Examination of the Auricle and Surrounding Area
The examination of the auricle relies primarily on visual inspection and palpation.
Examination of Auricular Deformities
Auricular deformities are often congenital.
Accessory Auricle
This is also known as accessory ear, where the auricle is normal but small skin tags, often containing cartilage, are present around the tragus.
Protruding Ear
This is caused by the forward and downward inclination of the helix and scaphoid fossa, leading to an overall forward projection of the auricle.
Macacus Ear
The upper posterior part of the helix protrudes in a triangular shape.
Microtia
This is characterized by underdeveloped auricles. It is classified into three grades:
- Grade I: Auricle is smaller, and partial closure of the external auditory canal is observed.
- Grade II: Accompanied by middle ear deformities, which are more common.
- Grade III: Accompanied by inner ear deformities.
Congenital Preauricular Fistula
This is characterized by a fistula in front of the auricular crus, which may discharge white sebaceous material upon compression. During inflammation, redness and swelling around the fistula, along with a fluctuating sensation during abscess formation, may occur. Severe cases lead to abscess rupture.
Branchial Fistula
Fistula openings may be present in the external auditory canal or auricle, and in the neck region at the second fistula. Cyst-like structures may exist between the two openings. During inflammation, redness, swelling, or inflammatory exudates may appear in the auricle, external auditory canal, or neck region.
Examination of Auricular Cysts
Localized swelling in the concha or cymba conchae is typically positive for transillumination when illuminated from behind the auricle.
Examination of Auricular Inflammation
Symptoms of redness, swelling, severe pain, and clustered blisters (herpes zoster) around the auricle, accompanied by ipsilateral peripheral facial paralysis, hearing loss, or vertigo, are indicative of Hunt syndrome. Diffuse auricular redness and dark discoloration may occur following frostbite or trauma, leading to perichondritis and subsequent auricular deformities due to contracture.
Examination of Postauricular Inflammation
Subperiosteal abscesses behind the ear, disappearance of the postauricular sulcus groove, swelling with a fluctuating sensation, and forward and outward displacement of the auricle may indicate an extracranial complication of suppurative otitis media with mastoiditis. Tenderness in postauricular lymph nodes should prompt an examination for scalp infections such as folliculitis.
Examination of the Preauricular and Infraauricular Regions
Pain during mouth opening accompanied by tenderness in the area anterior to the tragus often suggests temporomandibular joint inflammation or dysfunction. Swelling centered around the earlobe and extending below or around the auricle, located on the surface of the sternocleidomastoid muscle, may originate from the parotid gland. Smooth, mobile, medium-textured masses are often pleomorphic adenomas of the parotid gland, while fixed, ill-defined masses suggest malignant parotid tumors. Masses situated between the mastoid process and the mandible below the ear, especially when located deep to the sternocleidomastoid muscle, are often malignant metastatic lymph nodes of the upper deep cervical group, commonly originating from nasopharyngeal carcinoma.
Examination of the External Auditory Canal and Tympanic Membrane
The examiner and the patient should sit facing each other. The light source for the examination is positioned to the upper left of the patient’s head. The examined ear is turned towards the examiner, and the light beam reflected from the head mirror is directed onto the opening of the external auditory canal.
Manoeuvre Method
Due to the curved structure of the external auditory canal, the auricle is gently pulled backward, upward, and outward (or downward in infants) with one hand (or both hands) to straighten the canal. Simultaneously, the tragus is pressed forward with the index finger to enlarge the canal opening, providing a clearer view of the external auditory canal and tympanic membrane.

Figure 1 Manual ear examination using both hands
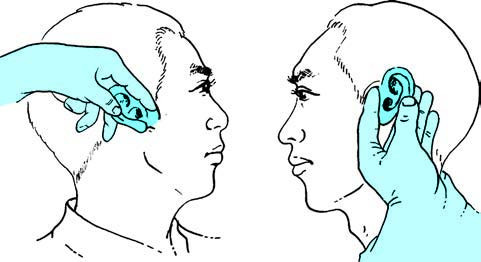
Figure 2 Manual ear examination using one hand
If there is pain upon pulling the auricle, the external auditory canal should be examined for the following:
- Localized redness and swelling in the cartilaginous portion of the canal may indicate a furuncle.
- Cerumen in the canal is yellowish-white and generally forms flakes. Oily cerumen appears brownish or soy-colored and liquid in form. Accumulated cerumen often forms hard brown plugs requiring softening with 3% sodium bicarbonate solution before removal.
- Diffuse redness and swelling of the canal skin may indicate external auditory canal inflammation.
- Black debris or white speckled deposits in the canal suggest external auditory canal fungal infection.
- Early-stage suppurative otitis media often produces clear, watery discharge, whereas chronic suppurative otitis media typically results in thick, foul-smelling discharge.
- Since the skin of the external auditory canal lacks mucous glands, the presence of mucus or mucopurulent secretions indicates a middle ear pathology.
Otoscopy
Conventional Otoscopy
For narrow or inflamed ear canals, a funnel-shaped otoscope is used, inserted into the external auditory canal while avoiding the hair in the cartilaginous portion to allow proper illumination. The axis of the otoscope should align with the long axis of the external auditory canal to enable visualization of the tympanic membrane. The bony portion of the canal lacks subcutaneous fat, so the tip of the otoscope should not extend beyond the cartilaginous portion to prevent pain. Otoscopy can be performed using either a one-handed or two-handed technique.
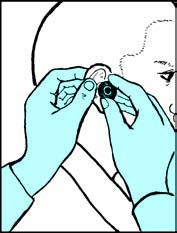
Figure 3 Otoscopic examination using both hands
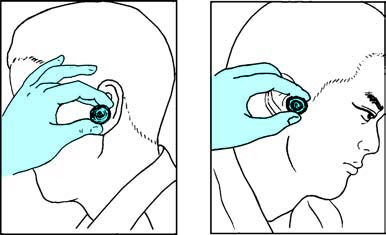
Figure 4 Otoscopic examination using one hand
Viewing the tympanic membrane requires adjustment of the otoscope's direction. The cone of light, located anteroinferiorly to the umbo, is identified first, followed by the observation of the malleus handle, the short process, and the anterior and posterior mallear folds. The distinction between the pars tensa and pars flaccida is then noted. A normal tympanic membrane appears semi-transparent and milky white.
Changes in Tympanic Membrane Color
Acute otitis media or acute inflammation of the tympanic membrane presents with redness and swelling of the tympanic membrane.
When there is fluid in the tympanic cavity, the tympanic membrane initially appears pink and later transitions to an amber (orange-yellow) color as the fluid thickens. Partial fluid in the tympanum may reveal an arc-shaped fluid level or air bubbles through the membrane.
Tympanosclerosis thickens the tympanic membrane, leading to the appearance of white calcified plaques.
Cholesterol granuloma, high jugular bulb, or glomus jugulare tumors result in a blue tympanic membrane.
Granulation tissue on the tympanic membrane can be visualized using a pneumatic otoscope. Granulation originating from tympanic membrane inflammation moves with the membrane, while granulation originating from the middle ear does not.
Bullous myringitis appears as dark red blisters on the surface of the tympanic membrane.
Tympanic Membrane Perforation
Perforations are classified based on location into those affecting the pars tensa, pars flaccida, or marginal perforations. Through the perforation, features such as mucosal congestion, edema, granulation tissue, calcified plaques, polyps, or cholesteatoma may be observed in the tympanic cavity.
In acute suppurative otitis media, the tympanic membrane appears red and swollen, with perforations resembling pinholes and potentially pulsating discharge.
In chronic suppurative otitis media, perforations in the pars tensa are kidney-shaped and surround the malleus handle, which may sometimes be exposed. Severe cases may lose the residual rim, and the malleus handle may also erode.
Tympanic membrane perforation due to middle ear cholesteatoma is primarily found in the pars flaccida. An early indication of acquired primary cholesteatoma is a yellowish-white bulging appearance in the pars flaccida, followed by gradual perforation. Cholesteatomas appear as white, lamellar masses of desquamated squamous epithelium, resembling moist cheese when wet.
Pneumatic Otoscopy (Siegle Otoscopy)
The pneumatic otoscope integrates a magnifying lens at the rear of a funnel-shaped otoscope and connects to a rubber bulb via a fine rubber tube. During examination, the otoscope is sealed against the skin of the external auditory canal, and alternating positive and negative pressure is applied by compressing the rubber bulb, causing inward and outward movement of the tympanic membrane. Decreased or absent tympanic membrane mobility indicates fluid accumulation in the tympanic cavity, while abnormally increased mobility may suggest Eustachian tube dysfunction or a thin tympanic membrane. Pneumatic otoscopy is capable of identifying tiny perforations, and negative pressure via the otoscope suction may draw discharge from small perforations. When performing a fistula test using a pneumatic otoscope, reference is made to vestibular function examination.
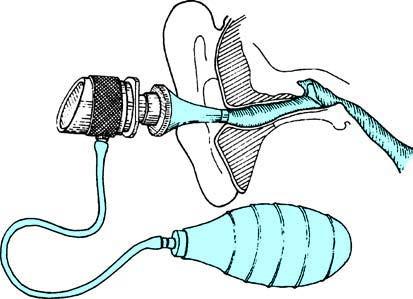
Figure 5 Pneumatic otoscopy
Electronic Otoscopy
This otoscope, equipped with a built-in light source and magnifying lens, provides detailed observation of subtle tympanic membrane changes, such as dilated microvascular patterns. It is particularly suitable for outpatient visits, bedridden patients, and infants.
Otoendoscopy
Otoendoscopy includes the use of otoendoscopes and microendoscopes, which can display the morphology of the external auditory canal and tympanic membrane on a monitor. To observe tympanic cavity lesions, a small incision may be made on the anesthetized tympanic membrane surface to insert the endoscope into the cavity. Perforations of the tympanic membrane allow direct examination of the Eustachian tube openings, ossicular chain, and tympanic isthmus. For inner ear pathology, a microendoscope with a diameter of 0.3–0.4mm may be inserted through a cochleostomy under a surgical microscope for direct observation.