anterior rhinoscope are first closed and inserted into the nasal vestibule parallel to the nasal floor, ensuring that it does not extend beyond the nasal valve. The leaves of the rhinoscope are then gently opened upward and downward to lift the nasal wing and enlarge the anterior nasal aperture.

Figure 1 Method of using the anterior rhinoscope
The condition of the nasal vestibule should be examined, including the presence of redness, erosion, fissures, crusting, or nasal hair loss, which are commonly observed in nasal vestibulitis. Localized swelling with pronounced tenderness is often indicative of nasal vestibular furuncle, while swelling on the lower wall of the vestibule without tenderness is more likely a nasal vestibule cyst. Abnormal growths or papillomas in the nasal vestibule should also be noted.
Examination of the Nasal Cavity
Anterior Rhinoscopy
The examiner uses the anterior rhinoscope to enlarge the nasal aperture, following the same method as described above, and examines the nasal cavity in three sequential head positions:
- First Head Position: The patient's head and face are in a vertical position or slightly lowered. The nasal floor, inferior nasal concha, inferior nasal meatus, the anteroinferior portion of the nasal septum, and the lower portion of the common nasal meatus are observed.
- Second Head Position: The patient's head is tilted slightly backward at a 30° angle relative to the nasal floor. The middle portion of the nasal septum, middle nasal concha, middle nasal meatus, and part of the olfactory cleft are examined.
- Third Head Position: The head is tilted further backward at a 30° angle, allowing an examination of the upper nasal septum, the anterior end of the middle nasal concha, nasal ridge, olfactory cleft, and the anteroinferior portion of the middle nasal meatus.
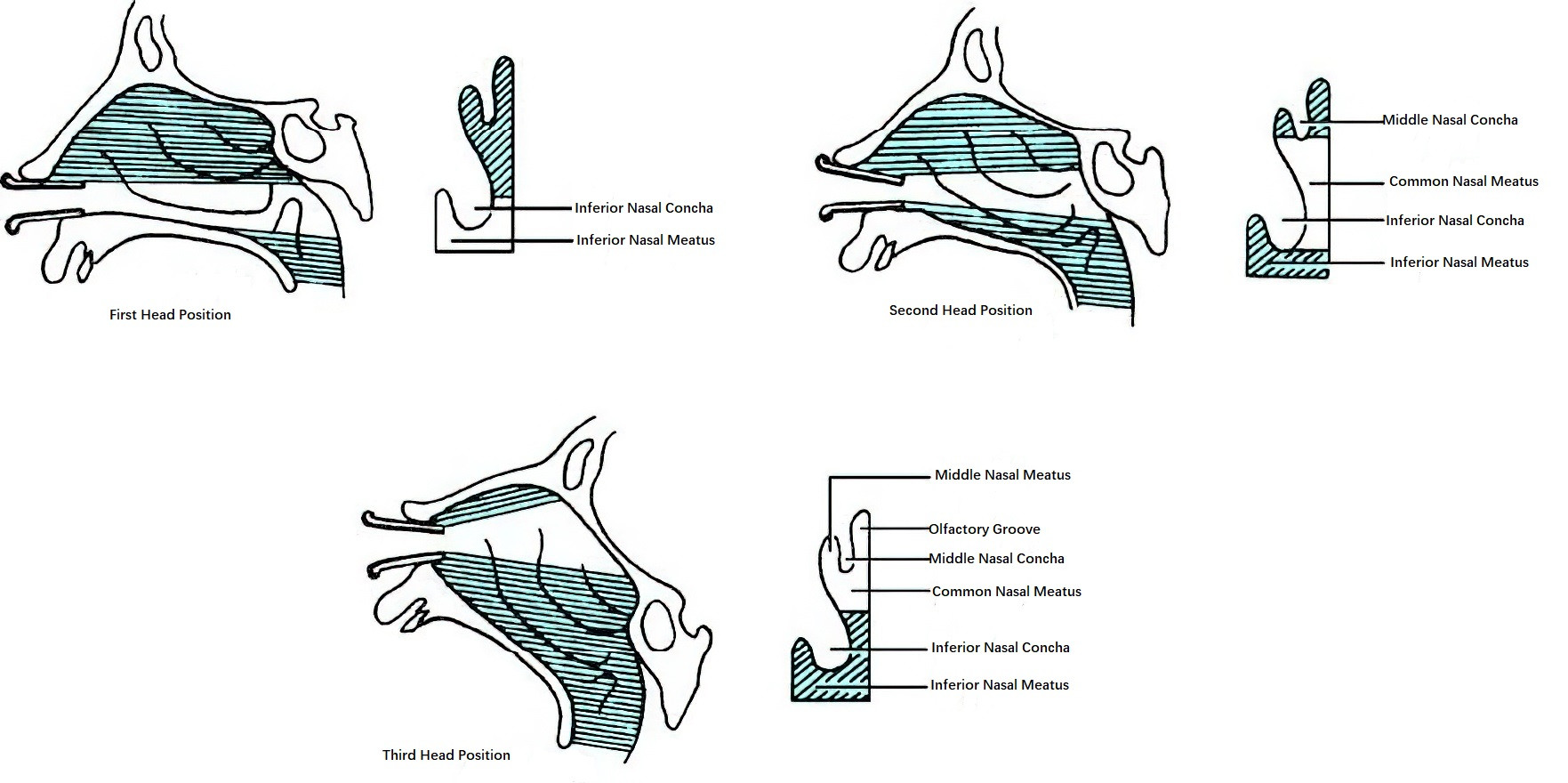
Figure 2 Three positions for anterior rhinoscopy
During the examination, attention is given to the following:
- The normal structure of the nasal conchae and the coloration of the nasal mucosa: A normal nasal concha appears smooth, with a distance maintained between the nasal conchae and the nasal septum. The mucosa covering the nasal conchae is light red, smooth, and moist. When touched with a swab (applicator), the mucosa feels soft and elastic, with a small amount of mucus exuding from the surface. There should be no mucus accumulation in the nasal meatus.
- Auxiliary tests: In cases of swollen or hypertrophic nasal conchae, 1% ephedrine nasal drops or other nasal decongestant sprays may be applied to constrict the nasal mucosa.
- Identification of positive findings: These include congestion, edema, hypertrophy, dryness, or atrophy of the nasal conchae; accumulation of secretions in the nasal meatus; polypoid changes of the middle nasal conchae; nasal septal abnormalities (such as deviation, bony ridges, spurs, or perforation); the presence of foreign bodies, polyps, or tumors.
Posterior Rhinoscopy
Posterior rhinoscopy is used to complement anterior rhinoscopy. An indirect nasopharyngeal mirror or fiberoptic nasopharyngoscope is inserted via the mouth or nasal cavity to examine the morphology, coloration, and secretions of the posterior nasal choanae, nasal conchae, and nasal meatus. This constitutes a fundamental examination technique.