Electric response audiometry (ERA) refers to an objective hearing assessment method that detects various bioelectric potentials, known as auditory evoked potentials (AEPs), generated during the transmission of sound waves through cochlear hair cells, the auditory nerve, and the auditory pathways to the auditory cortex.
The cochlear potentials, auditory brainstem responses, middle-latency responses, and cortical potentials used in clinical audiometry typically have amplitudes in the microvolt (μV) range. These signals are often masked by other spontaneous bioelectric potentials generated by the body, such as electroencephalographic (EEG) signals (in the millivolt [mV] range), background noise, and alternating electrical fields. By repeatedly presenting sound stimuli and employing electronic computer signal averaging techniques, the polarity-consistent microvolt potentials are enhanced, while polarity-random potentials like EEG signals are canceled out due to the summation of positive and negative phases.
Electrocochleography
Electrocochleography refers to the method of recording bioelectric potentials generated by the cochlea and auditory nerve in response to sound stimuli. The recorded waveform, known as the electrocochleogram (ECochG), consists of three components:
- Cochlear Microphonic Potential (CM): This alternating current potential, originating from the outer hair cells of the cochlea, has virtually no latency. Its waveform mirrors the waveform of the sound stimulus and lasts for the same or slightly longer duration as the stimulus. The amplitude of CM increases with increasing sound intensity.
- Summating Potential (SP): This negative direct current potential originates from the cochlear hair cells. Like the CM, it lacks latency and refractory periods.
- Compound Action Potential (AP): This potential, originating from the auditory nerve, primarily consists of a series of negative peaks (N1–N3). Its latency is inversely proportional to stimulus intensity, while its amplitude is directly proportional to stimulus intensity.
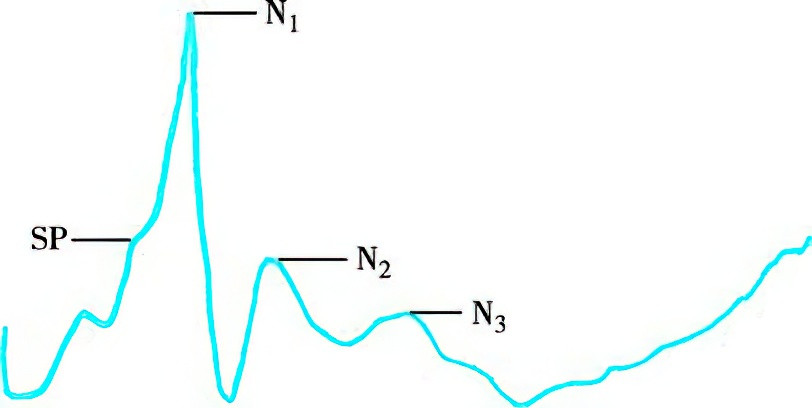
Figure 1 Electrocochleogram (ECochG)
In clinical applications, short-duration sounds (clicks), which elicit optimal neural synchronization, are used as stimulus signals, typically presented at a rate of 10 stimuli per second. Near-field recordings involve placing a lead electrode through the tympanic membrane onto the promontory, while far-field recordings use a miniature silver ball electrode placed at the posterior-inferior edge of the tympanic membrane near the annulus.
The primary clinical metric in electrocochleography is the AP waveform. Alternating-phase sound stimuli are used to cancel out CM, leaving a combined waveform of SP and AP. In cases of endolymphatic hydrops, the SP/AP amplitude ratio increases. Parameters such as AP latency, amplitude, duration, intensity-amplitude function curves, and intensity-latency function curves are useful for distinguishing types of hearing loss and assessing treatment efficacy. Electrocochleography is considered an ideal method for evaluating peripheral auditory and auditory nerve function due to its objectivity, unilateral focus, repeatability, and accuracy.
Auditory Brainstem Response (ABR)
Auditory brainstem response (ABR) involves recording evoked bioelectric responses with latencies within 10 milliseconds after auditory stimulation. This method is used to assess the auditory system and brainstem function in an objective manner. Short sound bursts (clicks) are presented at a rate of 20–30 stimuli per second. Electrodes are placed on the forehead (active electrode) and the earlobe of the stimulated side (reference electrode) for far-field recordings. The recorded responses are amplified and averaged 1,000 times.
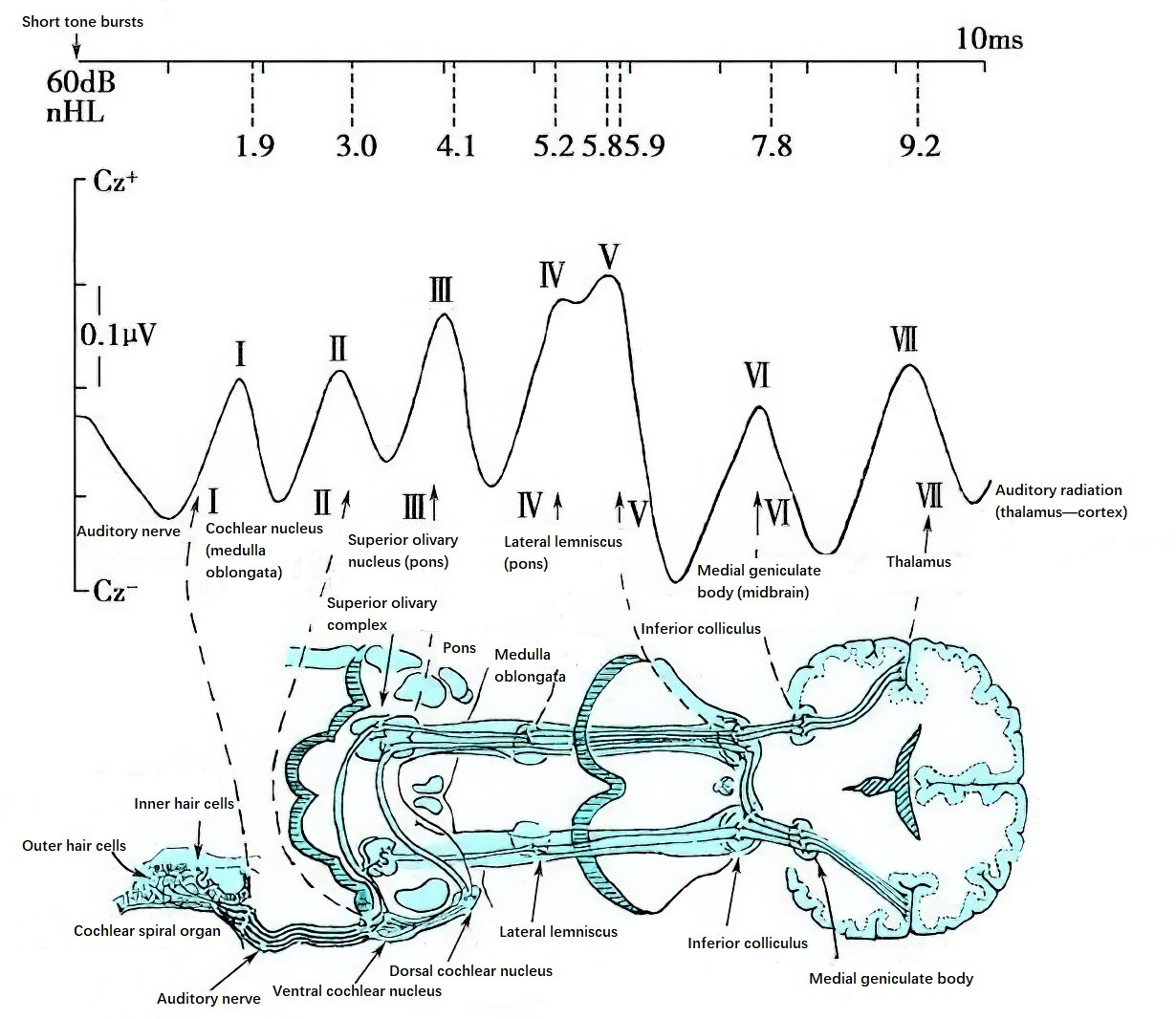
Figure 2 Schematic diagram of the seven typical waves of auditory brainstem response and their origins
The auditory brainstem response consists of seven positive peaks (Waves I–VII) occurring within a 1–10 millisecond timeframe.
Clinically, ABR analysis focuses on the latency of Waves I, III, and V; interpeak intervals (I–III, III–V, and I–V); and interaural differences in Wave V latency and I–V interpeak intervals. These parameters are used to evaluate auditory and brainstem function. The Wave V threshold is used to approximate mid- to high-frequency hearing thresholds. However, the ABR Wave V threshold does not precisely represent or replace behavioral hearing thresholds and is typically 15–20 dB higher than behavioral thresholds.
ABR is widely used for newborn and infant hearing screening, differentiation between organic and functional hearing loss, diagnosis of cerebellopontine angle tumors, assessment of brainstem function, intraoperative monitoring of brainstem function, and determination of brain death. It provides valuable objective information for these purposes.
Derived forms of ABR include click-evoked ABR (click-ABR), cortical auditory evoked potentials (CAEP), frequency-specific auditory evoked potentials (fs-AEP) under free-field conditions, and electrically evoked auditory brainstem responses (EABR).
40Hz Auditory Event-Related Potential (AERP)
The 40Hz AERP is an evoked potential test involving short-duration sounds or tone bursts presented at a rate of 40 stimuli per second. This method elicits sinusoidal-like bioelectric responses at approximately 40 Hz, with one peak occurring every 25 milliseconds. AERP is a derivative of middle-latency response testing.
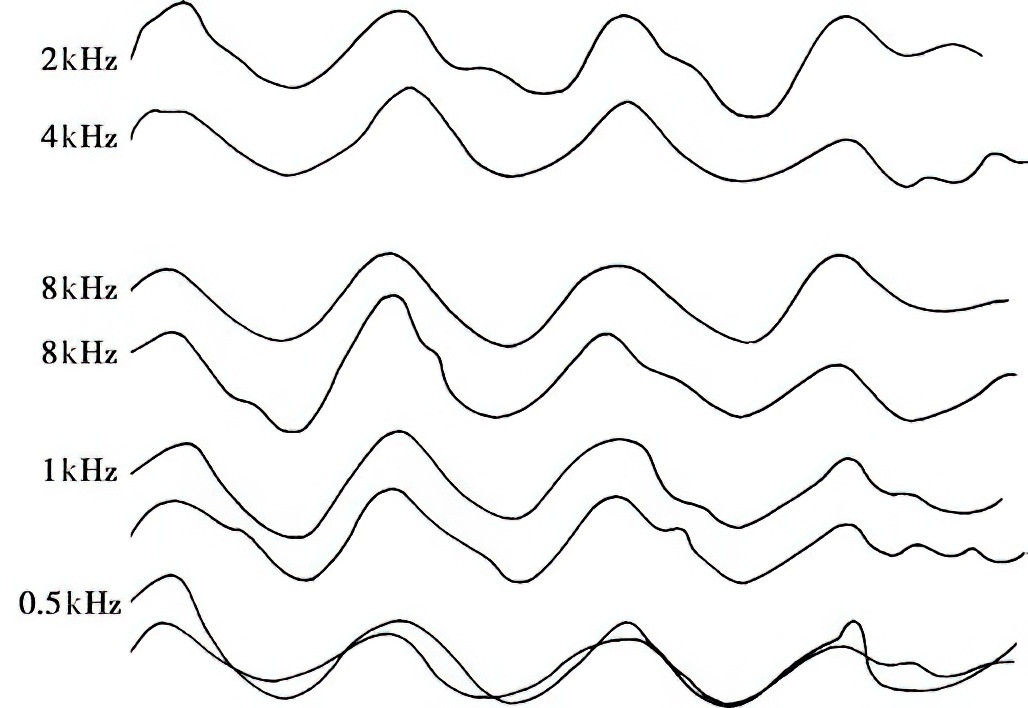
Figure 3 40Hz auditory event-related potential (AERP) curve
AERPs are primarily used for objective hearing threshold estimation. When tone bursts are used as stimuli, AERP demonstrates frequency specificity, making it especially valuable for determining thresholds below 1,000 Hz. Average response thresholds for stimuli at 500 Hz, 1,000 Hz, and 2,000 Hz are approximately 10 dB nHL. AERP, combined with ABR testing (which assesses mid- to high-frequency thresholds), provides an ideal method for objective hearing threshold evaluation.
Auditory Steady-State Response (ASSR)
ASSR refers to steady-state bioelectric responses elicited by amplitude-modulated tones across multiple frequencies. This method allows frequency-specific testing of auditory responses within the range of 250–8,000 Hz.
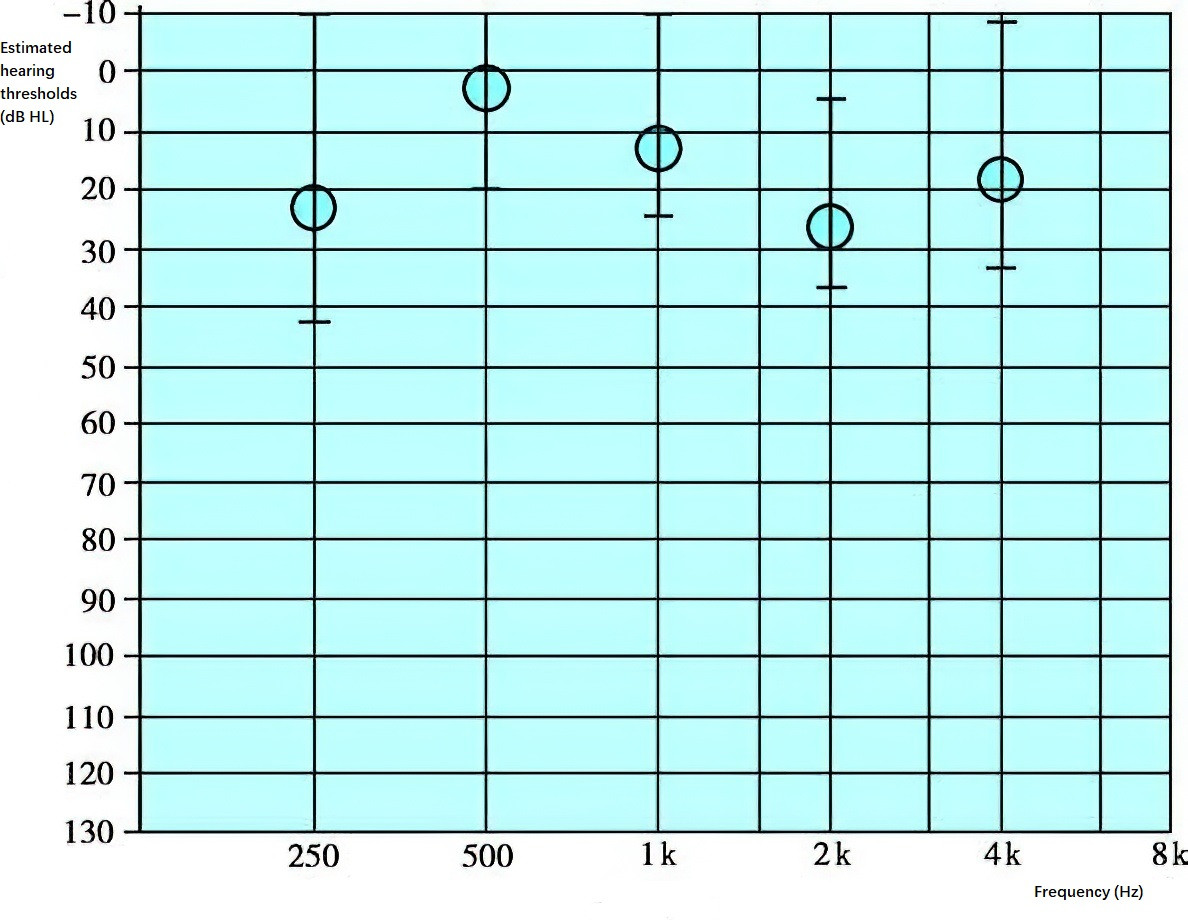
Figure 4 Multifrequent steady-state evoked response
The advantages of ASSR over ABR include its ability to measure hearing thresholds at different frequencies, its capability to deliver stimulus intensities up to 120 dB nHL, and its high accuracy in detecting moderate-to-severe hearing loss.
The main limitation of ASSR is its reduced accuracy when estimating thresholds in individuals with normal hearing or mild hearing loss.
In clinical practice, ASSR is often used to assess hearing thresholds in children with severe hearing loss and as a key reference for hearing aid fitting. Given its inherent limitations, ASSR results are typically interpreted in conjunction with ABR, behavioral audiometry, and 40-Hz AERP findings.