Peripheral vestibular function plays a dominant role in maintaining balance. The vestibular nervous system has extensive connections with the cerebellum, spinal cord, eyes, and autonomic nervous system. Vestibular function examinations are not only relevant to otologic diseases but also pertain to areas such as neurology, neurosurgery, ophthalmology, internal medicine, and trauma medicine. They are primarily divided into two categories: the balance function of the vestibulospinal reflex system and the nystagmus response of the vestibulo-ocular reflex arc.
Balance Function Examination
Balance function examinations are classified into two major types: examinations of static balance and dynamic balance.
General Examinations
Romberg Test
This is the most commonly used method for static balance function assessment in outpatient settings. The subject stands upright with feet together and both hands clasped in front of the chest. The observer monitors whether the subject’s torso sways or leans when the eyes are open or closed. In cases of labyrinthine lesions, the subject tends to sway toward the side of the slow phase of nystagmus (the side with reduced vestibular function), while in cerebellar lesions, the sway usually occurs toward the lesion side or backward.
Past Pointing Test
The subject alternately uses both index fingers to touch the examiner’s index finger positioned in front and below, first with the eyes open and then with the eyes closed. In labyrinthine lesions, both arms deviate toward the side of the slow phase of nystagmus. In cerebellar lesions, only one arm shows deviation.
Walking Test
The subject is asked to walk forward five steps and then backward five steps with their eyes closed, repeating this five times. The gait is observed, and the angle of deviation between the starting and ending points is measured. An angle exceeding 90° indicates significant asymmetry in vestibular function between the two sides. Alternatively, the subject walks straight forward with eyes closed, and a deviation toward the weaker vestibular side may indicate a lesion. This test holds clinical significance in evaluating balance disorders and the degree of recovery in balance function. Central lesions, on the other hand, often result in a characteristic ataxic gait.
Fistula Test
The pneumatic otoscope is pressed tightly against the subject’s external auditory canal, alternately applying and releasing pressure. The eye movements and the presence of vertigo are observed. If eye deviation or nystagmus accompanied by vertigo occurs, the fistula test is considered positive. If only vertigo is present without eye deviation or nystagmus, the result is weakly positive, indicating a suspected fistula. A negative result indicates no abnormal findings.
A fistula located in the middle segment of the lateral semicircular canal (posterior to the ampulla) causes endolymph flow toward the vestibule when pressure is applied, exciting the hair cells within the ampulla and producing nystagmus with a fast phase toward the same side. Conversely, a fistula closer to the anterior vestibular area causes the endolymph to flow away from the vestibule, inhibiting lateral semicircular canal function and producing nystagmus with a fast phase toward the opposite side.
In cases of a dead labyrinth or obstruction of the fistula (e.g., by granulation tissue, cholesteatoma, or fibrosis), the fistula test may yield negative results but cannot entirely exclude the possibility of a labyrinthine fistula. In Meniere's disease, adhesions can form between the membranous labyrinth and the footplate of the stapes, resulting in a positive fistula test, also referred to as the Hennebert sign. Additionally, strong sound stimuli may induce dizziness or vertigo, a phenomenon known as the Tullio phenomenon, often associated with labyrinthine fistulas or cracks in the anterior semicircular canal.
Posturography
Posturography provides objective and precise results for balance function assessment.
Static Posturography
This method records the displacement of the body’s center of gravity caused by postural sway during standing with eyes open and closed. Pressure sensors within a pressure plate under the feet transmit information to a computer for analysis. It quantifies the Romberg test by analyzing the trajectory of the center of gravity. However, because this method does not exclude proprioceptive information, the ability to extract vestibular function information is limited, reducing its value in clinical application.
Dynamic Posturography
Movement Coordination Test (MCT)
This method assesses the amplitude and latency of electromyographic (EMG) responses in the limb's antigravity muscles during platform movements and tilts.
Sensory Organization Test (SOT)
In this test, a visual screen with adjustable tilt angles is placed in front of a balance platform. Six conditions are created by altering platform tilt angles, visual field tilt angles, and testing with eyes open or closed. It eliminates proprioceptive input at the ankle, knee, and hip joints and isolates visual input to provide vestibular-specific information about its influence on balance.
Gait Analysis
Gait analysis evaluates balance function during active walking. The subject wears two foot plates equipped with pressure switches, which transmit data for analysis. Electromyographic data of the antigravity muscles are incorporated to assess gait and balance during locomotion.
Nystagmus Examination
Nystagmus is an involuntary rhythmic movement of the eyes. It is often categorized into vestibular nystagmus, central nystagmus, and ocular nystagmus. Based on the direction of the eye movement, nystagmus can be classified as horizontal, vertical, rotational, dissociated, or diagonal. Combinations of directions, such as horizontal/rotational or vertical/rotational nystagmus, are frequently observed.
Vestibular nystagmus consists of alternating slow-phase (slow component) and fast-phase (quick component) movements. The slow phase involves a gradual movement of the eyes toward the side with lower vestibular excitability, typically corresponding to the side of the vestibular lesion or dysfunction. However, during the acute phase of vestibular irritation, a transient increase in excitability in the affected side may cause the slow phase to initially be directed toward the healthy side; this direction may reverse as vestibular function diminishes further. The fast phase is a corrective motion toward the side with higher vestibular excitability, regulated by the midbrain's quick-phase center. The direction of the fast phase is typically used to define the direction of nystagmus due to its ease of observation.
General Methods for Nystagmus Examination
Spontaneous Nystagmus Examination
During this test, the examiner holds a finger 40–60 cm in front of the subject to guide their gaze in five directions: left, right, upward, downward, and straight ahead. The examiner observes the eye movements for any nystagmus, noting its direction and intensity. The angle of deviation of the eyes from the midline should not exceed 30° to avoid inducing physiological end-point nystagmus. Nystagmus intensity is graded into three levels:
- Grade I: Nystagmus occurs only when gazing in the direction of the fast phase.
- Grade II: Nystagmus is observed both in the direction of the fast phase and during frontal gaze.
- Grade III: Nystagmus occurs during frontal gaze as well as in the directions of both the fast and slow phases.
By characterizing spontaneous nystagmus, it is possible to preliminarily differentiate whether the nystagmus originates from peripheral, central, or ocular causes.
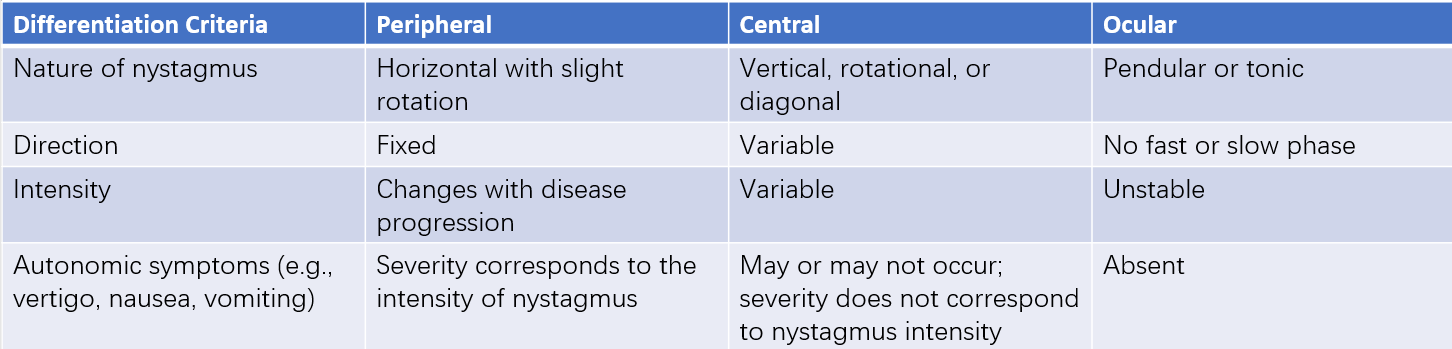
Table 1 Differentiation of spontaneous nystagmus
Frenzel Glasses Examination
Frenzel glasses are convex lenses with diopters of +15 to +20 D, typically equipped with small lightbulbs for illumination. When a subject wears these glasses during the examination, fixation-induced suppression of nystagmus—commonly observed during naked-eye testing—is minimized. The magnification effect of the convex lenses and the additional lighting make nystagmus easier to detect.
Positional Nystagmus Examination
Positional nystagmus refers to nystagmus that occurs only when the head is in a specific position. The examination is typically conducted in a dark room. The subject’s head is first turned to the left and right and tilted forward and backward by 45–60° while in a seated position. This is followed by similar head movements in the supine position and finally with the head hanging off the edge of the examination table (head-hanging position). Changes in head position should be performed slowly, with each position maintained for at least 30 seconds while observing and recording nystagmus.
Positioning Nystagmus Examination
Positioning nystagmus is provoked by rapid changes in head or body position and is often associated with benign paroxysmal positional vertigo (BPPV). The underlying cause is stimulation of the semicircular canal’s ampullary crest by otolith debris dislodged from the utricle. The subject begins in a seated position with their head upright. The examiner, standing to the subject’s right, holds the subject's head and conducts the following sequence: seated → supine head-hanging → seated → rightward head turn with supine head-hanging → seated → leftward head turn with supine head-hanging → seated. Each positional change is completed within 3 seconds, and observations are recorded for 20–30 seconds after each movement. Observations include latency, the nature and direction of nystagmus, amplitude, slow-phase velocity, duration, and the presence of symptoms such as vertigo, nausea, or vomiting. If nystagmus occurs, it is observed for 1 minute after its onset and evaluated further before proceeding to the next position.
Videonystagmography (VNG)
Videonystagmography (VNG) is one of the most commonly used methods for recording nystagmus. Infrared cameras mounted within a closed eye mask capture eye movements and transmit the data to a computer for analysis. Specialized software measures and processes various nystagmus components, such as the slow and fast phases. While VNG is a highly versatile tool, it requires a controlled environment with low light, minimal noise, and a stable temperature.
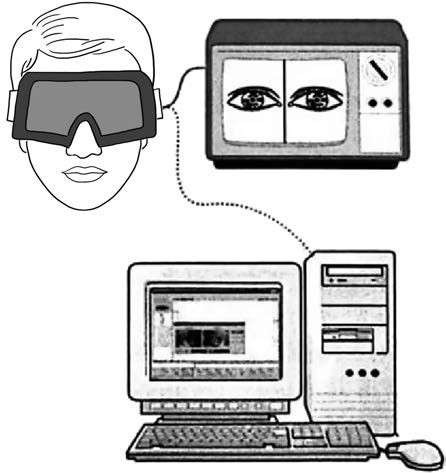
Figure 1 Method for capturing eye movement via nystagmography
VNG plays a crucial role in vestibular function testing and can be divided into two main categories: vestibulo-ocular testing and visual-ocular testing. Vestibulo-ocular testing includes assessments of spontaneous and induced nystagmus, while visual-ocular testing involves saccade testing, smooth pursuit tracking, and optokinetic nystagmus tests. These tests evaluate the functions of the visual system and visuovestibular system, providing invaluable insights into peripheral and central vestibular system function.
VNG is particularly useful for diagnosing and assessing balance disorders. It can detect subtle nystagmus with intensities as low as 7°/s, which are invisible to the naked eye, and allows for precise measurement of nystagmus intensity, direction, and other parameters. However, VNG is a functional test and cannot directly correlate specific findings to a particular disease. Its results must be interpreted in conjunction with physical examinations, patient history, audiological tests, imaging studies, and other vestibular function tests for comprehensive evaluation and diagnosis.
Identification of Nystagmus Direction Using VNG
Determining Horizontal or Vertical Orientation
In the horizontal direction, rightward movements correspond to an upward deflection; leftward movements correspond to a downward deflection.
In the vertical direction, upward movements are classified as upward nystagmus; downward movements are classified as downward nystagmus.
Analyzing the Direction of the Fast Phase
Horizontal
An upward fast phase indicates rightward nystagmus; a downward fast phase indicates leftward nystagmus.
Vertical
An upward fast phase indicates upward nystagmus; a downward fast phase indicates downward nystagmus.
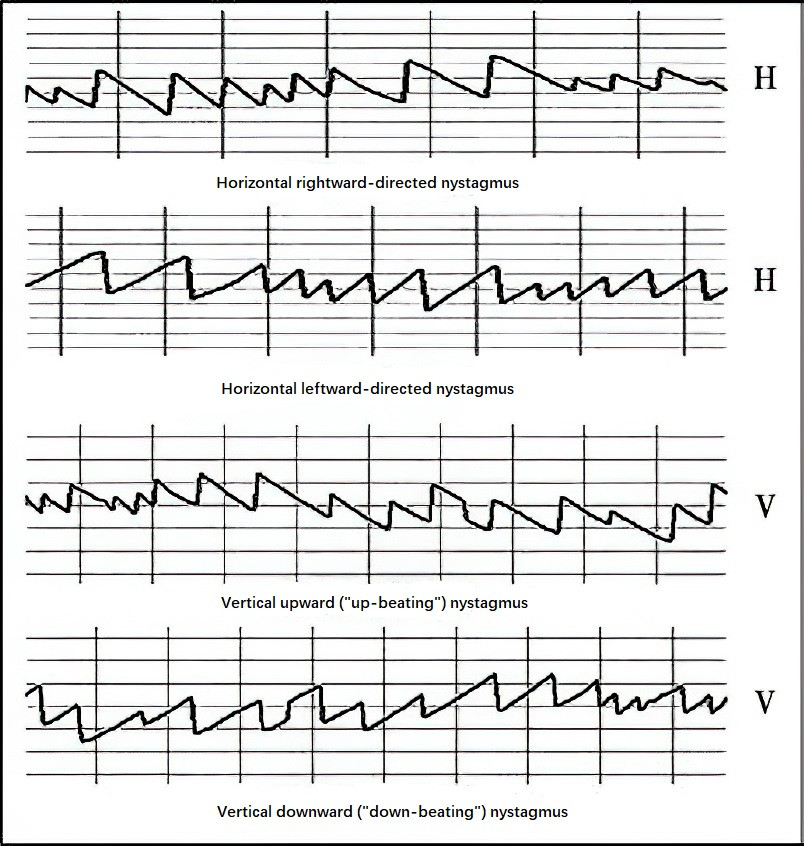
Figure 2 Nystagmus patterns in different directions
H: Horizontal
V: Vertica
Examination of Otolith Organs and Their Neural Pathways
Vestibular evoked myogenic potential (VEMP) is a short-latency response recorded from the surface of tensed muscles, triggered by strong sound stimulation of the vestibular otolith organs through a reflex pathway. VEMP includes cervical vestibular evoked myogenic potential (cVEMP) and ocular vestibular evoked myogenic potential (oVEMP).
cVEMP is a myogenic potential (p13/n23) induced by loud stimuli and recorded from surface electrodes placed on the actively contracted sternocleidomastoid muscle (SCM). This potential has been confirmed to originate from the saccule and is highly reproducible. It serves as a clinical indicator for assessing the function of the saccule and the inferior vestibular nerve.
oVEMP is recorded from surface electrodes placed on the inferior oblique and inferior rectus muscles beneath the eye, which contract in response to strong auditory stimuli, producing a myogenic potential (n10/p15). The exact origin of these signals remains debated, with some suggesting the utricle or both the saccule and utricle; however, current understanding leans toward the utricle as the primary source. oVEMP is considered a clinical indicator for evaluating the function of the utricle and the superior vestibular nerve.
In clinical practice, cVEMP and oVEMP are often tested together. They assist in diagnosing and evaluating peripheral vestibular dysfunction caused by conditions such as vestibular neuritis, endolymphatic hydrops, superior semicircular canal dehiscence syndrome, Meniere’s disease, vestibular schwannoma, and cochlear implantation.