The ear is divided into three parts: the external ear, middle ear, and inner ear. The primary structures of the ear are located within the temporal bone, which contains the bony part of the external auditory canal, the middle ear, the inner ear, and the internal auditory canal.
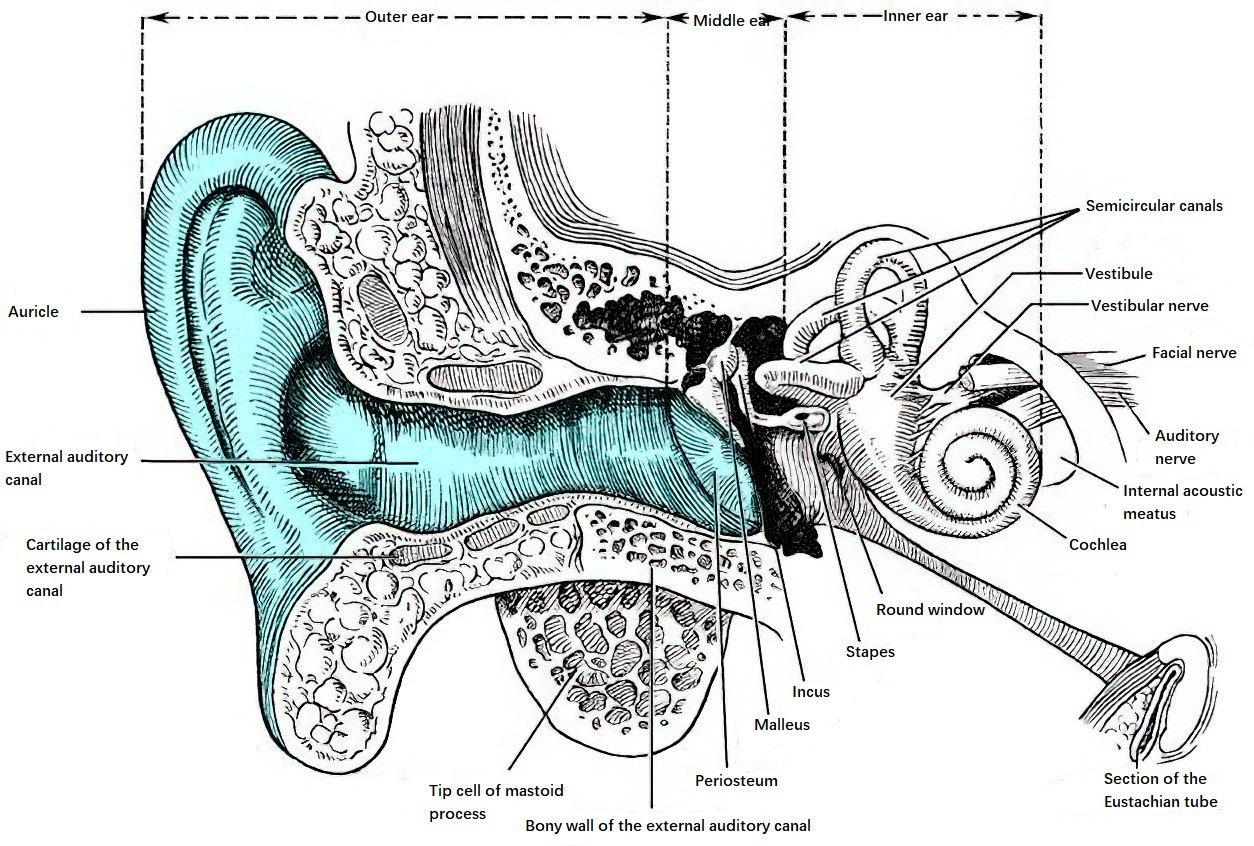
Figure 1 Schematic diagram of the anatomical relationships of the ear
Temporal Bone
The temporal bone is one of the most complex bony structures in human anatomy. It is located on both sides of the skull, wedged between the parietal, sphenoid, zygomatic, and occipital bones, contributing to the base and lateral walls of the skull. The temporal bone is a composite bone and is divided into five parts centered around the external auditory canal: the squamous portion, tympanic portion, mastoid portion, petrous portion, and styloid process.
Squamous Portion
Also known as the squama temporalis, this part occupies the upper anterior portion of the temporal bone and resembles the shape of a fish scale. It has an external surface and an internal surface. The outer surface is smooth and slightly convex, with a longitudinal groove for the middle temporal artery near its center. Below the groove, the zygomatic process projects forward and forms the zygomatic arch by joining the temporal process of the zygomatic bone. The zygomatic process has three roots: the anterior root (articular tubercle), the middle root (postglenoid process), and the posterior root. The posterior root extends backward along the upper margin of the zygomatic process, forming the curved temporal line, which is often used as an external landmark for the floor of the middle cranial fossa.
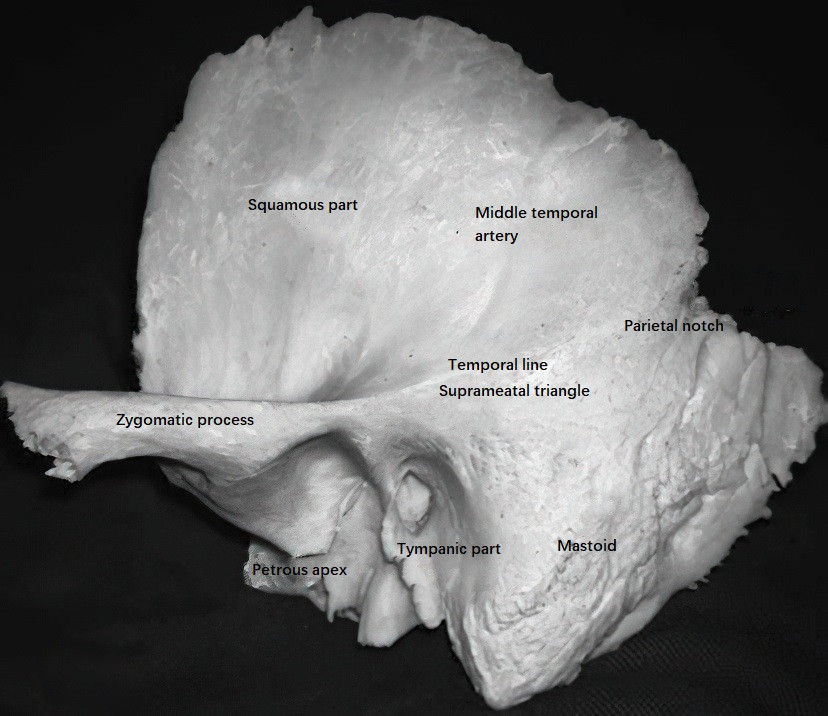
Figure 2 Lateral view of the temporal bone (Left side)
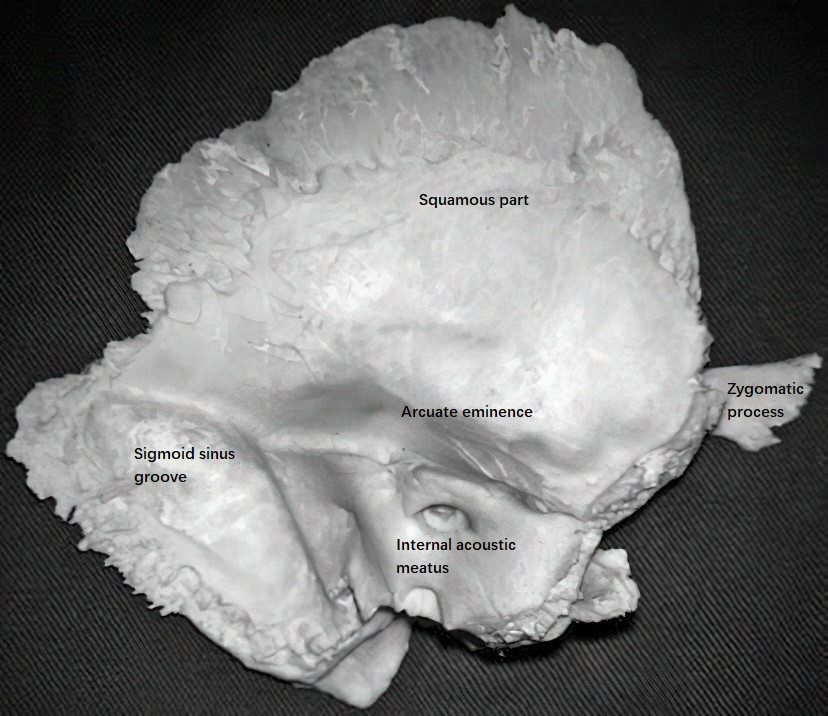
Figure 3 Medial view of the temporal bone (Left side)
Above the posterior superior margin of the external auditory canal, there is a small spine called the suprameatal spine. Behind this spine, a triangular area termed the suprameatal triangle (or cribriform area) is located; its rough and slightly depressed surface intersects the posterior superior wall of the external auditory canal with the temporal line. The mastoid air cells lie deep to this region.
The internal surface of the squamous portion is slightly concave and has impressions for cerebral gyri and grooves for the middle meningeal artery, corresponding to its contact with the temporal lobe. The posterior superior margin articulates with the parietal bone, while the anteroinferior margin articulates with the greater wing of the sphenoid bone. The inferior margin fuses with the anterior edge of the petrous portion, forming the petro-squamous suture. In adults, this suture is only visible as a trace, but it is more pronounced in children, allowing small blood vessels to traverse the dura mater into the middle ear. This anatomical feature can explain meningitic symptoms resulting from otitis media in children.
Tympanic Portion
The tympanic portion is a curved, U-shaped bony plate located below the squamous part, anterior to the mastoid portion, and on the outer lower side of the petrous portion. It forms part of the anterior, inferior, and posterior walls of the bony external auditory canal. The anteroinferior aspect of the tympanic portion contributes to the posterior wall of the mandibular fossa, while its inner end contains a groove called the tympanic sulcus. The fibrous ring of the tympanic membrane attaches to this sulcus. The superior aspect of the sulcus features a notch, the notch of Rivinus, which lacks both the sulcus and the fibrous ring.
Mastoid Portion
This portion forms the posteroinferior part of the temporal bone and appears as a conical projection. The lateral surface of the mastoid portion is rough, providing attachment sites for the sternocleidomastoid, splenius capitis, and longissimus capitis muscles. Near the occipitomastoid suture, also known as the occipitomastoid fissure, there is a mastoid foramen, which acts as a passage for the mastoid emissary vein, connecting extracranial veins to the sigmoid sinus.
The medial aspect of the mastoid tip contains a deep groove, the mastoid notch, which serves as the origin of the posterior belly of the digastric muscle. Medial to the notch lies the occipital artery groove, which accommodates the occipital artery. A sigmoid sulcus curves downward along the medial side of the mastoid portion, housing the sigmoid sinus. The depth and thickness of the bone in the sigmoid sulcus vary depending on the development of the mastoid air cells. In well-pneumatized mastoid portions, the sigmoid sinus plate is thinner and positioned further posteriorly, while in poorly developed ones, the plate is thicker and located anteriorly. During mastoid surgery, this anatomical variation can pose a risk of injuring the sigmoid sinus, potentially leading to bleeding or air embolism.
Petrous Portion
The petrous portion, located at the base of the skull, is wedged between the sphenoid and occipital bones. Its three-sided pyramidal shape gives it the nickname "petrous pyramid," and it houses the organs of hearing and balance.
The base of the petrous portion is directed outward and fuses with the squamous and mastoid portions, while its apex is rough and irregular. The apex points anteromedially and slightly upward, fitting into the angle formed by the posterior edge of the greater wing of the sphenoid bone and the occipital bone, forming part of the posterior and lateral margins of the foramen lacerum, where the carotid canal opens internally.
The petrous portion has three surfaces:
Anterior Surface
It forms the posterior part of the middle cranial fossa and connects to the cerebral surface of the squamous portion. Important landmarks from medial to lateral include:
- The trigeminal impression near the petrous apex, which accommodates the trigeminal ganglion (also called the semilunar ganglion).
- Two small grooves parallel to the long axis of the petrous pyramid, with the medial groove containing the greater petrosal nerve and leading to the hiatus for the facial canal.
- The lateral groove contains the lesser petrosal nerve and extends to the small aperture near the facial canal's opening. Both grooves serve as channels for their respective nerves.
- Laterally, an arcuate eminence is present, beneath which lies the anterior semicircular canal. The highest point of the anterior semicircular canal is located slightly anteromedial and inferior to the peak of the arcuate eminence.
- A thin bony plate, termed the tegmen tympani, separates the tympanic cavity from the middle cranial fossa.
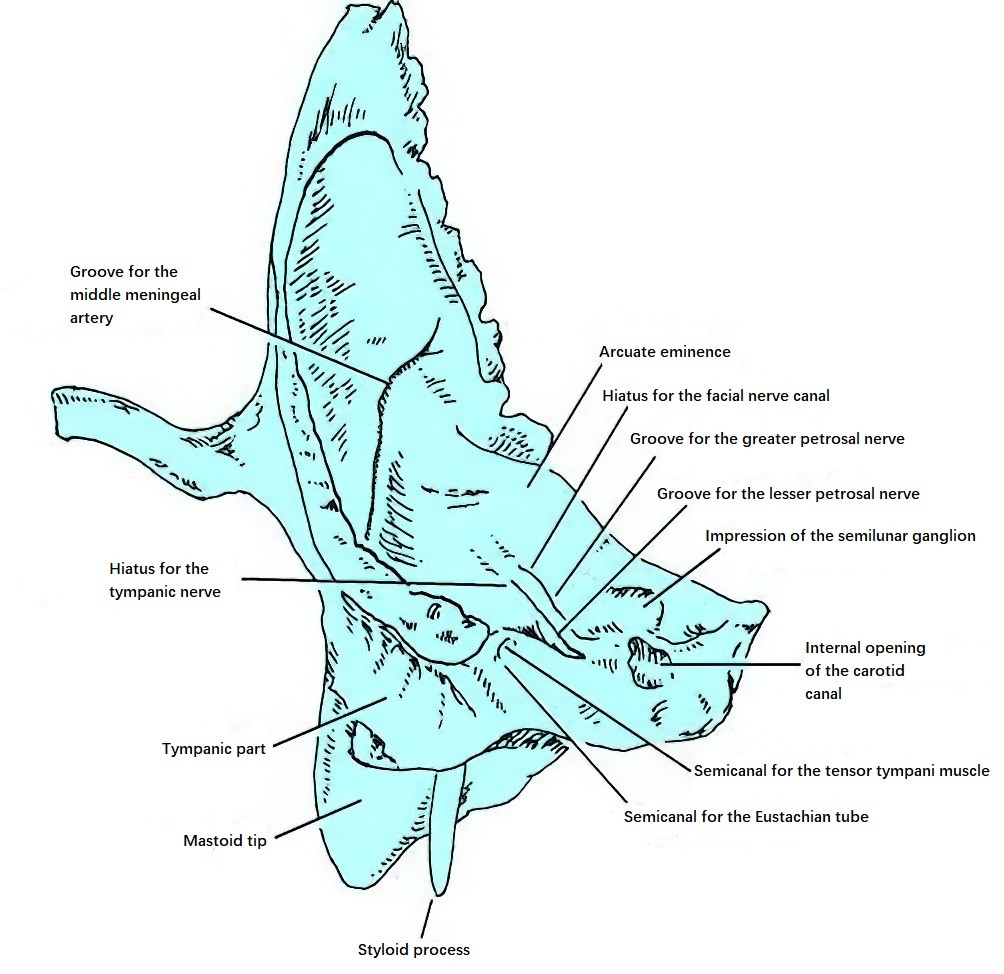
Figure 4 Anterior view of the petrous part
Posterior Surface
The posterior surface is a triangular bony area surrounded by the superior petrosal sinus, inferior petrosal sinus, and sigmoid sinus. Its apex points medially, and its base faces laterally, forming the anterior wall of the posterior cranial fossa and connecting to the medial surface of the mastoid portion. Near the central-medial area of the posterior surface lies the internal acoustic porus, which leads outward into the internal acoustic meatus. Posterolateral to this porus is a fissure covered by a thin bony plate that forms the external opening of the vestibular aqueduct (also known as the vestibular canaliculus), allowing the endolymphatic duct and endolymphatic sac to continue. Above this fissure and between it and the internal acoustic porus is a small depression called the subarcuate fossa.
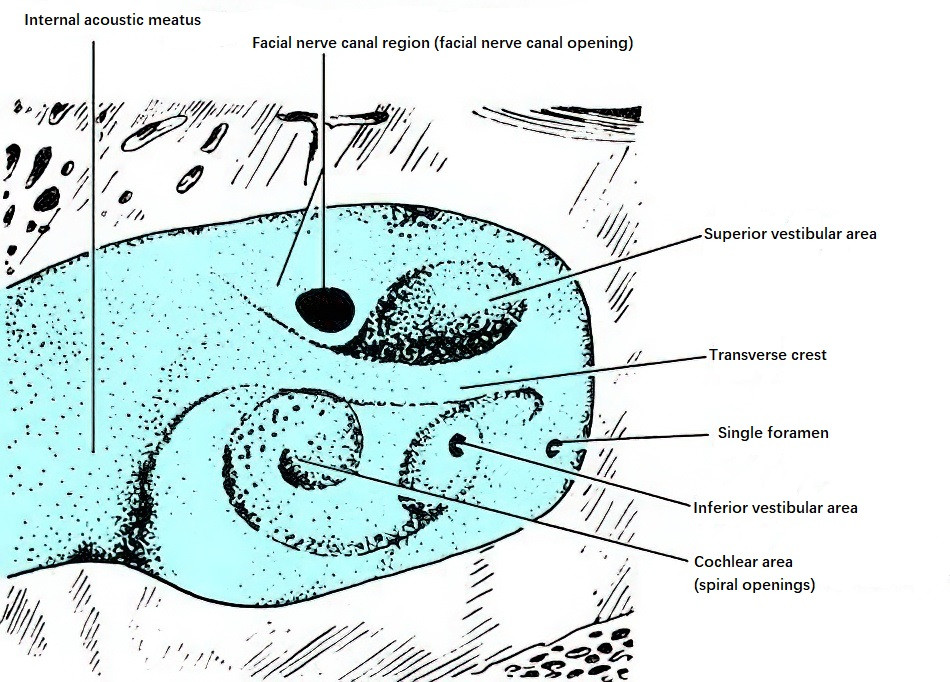
Figure 5 Base of the internal acoustic meatus (Right side)
The internal acoustic meatus (also known as the internal auditory canal) is a bony canal located within the petrous portion of the temporal bone. It has an average length of about 10 mm and a vertical diameter of approximately 5.9 mm. It serves as a passage for the facial nerve, cochlear nerve, vestibular nerve, intermediate nerve, labyrinthine artery, and labyrinthine vein. The internal acoustic meatus extends posteriorly and laterally into the petrous portion of the temporal bone, almost at a right angle to the petrous axis. The dura mater extends into the meatus via the internal acoustic porus, covering its surface. The external end of the internal acoustic meatus is sealed by a vertically oriented bony plate perforated by numerous small holes, forming what is called the fundus of the internal acoustic meatus.
The fundus constitutes most of the medial walls of the vestibule and cochlea. A transverse crest divides the fundus into upper and lower regions.
The upper region is smaller and further subdivided by a vertical crest into anterior and posterior sections. The anterior section is the facial canal region, where the facial nerve enters the facial canal and continues outward via the labyrinthine segment. The posterior section is the superior vestibular region, which contains small foramina for the passage of terminal branches of the superior vestibular nerve, supplying the utricular macula, anterior semicircular canal, and lateral semicircular canal ampulla.
The lower region is further divided at the anterior part into the cochlear region, containing numerous spirally arranged foramina for cochlear nerve fibers, and at the posterior part into the inferior vestibular region, where several small foramina allow passage of branches of the inferior vestibular nerve to the saccule. In the posteroinferior corner of the inferior vestibular region, an individual foramen exists for the posterior ampullary nerve branch of the vestibular nerve.
Inferior Surface
The inferior surface is rough and irregular, forming part of the external base of the skull. The petrous portion contains two adjacent deep fossae in its medial aspect. The carotid canal external opening is located anteromedially, allowing passage of the internal carotid artery and the carotid plexus of nerves. Posterolaterally lies the jugular fossa, which houses the jugular bulb. An anteromedial triangular indentation near the jugular fossa contains the external opening of the cochlear aqueduct, through which perilymph drains into the subarachnoid space. This aqueduct is a consistent anatomical feature and serves as an important landmark, located adjacent to the glossopharyngeal nerve.
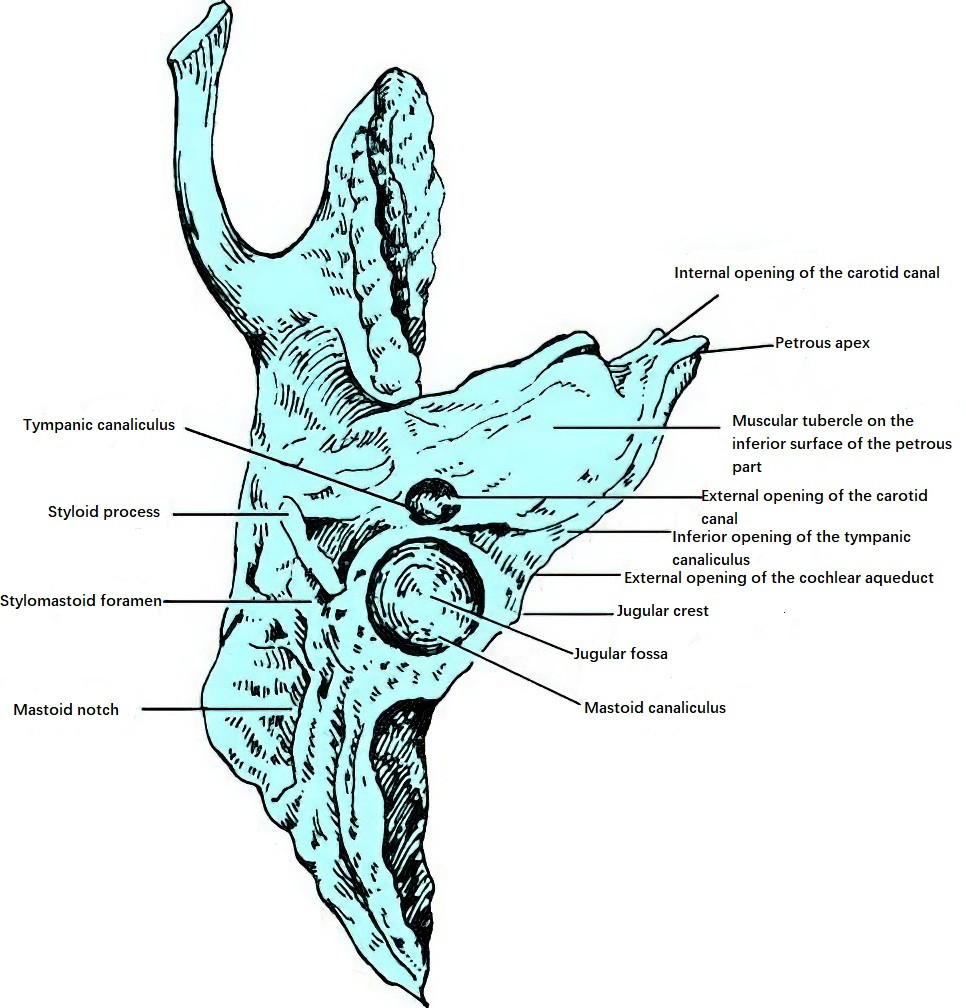
Figure 6 Inferior view of the petrous part
The petrous portion has three borders. The longest is the superior border, which features the superior petrosal groove, accommodating the superior petrosal sinus that connects the sigmoid sinus to the cavernous sinus. At its anterior extremity, the superior border connects to the sphenoid bone via the petro-sphenoidal ligament, which forms a small canal containing the abducent nerve and inferior petrosal sinus. Acute suppurative mastoiditis with well-pneumatized temporal bones can lead to petrositis, causing symptoms such as trigeminal neuralgia and abducent nerve palsy.
The posterior border features the inferior petrosal groove medially, containing the inferior petrosal sinus which connects the cavernous sinus to the jugular bulb. Laterally, this border and the jugular notch of the occipital bone surround the jugular foramen.
Between the petrous portion and the squamous portion, two parallel canals (semi-canals) extend into the tympanic cavity: one for the tensor tympani muscle and the other for the auditory (Eustachian) tube.
Styloid Process
The styloid process is located anterior to the mastoid portion and below the tympanic portion. It is a slender, elongated bony projection that extends anteroinferiorly, measuring approximately 2.5 cm in length on average. The base of the styloid process is encased by the tympanic portion, while its distal end serves as the attachment site for the styloglossus muscle, stylopharyngeus muscle, stylohyoid muscle, stylohyoid ligament, and stylomandibular ligament.
Between the styloid process and the mastoid portion lies the stylomastoid foramen, through which the main trunk of the facial nerve exits the skull. In infants, the mastoid portion is underdeveloped, making the stylomastoid foramen more superficial. This anatomical feature necessitates caution during mastoid surgery, particularly when making a postauricular incision, as excessive downward extension of the incision may risk injuring the facial nerve trunk.
External Ear
The external ear consists of the auricle and the external acoustic meatus.
Auricle
The auricle contains an elastic cartilage framework covered by skin. It is positioned at an angle of approximately 30° to the skull and is symmetrical on both sides. It has an anterior (outer) and a posterior (inner) surface. The anterior surface of the auricle is uneven, with key surface features that include the helix, crus of helix, auricular tubercle (or Darwin tubercle), triangular fossa, scaphoid fossa, cymba conchae, cavum conchae, tragus, antitragus, and intertragic notch. The depression between the tragus and the crus of helix is called the anterior auricular notch. Because this area lacks cartilage, incisions made here can avoid damaging cartilage and provide direct access to the external acoustic meatus and mastoid periosteum. Beneath the antitragus lies the lobule, a cartilage-free area composed of fat and connective tissue. The posterior surface of the auricle is relatively smooth and slightly raised, with its attachment site forming the posterior auricular groove, which serves as an important landmark for otologic surgeries.
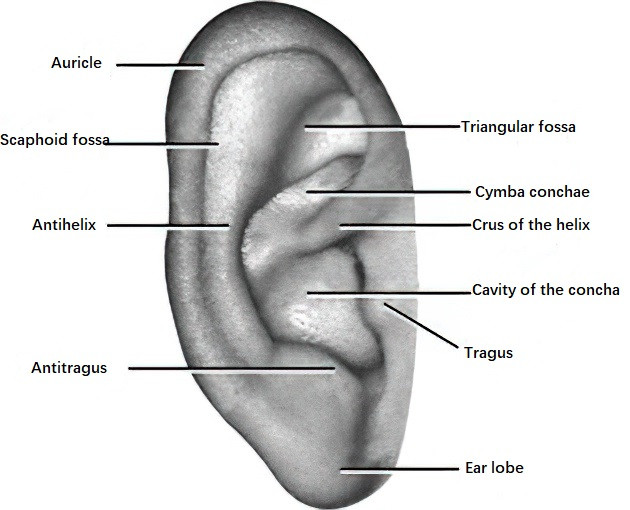
Figure 7 Surface landmarks of the auricle
Figure 8 Left auricle (Posterior view)
Except for the lobule, which is made of fat and connective tissue, the rest of the auricle consists of elastic cartilage covered by perichondrium and skin. The auricular cartilage lacks direct nerve supply, but nerve fibers follow blood vessels and are distributed to the perichondrium. The skin on the anterior surface of the auricle is more closely adhered to the cartilage compared to the posterior surface, with minimal subcutaneous tissue. This tight adherence makes the nerves more prone to compression in cases of swelling due to inflammation, resulting in severe pain. Hematomas or exudates in this area are also difficult to absorb. Trauma or surgery involving the auricle may lead to suppurative perichondritis or even cartilage necrosis, potentially causing auricular deformation. The superficial location of blood vessels in the auricle and the thin skin increase its susceptibility to frostbite.
External Acoustic Meatus
The external acoustic meatus begins at the base of the cavum conchae and ends at the tympanic membrane. It is composed of a cartilaginous portion and a bony portion, forming a slightly S-shaped curve, with a length of approximately 2.5–3.5 cm. In adults, the outer one-third of the canal is cartilaginous, while the inner two-thirds are bony. In newborns, the cartilaginous and bony portions are not fully developed, and the canal is primarily composed of fibrous tissue, making it narrower and more prone to collapse.
Two narrow points exist along the canal: one at the junction between the cartilaginous and bony portions, and the other about 0.5 cm from the tympanic membrane, known as the isthmus of the external acoustic meatus. The outer portion of the canal curves inward, forward, and slightly upward; the middle portion curves inward and backward; and the inner portion curves inward, forward, and slightly downward. These curves make it necessary to lift the auricle posteriorly and superiorly to align the canal during examinations of its deeper parts or the tympanic membrane.
There is a gap in the cartilage of the external acoustic meatus at its posteroinferior portion, which is replaced by connective tissue. The anteroinferior portion of the cartilage often contains 2 to 3 vertical fissures filled with connective tissue, known as the cartilage notches of the external acoustic meatus (Santorini's fissures). These notches enhance the mobility of the auricle but also serve as pathways for infection to spread between the external acoustic meatus and the parotid gland.
The bony portion of the external acoustic meatus is formed superiorly by the squamous part of the temporal bone, with only a thin bony plate separating it from the middle cranial fossa at its deepest point. The anterior wall, inferior wall, and part of the posterior wall of the bony portion are formed by the tympanic part of the temporal bone. The inner end of the bony portion forms the tympanic sulcus, where the fibrous ring of the tympanic membrane's tense part is embedded. The upper portion of the sulcus has a notch, called the Rivinus notch.
The subcutaneous tissue in the external acoustic meatus is minimal, and the skin tightly adheres to the perichondrium and periosteum. Consequently, swelling caused by infection can readily compress nerve endings, leading to severe pain. The skin over the cartilaginous portion is thicker and contains numerous hair follicles, sebaceous glands, and ceruminous glands (specialized sweat glands), which secrete cerumen. The bony portion has thinner skin with fewer hair follicles and ceruminous glands, although it contains a small number of sebaceous glands on its roof. Cerumen, formed by the combination of ceruminous and sebaceous secretions with desquamated skin, provides antimicrobial protection by inhibiting fungal and bacterial growth. The temporomandibular joint lies anterior to the external acoustic meatus, and movements of the cartilaginous portion during jaw opening and closing help expel cerumen and epithelial debris outward. Inflammation of the external acoustic meatus often exacerbates pain during mastication due to traction on the canal.
Nerves, Blood Supply, and Lymphatics of the External Ear
The external ear receives nerve supply primarily from two sources. The auriculotemporal branch of the mandibular nerve innervates the anterior wall of the external acoustic meatus, which explains why toothaches may result in referred otalgia. The auricular branch of the vagus nerve supplies the posterior wall of the canal, accounting for reflexive coughing triggered by stimulation of its skin. Additional innervation comes from the greater auricular nerve and lesser occipital nerve (from the cervical plexus) as well as branches of the facial and glossopharyngeal nerves.
Blood supply to the external ear is provided by the superficial temporal artery, posterior auricular artery, and maxillary artery, all branches of the external carotid artery. Venous drainage flows into the external jugular vein. Some venous drainage may also return to the internal jugular vein. The posterior auricular vein connects with the sigmoid sinus via mastoid emissary veins.
Lymphatic drainage from the external ear flows into the surrounding lymph nodes. Lymph from the anterior auricle drains into the preauricular and parotid lymph nodes, while lymph from the posterior auricle flows into the posterior auricular lymph nodes. Lymph from the lower auricle and inferior wall of the external acoustic meatus drains into the infra-auricular lymph nodes (part of the upper group of the superficial cervical lymph nodes), as well as into the superficial cervical lymph nodes and the upper group of deep cervical lymph nodes.
Middle Ear
The middle ear is situated between the external ear and the inner ear. It is an irregular air-filled cavity and passage located within the temporal bone, comprising four parts: the tympanic cavity, the auditory tube, the mastoid antrum, and the mastoid air cells.
Tympanic Cavity
The tympanic cavity is the largest irregular air-filled cavity within the temporal bone. It is located between the tympanic membrane and the lateral wall of the inner ear. Anteriorly, it communicates with the nasopharynx via the auditory tube, and posteriorly, it communicates with the mastoid antrum and mastoid air cells via the aditus to the mastoid antrum. The tympanic cavity can be divided into three parts based on the upper and lower margins of the tense portion of the tympanic membrane:
- The epitympanum (or attic), which is located above the upper margin of the tense portion of the tympanic membrane.
- The mesotympanum, located between the upper and lower margins of the tense portion, corresponding to the space between the tympanic membrane and the medial wall of the tympanic cavity.
- The hypotympanum, which is located below the lower margin of the tense portion, extending downward to the floor of the tympanic cavity.
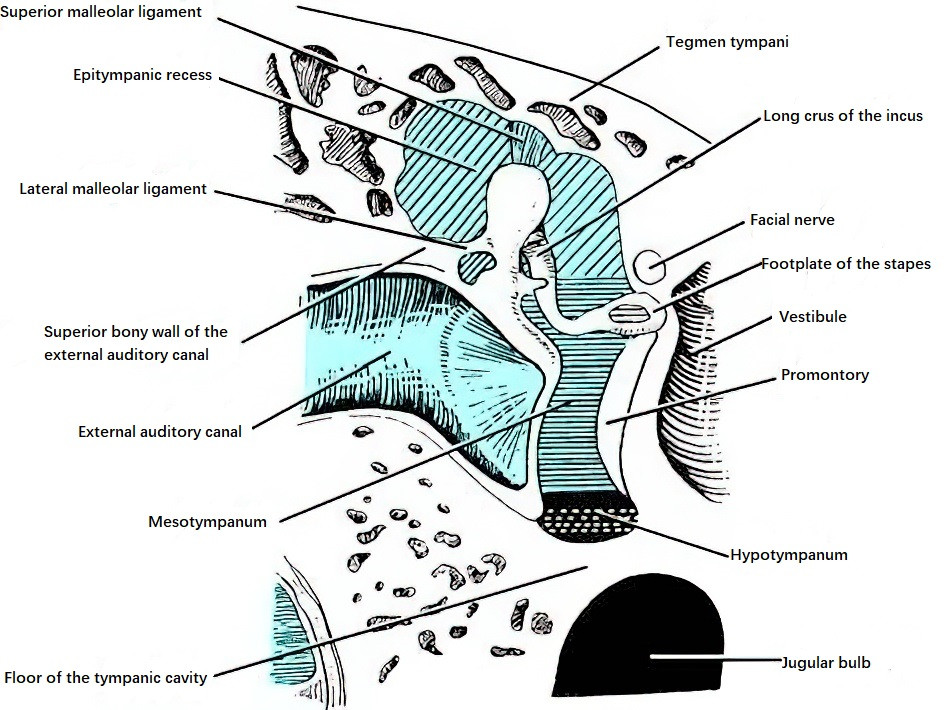
Figure 9 Divisions of the tympanic cavity
The tympanic cavity has an approximate vertical dimension of 15 mm, an approximate anteroposterior dimension of 13 mm, and a transverse dimension ranging from about 6 mm at the epitympanum to about 4 mm at the hypotympanum. The shortest transverse dimension, measuring only about 2 mm, occurs between the umbo of the tympanic membrane and the promontory in the mesotympanum. The cavity has a volume of approximately 1 to 2 mL. Its contents include the auditory ossicles (commonly referred to as the ossicles), nerves, muscles, and ligaments. The tympanic cavity is lined with mucosa, which covers the tympanic membrane, the posterior portion of the promontory, the ossicles, the epitympanum, mastoid antrum, and mastoid air cells. The epithelial layer is predominantly non-ciliated squamous or cuboidal epithelium but transitions to ciliated columnar epithelium elsewhere. Recent research suggests that epithelial cells of the middle ear mucosa are true respiratory epithelial cells.
Six Walls of the Tympanic Cavity
Although the shape of the tympanic cavity is highly irregular, it can be conceptualized as having six walls: the lateral (external), medial (internal), anterior, posterior, superior, and inferior walls.
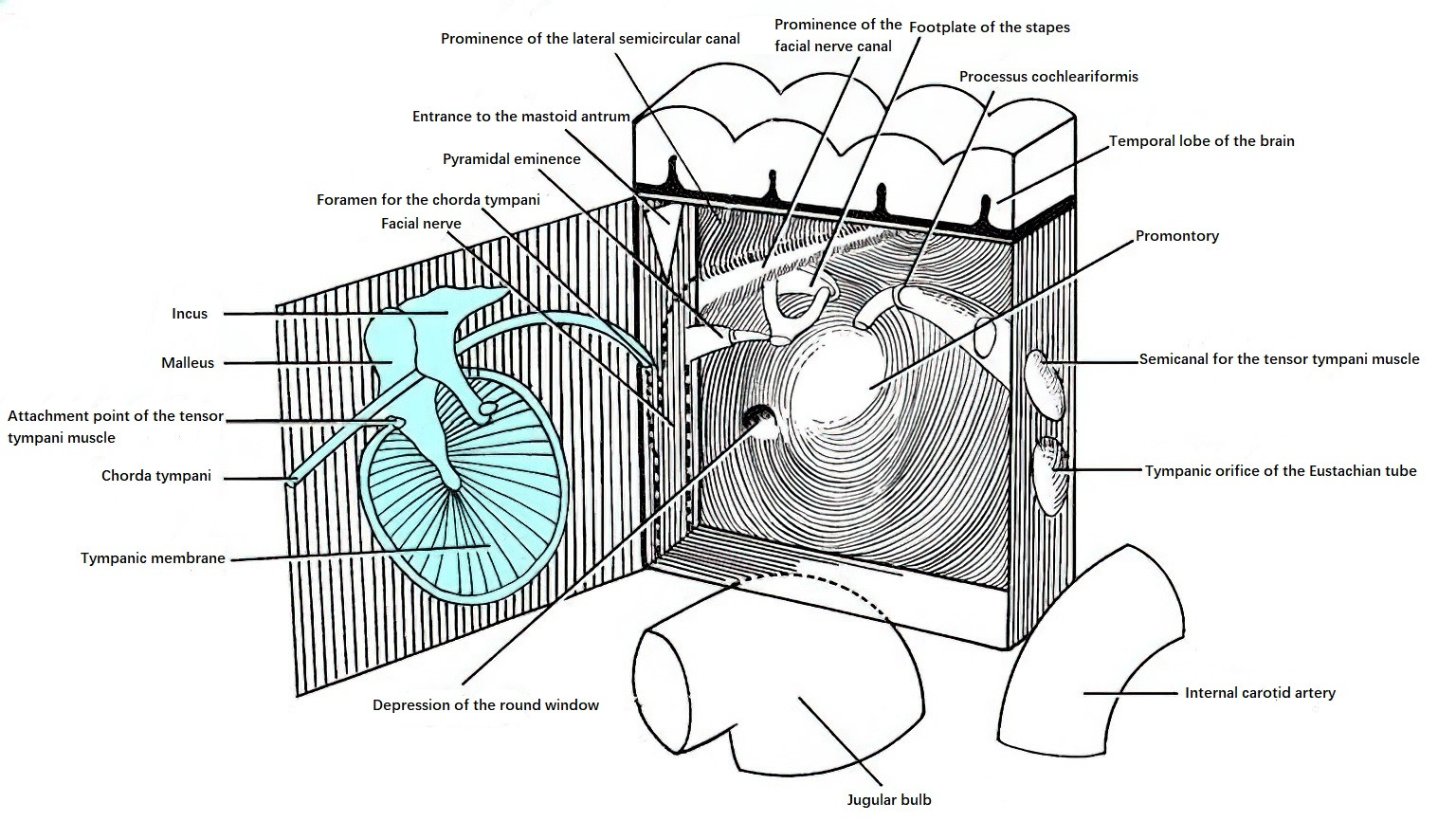
Figure 10 Schematic diagram of the six walls of the tympanic cavity (Right)
Lateral Wall
The lateral wall consists of a bony part and a membranous part. The bony part is smaller and forms the lateral wall of the epitympanum above the tympanic membrane, while the membranous part forms the tympanic membrane itself.
The tympanic membrane, located between the tympanic cavity and the external acoustic meatus, is a thin, semitransparent structure that is oval in adults and rounder in children. It is approximately 9 mm in height, 8 mm in width, and 0.1 mm thick. The lower anterior portion of the tympanic membrane slopes medially, forming an angle of about 45°–50° with the floor of the external acoustic meatus. In newborns and infants up to 5 months old, the tilt is even more pronounced, forming an angle of about 35°.
The peripheral edge of the tympanic membrane is slightly thicker. Most of this edge is attached to the tympanic sulcus via a fibrous ring, forming the pars tensa (tense portion). Superior to the sulcus, where the tympanic notch is located, the membrane attaches directly to the squamous part of the temporal bone, forming the pars flaccida (flaccid portion). The pars tensa is centrally concave, resembling the shape of a funnel, while the pars flaccida is relatively flat.
The tympanic membrane consists of three layers: an epithelial layer externally, a fibrous layer (comprising superficial radiating fibers and deep circular fibers) in the middle, and a mucosal layer internally. The handle of the malleus is embedded within the fibrous layer. The most concave point of the tympanic membrane corresponds to the tip of the malleus handle and is referred to as the umbo.
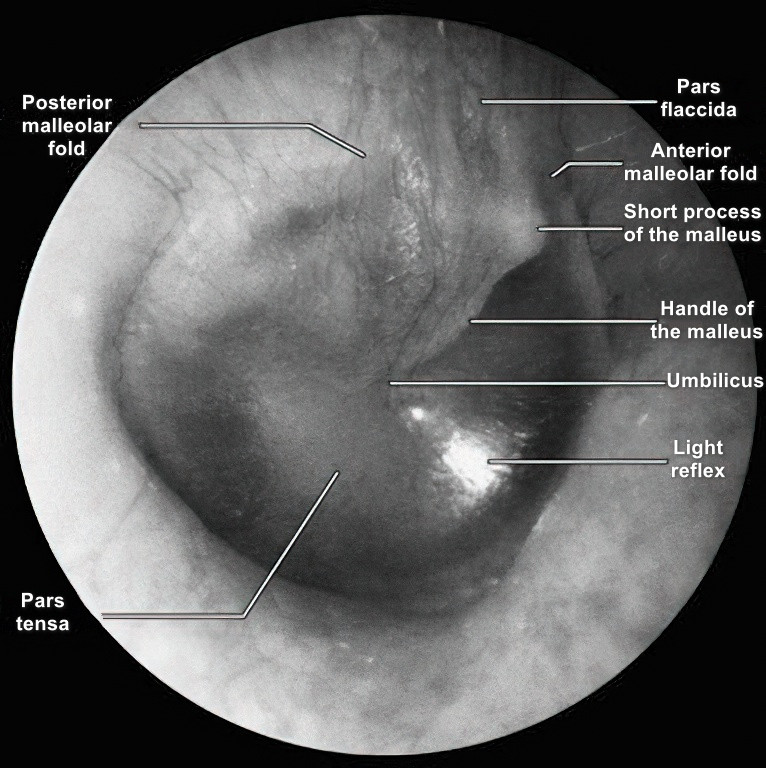
Figure 11 Normal appearance of the tympanic membrane (Right ear)
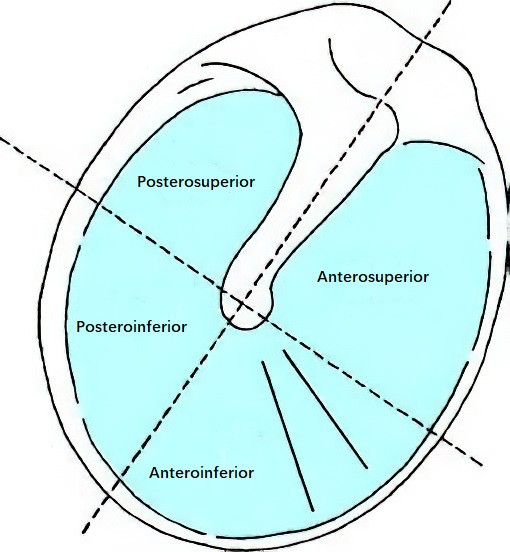
Figure 12 Four quadrants of the tympanic membrane
Extending slightly upwards and anteriorly from the umbo to the upper margin of the pars tensa is a small, grayish-white prominence known as the malleolar prominence, formed by the short process of the malleus. A white linear shadow, called the malleolar stria, represents the shadow of the malleus handle and extends between the umbo and the malleolar prominence on the tympanic membrane. Two mucosal folds extend outward from the malleolar prominence: the anterior malleolar fold extends anteriorly to the anterior end of the tympanic notch, and the posterior malleolar fold extends posteriorly to the posterior end of the tympanic notch. These folds demarcate the boundary between the pars tensa and the pars flaccida.
When viewed with an otoscope, a triangular light reflex, known as the cone of light, extends anteroinferiorly from the umbo to the edge of the tympanic membrane. This reflex results from the concave shape of the tympanic membrane reflecting external light inward. Retraction of the tympanic membrane can distort or obliterate this light reflex. Newborns do not exhibit a visible cone of light due to the pronounced slope of their tympanic membranes. Clinically, the membrane is often divided into four quadrants for documentation: a vertical line through the malleus handle intersects with a horizontal line through the umbo, dividing the membrane into the anterior-superior, anterior-inferior, posterior-superior, and posterior-inferior quadrants.
Medial Wall
The medial wall of the tympanic cavity constitutes the external wall of the inner ear and exhibits several prominences and depressions. The promontory is a large central bulge corresponding to the basal turn of the cochlea. It is covered by the tympanic plexus.
Posterior and superior to the promontory is a depression called the vestibular recess, which has an anteroposterior dimension of approximately 3.25 mm and a vertical dimension of approximately 1.75 mm. The floor of this recess contains the vestibular (oval) window, a bony opening approximately 3.2 mm² in area, sealed by the footplate of the stapes and its surrounding annular ligament, leading to the vestibule of the inner ear.
Inferior and posterior to the promontory lies the cochlear recess, which contains the cochlear (round) window at its upper portion. The cochlear window, also known as the second tympanic membrane, has an area of approximately 2 mm² and opens into the scala tympani of the cochlea. Its membrane closes the window at nearly a right angle to the plane of the stapes footplate.
Posterior to the promontory is the prominence of the lateral semicircular canal, a common site for labyrinthine fistulae. Anterior and slightly superior to the vestibular window is the cochleariform process, a bony structure formed by the curved external end of the semicanal for the tensor tympani muscle. The tendon of the tensor tympani passes outward over this process to attach to the malleus handle where it meets the neck of the malleus.
Anterior Wall
The lower part of the anterior wall is separated from the internal carotid artery by a very thin bony plate, while the upper part contains the openings of the semicanal for the tensor tympani muscle and the tympanic opening of the auditory tube.
Posterior Wall
Also referred to as the mastoid wall, this wall tapers from top to bottom. The vertical segment of the facial nerve runs medial to it. Near the upper part of the posterior wall is a small opening called the aditus to the mastoid antrum, which connects the epitympanum to the mastoid antrum. Inferomedial to the aditus, near the second genu (the bend) of the facial nerve and posterior-superior to the lateral semicircular canal prominence, is a structure known as the incudal fossa. This small cavity accommodates the short process of the incus and serves as an important surgical landmark during middle ear procedures.
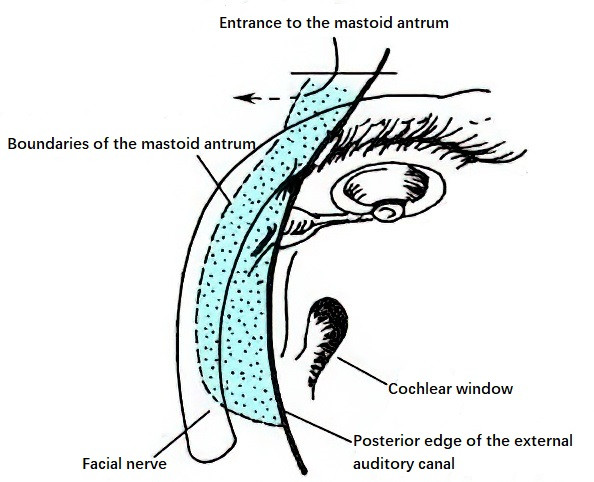
Figure 13 Mastoid antrum
Lower and medial to this wall, roughly at the level of the vestibular window, is a small conical projection called the pyramidal eminence. This eminence contains a canal through which the tendon of the stapedius muscle emerges and attaches to the posterior part of the stapes neck. Between the pyramidal eminence and the tympanic sulcus lies the tympanic opening of the small canal that transmits the chorda tympani nerve, allowing it to enter the tympanic cavity.
The part of the tympanic cavity posterior to the tympanic membrane is called the posterior tympanum, which contains the tympanic sinus (also known as the pyramidal recess) and the facial recess. These regions are common locations for hidden lesions, such as cholesteatomas. The facial recess is bounded medially by the pyramidal eminence, posteriorly by the vertical segment of the facial nerve, and laterally by the bony annular ring of the tympanic membrane and the chorda tympani nerve. Its roof is bordered by the incudal fossa. In cochlear implant surgeries or posterior tympanotomy procedures exposing the facial recess via the mastoid cavity, these structures require careful differentiation.
Superior Wall
The superior wall, also known as the tegmen tympani, forms the roof of the tympanic cavity. It consists of the anterior surface of the petrous part of the temporal bone and separates the tympanic cavity from the middle cranial fossa. Anteriorly, it connects with the roof of the semicanal for the tensor tympani muscle, while posteriorly, it extends to form the roof of the mastoid antrum (tegmen antri). In infants and young children, the petrosquamous fissure located on the tegmen tympani often remains unclosed, allowing small blood vessels of the dura mater to connect with the tympanic cavity, thus providing a potential route for intracranial spread of middle ear infections.
Inferior Wall
The inferior wall, which is narrower than the superior wall, consists of a thin bony plate that separates the tympanic cavity from the jugular bulb. Anteromedially, the wall forms part of the posterior bony wall of the carotid canal. In congenital defects of the tympanic cavity, the jugular bulb may project into the lower tympanum, giving the inferior wall a bluish appearance. In such cases, myringotomy may risk damaging the jugular bulb and causing severe hemorrhage. A small foramen in the inferior wall allows the tympanic branch of the glossopharyngeal nerve to pass through.
Contents of the Tympanic Cavity
The tympanic cavity contains the auditory ossicles, ligaments, and muscles.
Auditory Ossicles
The auditory ossicles represent the smallest bones in the human body and include the malleus, incus, and stapes. Together, they form the ossicular chain, which bridges the tympanic membrane and the vestibular (oval) window, transmitting sound waves from the outer ear to the inner ear.
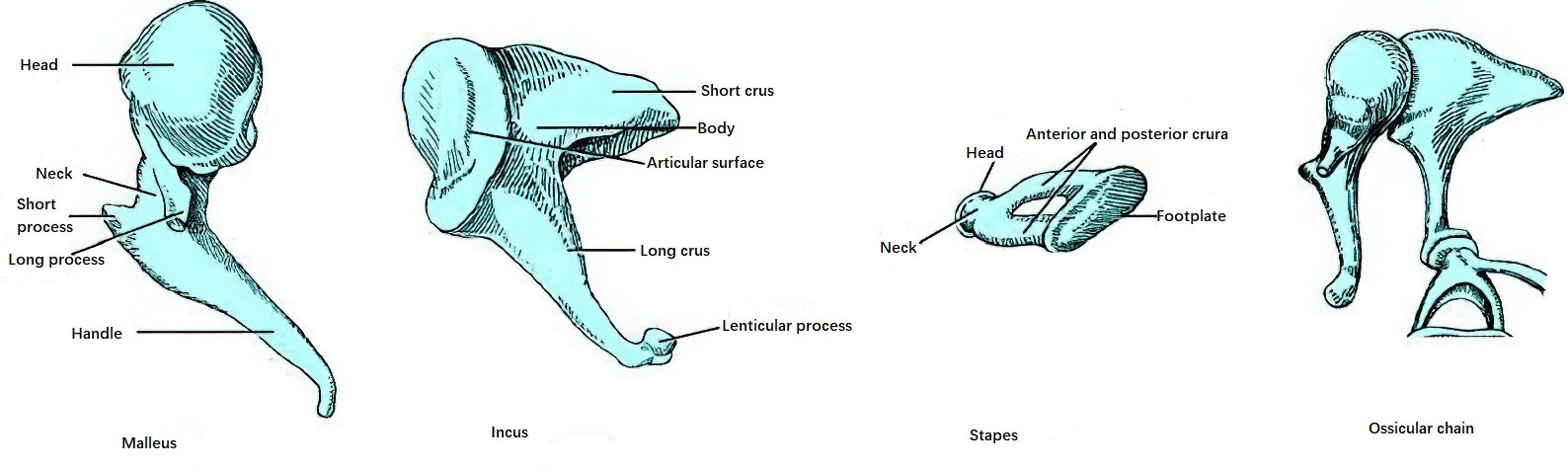
Figure 14 Auditory ossicles
The malleus, shaped like a hammer, is located in the middle and most lateral part of the tympanic cavity. It measures approximately 8–9 mm in length and consists of a head, neck, short process (lateral process), long process (anterior process), and handle. The handle of the malleus lies between the mucosal and fibrous layers of the tympanic membrane, while its head resides in the epitympanum. On the posteromedial aspect of its head is a concave articular facet, which forms the incudomalleolar joint with the body of the incus.
The incus consists of a body, a long limb, and a short limb. The long limb measures about 7 mm, and the short limb measures about 5 mm. The body of the incus is located posterior to the head of the malleus in the epitympanum, where it articulates with the malleus head via the incudomalleolar joint. The short limb projects into the incudal fossa at the base of the mastoid antrum, where it is attached by ligaments. The long limb is located behind and parallel to the handle of the malleus and ends in a medially projecting enlargement called the lenticular process. The lenticular process sometimes separates partially or completely from the long limb, forming what is referred to as the "fourth auditory ossicle." It articulates with the head of the stapes, forming the incudostapedial joint.
The stapes, shaped like a stirrup, consists of a head, neck, anterior crus, posterior crus, and a base (footplate). It measures approximately 3–4 mm in height. The stapes head articulates with the lenticular process of the incus. Its very short neck provides an attachment site for the stapedius muscle tendon. The anterior crus is thinner and straighter than the posterior crus, and each has a deep groove on its medial side. The anterior and posterior crura, along with the footplate, enclose an opening called the obturator foramen. The footplate of the stapes is oval-shaped, measuring about 3 mm in length and 1.4 mm in width. It is attached to the vestibular window via the annular ligament.
Ligaments of the Auditory Ossicles
The ossicles are supported within the tympanic cavity by several ligaments, including the superior malleolar ligament, anterior malleolar ligament, lateral malleolar ligament, superior incudal ligament, posterior incudal ligament, and the annular ligament of the stapes.
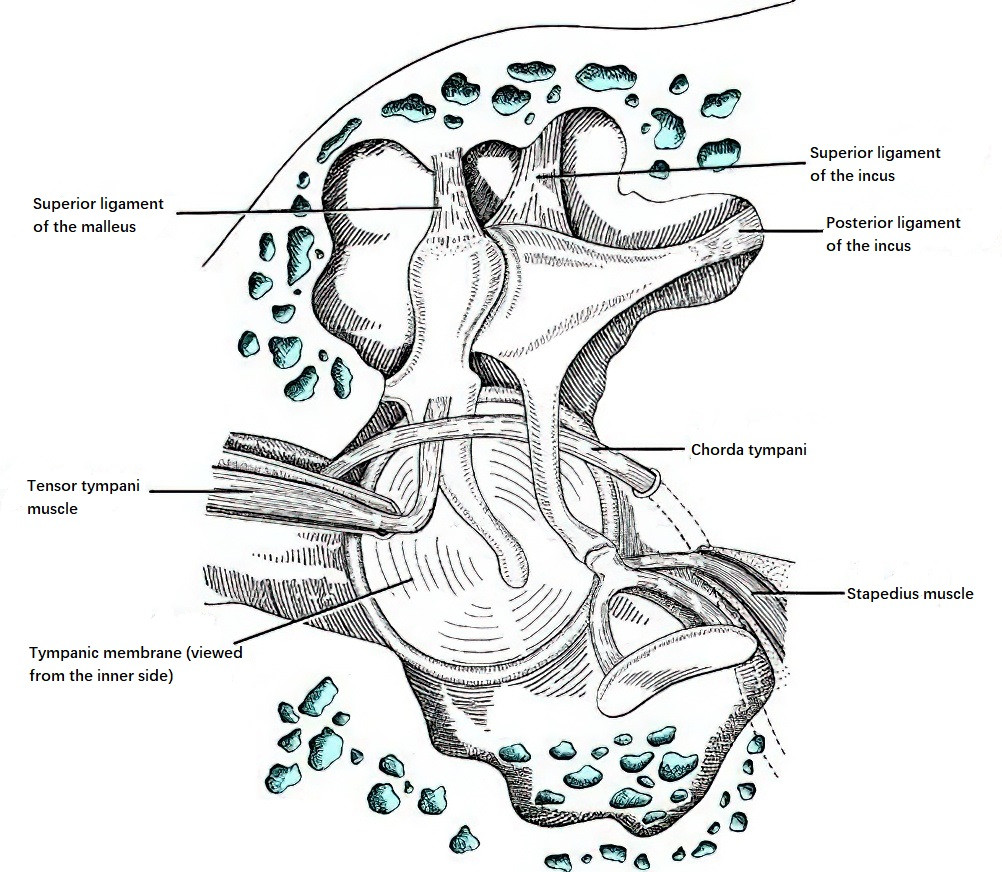
Figure 15 Tympanic muscles and ligaments
Tympanic Muscles
Tensor Tympani Muscle
It originates from the cartilaginous portion of the auditory tube, greater wing of the sphenoid, and walls of the semicanal for the tensor tympani muscle. It inserts just below the neck of the malleus. It is innervated by a small branch of the mandibular division of the trigeminal nerve. When contracted, this muscle pulls the handle of the malleus medially, increasing the tension of the tympanic membrane to protect it from rupture and prevent damage to the inner ear.
Stapedius Muscle
It originates from within the pyramidal eminence on the posterior wall of the tympanic cavity and inserts into the posterior neck of the stapes. It is controlled by the stapedius branch of the facial nerve. Contraction of this muscle pulls the head of the stapes posteriorly, reducing contact between the stapes footplate and the vestibular window, thereby regulating pressure in the inner ear.
Tympanic Recesses and Partitions
The mucosa of the tympanic cavity covers not only its walls and contents but also forms several mucosal folds. Together with the ligaments, muscles, and auditory ossicles, these folds divide the tympanic cavity into several compartments. The narrow communication between the mesotympanum and epitympanum is prone to obstruction when the mucosa swells, which may lead to various pathological conditions. On the other hand, the presence of recesses and partitions in the tympanic cavity can temporarily contain infections or cholesteatomas.
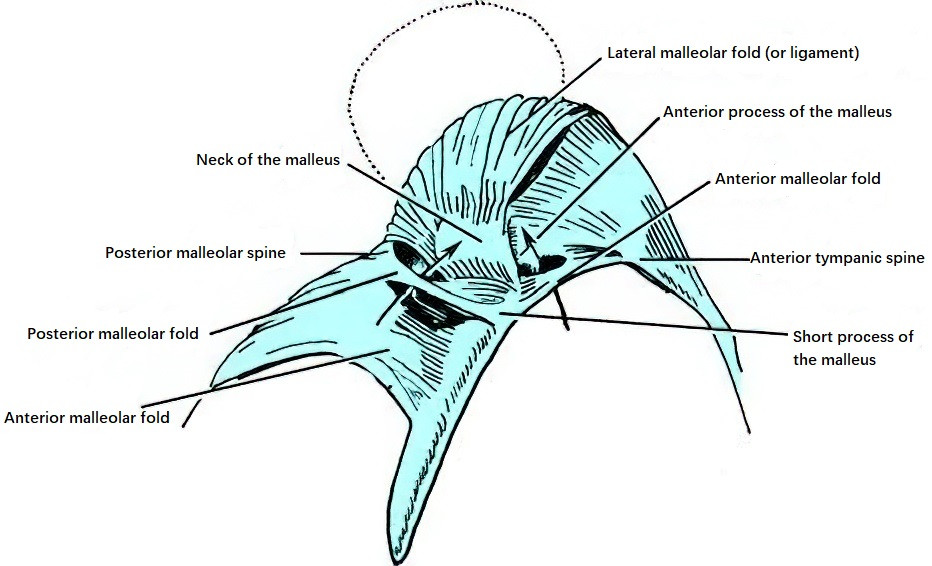
Figure 16 Anterior, posterior, and superior recesses of the tympanic membrane
Tympanic Mucosa
The surfaces of the walls and contents of the tympanic cavity are covered by mucosa, which is continuous with the mucosa of the auditory tube anteriorly and with the mucosa of the mastoid antrum and mastoid air cells posteriorly. The mucosa of the auditory tube exhibits columnar or pseudostratified columnar ciliated epithelium, while that of the mastoid region is cuboidal or low columnar ciliated epithelium. Normal middle ear epithelium contains two types of secretory cells: goblet cells, which secrete mucous, and intermediate cells, which secrete serous fluid. Bacterial infection or environmental disturbances within the tympanic cavity may cause the epithelium to differentiate into stratified squamous epithelium.
Blood Supply and Nerve Innervation of the Tympanic Cavity
Blood Supply
Arterial supply to the tympanic cavity primarily originates from branches of the external carotid artery, including the maxillary artery, posterior auricular artery, middle meningeal artery, ascending pharyngeal artery, and superficial petrosal artery. There is also a minor contribution from the tympanic branch of the internal carotid artery. The vessels of the tympanic membrane are mainly distributed in the pars flaccida, the handle of the malleus, and the surrounding regions of the pars tensa. Inflammation in the tympanic membrane typically begins with congestion in the pars flaccida and subsequently spreads to the handle of the malleus and other parts of the membrane. Venous drainage occurs through the pterygoid venous plexus and the superior petrosal sinus.
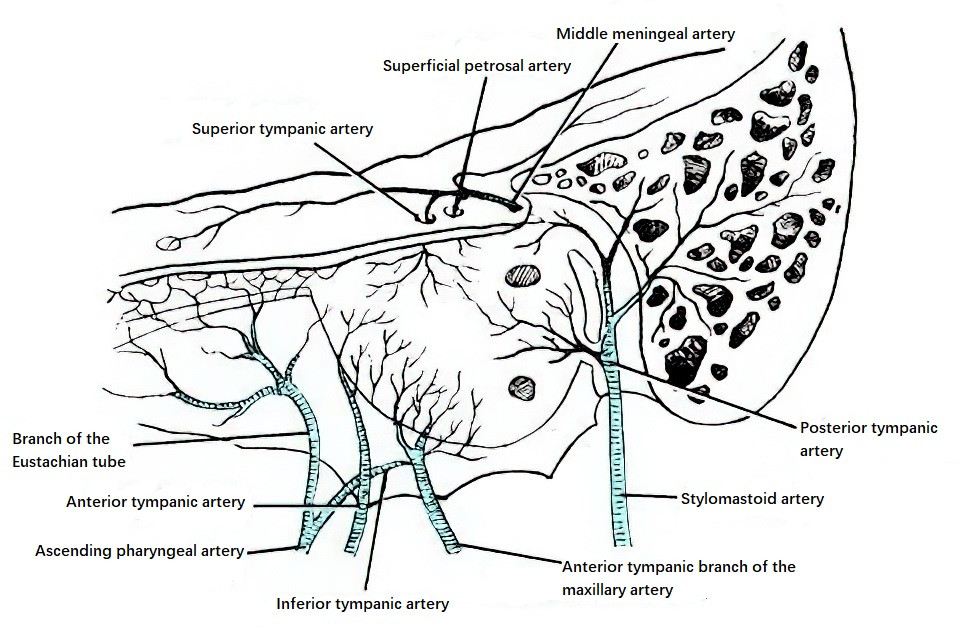
Figure 17 Blood supply of the tympanic cavity
Nerve Innervation
The tympanic cavity is primarily innervated by the tympanic plexus and the chorda tympani nerve.
The tympanic plexus consists of the tympanic branch of the glossopharyngeal nerve and the caroticotympanic nerves from the sympathetic plexus of the internal carotid artery. It is located on the surface of the promontory and is responsible for sensory innervation to the tympanic cavity, auditory tube, and mastoid air cells.
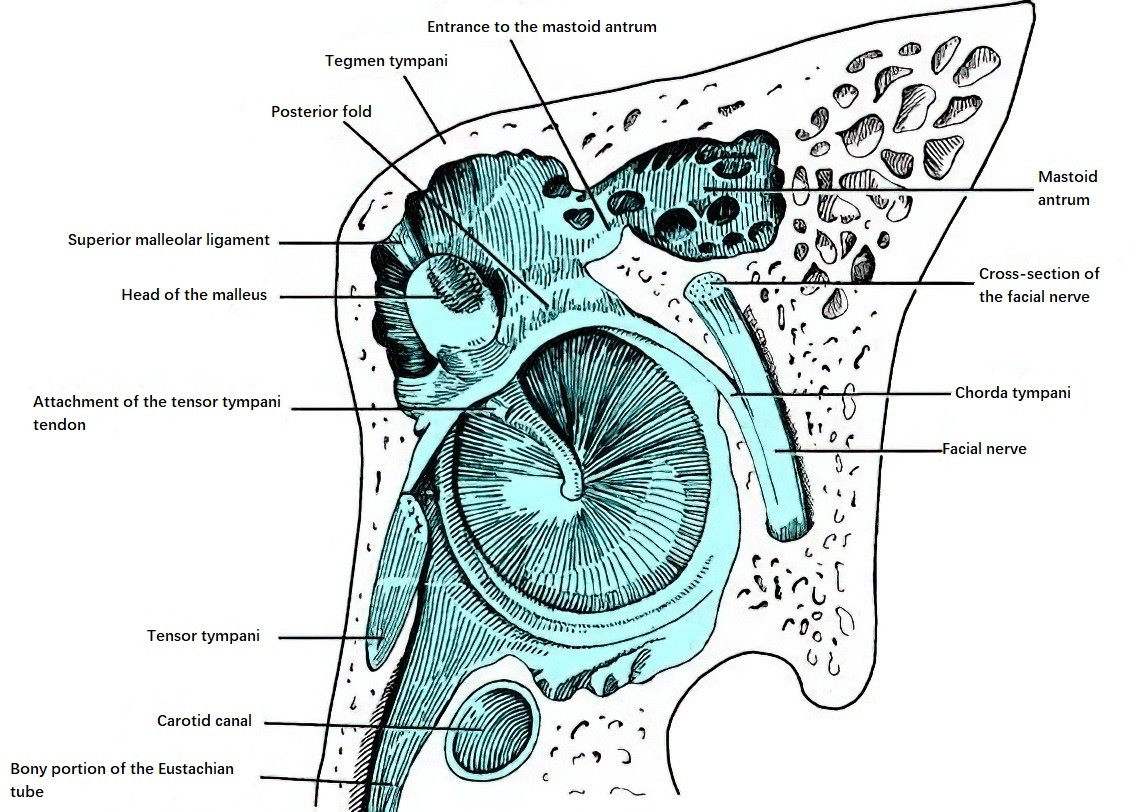
Figure 18 Course of the chorda tympani nerve in the tympanic cavity (Left side)
The chorda tympani nerve, a branch of the facial nerve, branches off from the vertical segment of the facial nerve and travels upward and forward within the canal for the chorda tympani. It enters the tympanic cavity lateral to the pyramidal eminence and passes between the lateral surface of the long limb of the incus and the medial surface of the upper part of the malleus handle. It exits the tympanic cavity anteroinferiorly through the petrotympanic fissure, joining the lingual nerve and providing taste sensation to the anterior two-thirds of the tongue.
Auditory Tube
The auditory tube (pharyngotympanic tube) is located at the junction between the tympanic and petrous parts of the temporal bone. It is lateral to the carotid canal and is separated from the semicanal for the tensor tympani muscle by only a thin bony plate superiorly. It serves as a channel connecting the tympanic cavity with the nasopharynx and measures approximately 35 mm in adults.
The tube consists of an outer one-third bony portion and an inner two-thirds cartilaginous portion. The tympanic opening of the auditory tube is located in the upper part of the anterior wall of the tympanic cavity, while the pharyngeal opening is situated on the lateral wall of the nasopharynx, posteroinferior to the posterior end of the inferior nasal concha. The tube runs medially, anteriorly, and inferiorly, forming an angle of approximately 40° with the horizontal plane and 45° with the sagittal plane.
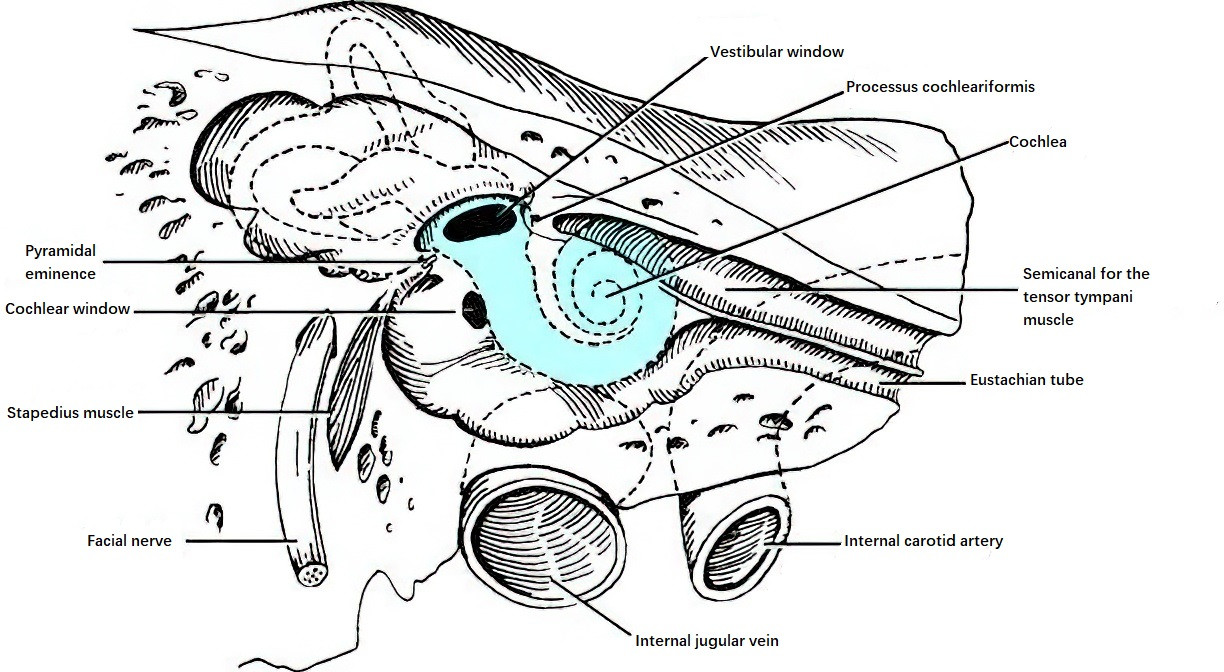
Figure 19 Longitudinal section of the Eustachian tube (Right side)
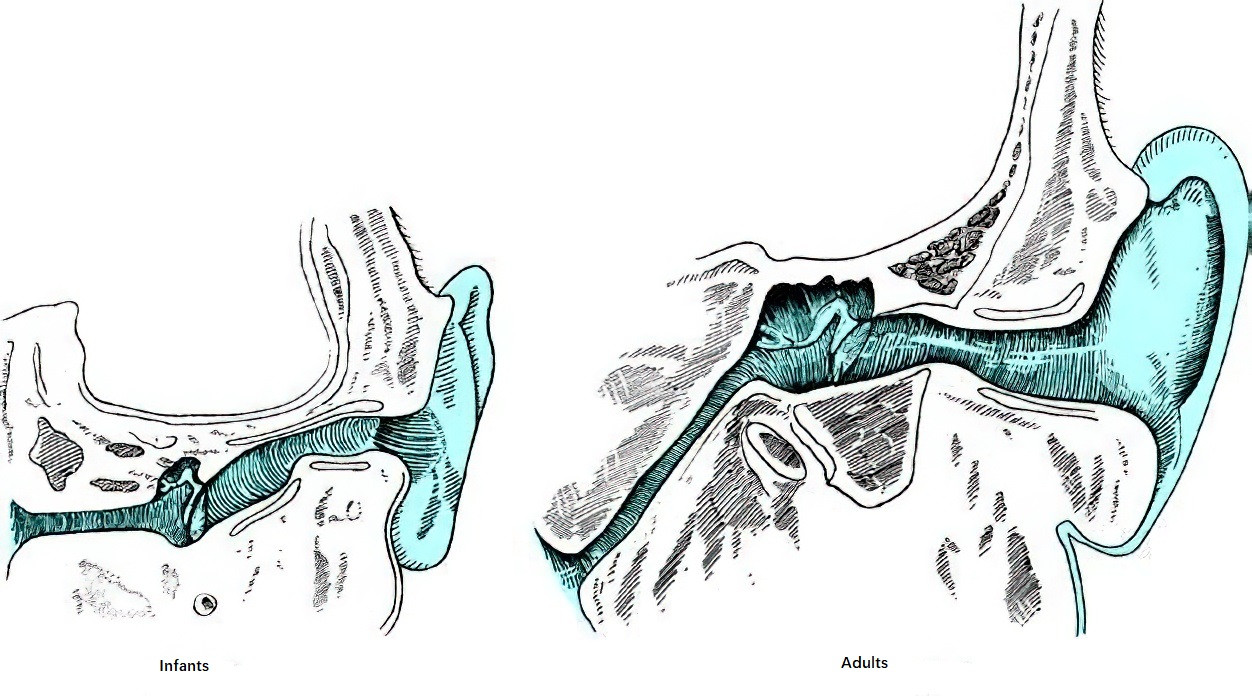
Figure 20 Comparison of the Eustachian tube in adults and infants
The bony part of the tube is patent and has its widest diameter at the tympanic opening, with the diameter narrowing toward the isthmus at the bony-cartilaginous junction. The isthmus, which is the narrowest segment, measures about 2 mm in length and 1 mm in internal diameter. The cartilaginous portion gradually widens toward the pharyngeal opening. The posteromedial and superior walls of the cartilaginous portion are composed of cartilaginous plates, while the anterolateral wall is formed by mucosa and membranous tissue. During rest, the cartilaginous portion remains closed as a slit due to its structural composition.
The tensor veli palatini, levator veli palatini, and salpingopharyngeus muscles originate from the cartilaginous wall or connective tissue membrane of the auditory tube. The first two muscles insert into the soft palate, while the latter inserts into the posterior wall of the pharynx. When these muscles contract during activities such as yawning, swallowing, or singing, they open the pharyngeal end of the tube, allowing pressure equalization between the tympanic cavity and external environment, maintaining a balance in tympanic membrane pressure.
The mucosa of the auditory tube is composed of pseudostratified columnar ciliated epithelium. The ciliary movement is directed toward the nasopharynx, facilitating the drainage of secretions from the tympanic cavity. The mucosal folds in the cartilaginous portion act as a valve to prevent reflux of fluids from the pharynx into the tympanic cavity. The tympanic opening of the auditory tube in adults is positioned approximately 2–2.5 cm higher than the pharyngeal opening. In children, the auditory tube is more horizontally aligned, shorter (roughly half the length of an adult tube), and has a wider internal diameter, making the middle ear more susceptible to infections originating from the nasopharynx.
Mastoid Antrum
The mastoid antrum is an air-filled cavity located in the posterosuperior part of the tympanum. It is lined with ciliated mucosal epithelium and communicates anteriorly with the epitympanum and posteriorly and inferiorly with the mastoid air cells. It is present at birth but is relatively shallow and higher in position in infants, lying almost directly above the external auditory meatus. As the mastoid process develops, the antrum gradually shifts downward.
Anteriorly, the mastoid antrum connects to the epitympanum via the aditus, while posteriorly and inferiorly, it communicates with the mastoid air cells. Superiorly, it is separated from the middle cranial fossa by the tegmen antri. The anterior part of its medial wall features the prominence of the lateral semicircular canal and the prominence of the facial nerve canal. The posterior wall is separated from the posterior cranial fossa by the mastoid air cells and the sigmoid sinus plate. The lateral wall of the antrum is formed by the mastoid cortex, corresponding to the suprameatal triangle (Macewen's triangle).
The size, shape, and position of the mastoid antrum vary significantly among individuals and are directly related to the extent of pneumatization of the mastoid process in different individuals.
Mastoid Process
The mastoid process refers to the outward extension of the tympanum and mastoid antrum. The distribution of mastoid air cells varies among individuals. In well-developed cases, air cells can extend superiorly to the squamous part of the temporal bone, anteriorly above the external auditory canal to the root of the zygomatic process, medially toward the apex of the petrous part, posteriorly to the region behind the sigmoid sinus, and inferiorly into the styloid process.
Based on the degree of pneumatization, the mastoid process can be classified into four types:
- Pneumatic type: The mastoid process is fully pneumatized, containing large air cells with thin intervening bony walls, accounting for approximately 80% of cases.
- Diploetic type: Poorly pneumatized mastoid with small, numerous air cells resembling the diploë of cranial bones.
- Sclerotic type: Non-pneumatized mastoid with dense bone, often attributed to factors like exposure to amniotic fluid, bacterial infections, or local nutritional deficiencies during infancy.
- Mixed type: A coexistence of any two or all three of the above types.
The mastoid process develops gradually from the mastoid antrum postnatally, with considerable extension of air cells by around six years of age. Eventually, numerous interconnected air cells of varying sizes and shapes are formed, lined with non-ciliated epithelial mucosa.
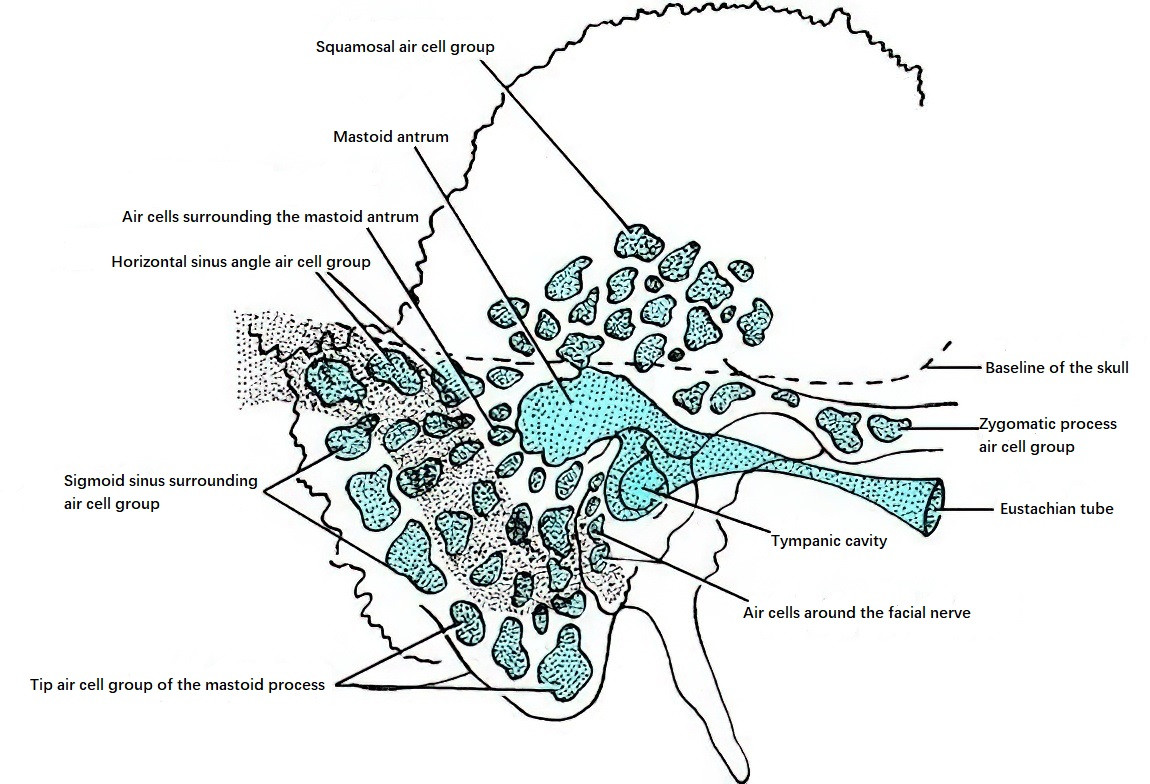
Figure 21 Distribution of mastoid air cells
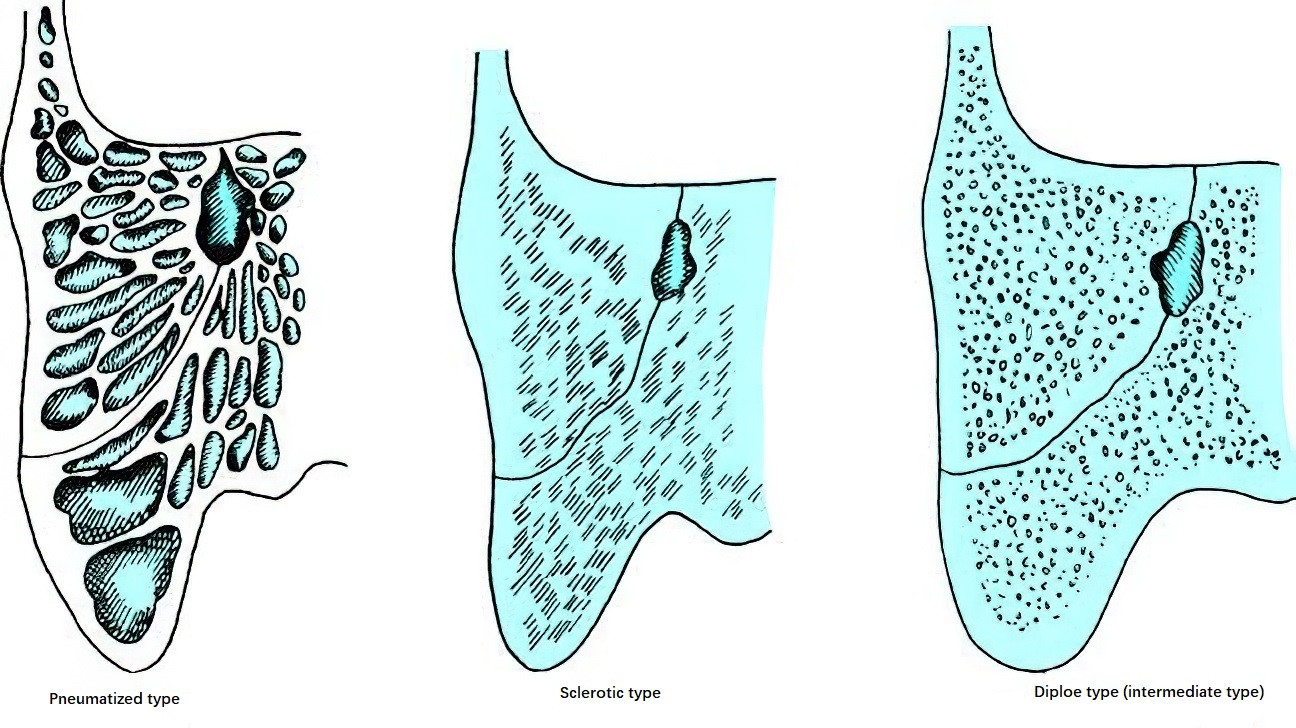
Figure 22 Types of mastoid pneumatization
Near the lower part of the mastoid cavity, close to the mastoid tip, there is a crescent-shaped bony ridge running posteriorly to anteriorly, known as the digastric ridge. This ridge is an important anatomical landmark for locating the vertical segment of the facial nerve. The posteromedial wall of the mastoid cavity bulges slightly forward to form the anterior wall of the sigmoid sinus. Medially to this wall lies the endolymphatic sac, which is typically located below the posterior semicircular canal, anterior to the sigmoid sinus, and posterior to the vertical segment of the facial nerve.
Inner Ear
The inner ear, also known as the labyrinth, is a structurally intricate and precise system embedded in the petrous part of the temporal bone. It houses the auditory and vestibular organs and is anatomically and functionally divided into three parts: the vestibule, the semicircular canals, and the cochlea.
Histologically, the inner ear consists of the osseous labyrinth and the membranous labyrinth, which are similar in shape. The membranous labyrinth is enclosed within the osseous labyrinth. The sensory receptors for hearing and balance reside in the membranous labyrinth. The space between the osseous labyrinth and the membranous labyrinth is filled with perilymph, while the membranous labyrinth itself contains endolymph. Perilymph and endolymph are distinct and do not interconnect.
Osseous Labyrinth
The osseous labyrinth is made up of dense bone and includes three main parts: the cochlea (medially), the osseous semicircular canals (posterolaterally), and the vestibule (connecting the two centrally).
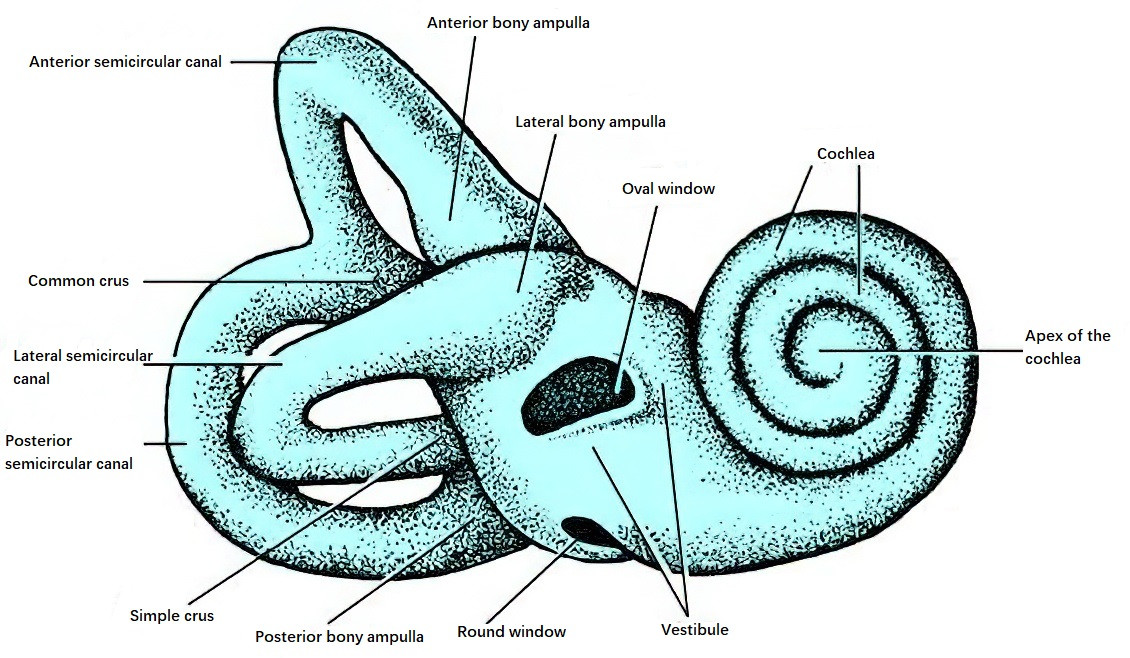
Figure 23 Bony labyrinth (Right side)
Vestibule
The vestibule, located between the cochlea and the semicircular canals, is roughly oval-shaped and contains the utricle and saccule. The anteroinferior part of the vestibule is narrower and connects to the scala vestibuli of the cochlea via an oval aperture, whereas the posteriosuperior part is wider and contains five openings of the three semicircular canals.
The lateral wall of the vestibule forms part of the medial wall of the tympanic cavity and contains the oval window (vestibular window) and the round window (cochlear window). Its medial wall faces the internal acoustic meatus and constitutes the meatal fundus.
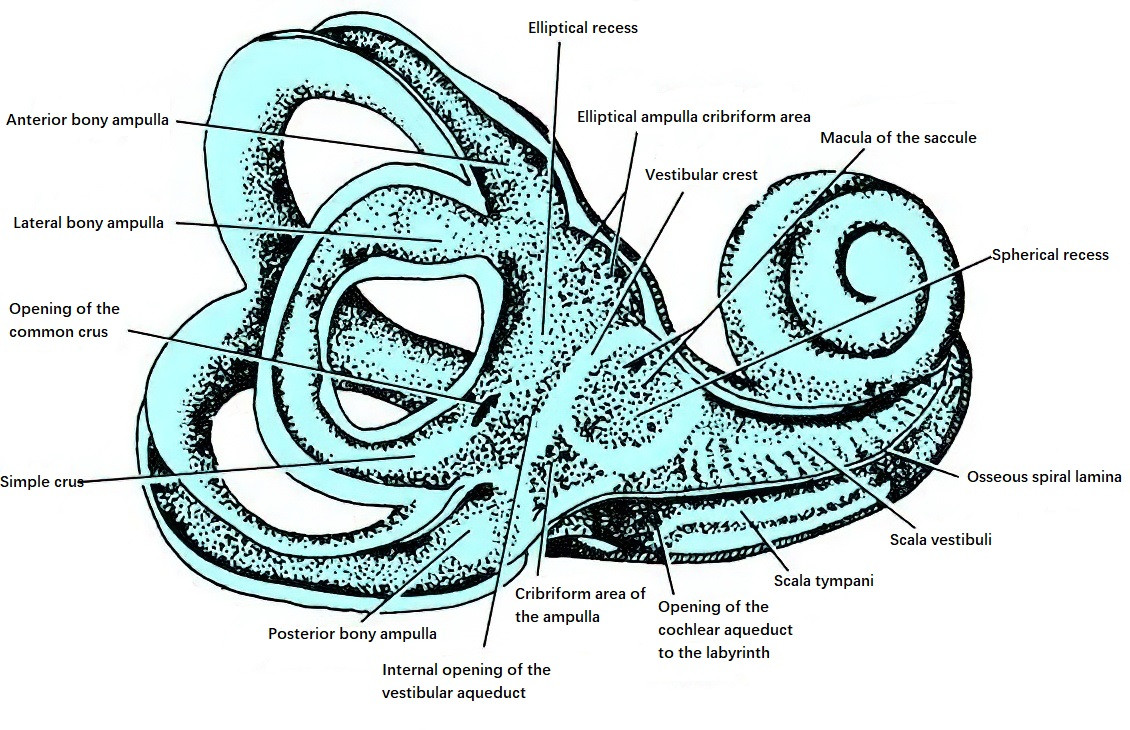
Figure 24 Schematic anatomy of the vestibule
Inside the vestibule is an oblique bony ridge, known as the vestibular crest, running from the anterosuperior to the posteroinferior part. Anterior to the crest is the spherical recess, which houses the saccule and contains small perforations referred to as the foramen of the middle macula (saccular macula). Posterior to the crest is the elliptical recess, which accommodates the utricle, with several small openings called the foramen of the superior macula (utricular macula).
Inferior to the elliptical recess is the opening of the vestibular aqueduct, which communicates with the endolymphatic sac. The external opening of the vestibular aqueduct (cranial opening) lies at the bottom of the slit-like petrous portion (internal acoustic meatus), measuring less than 2 mm in diameter. The size of the vestibular aqueduct is related to the degree of temporal bone pneumatization. Posteroinferior to the vestibular crest is a partition with a small fossa called the cochlear recess, which lies between the hook-like extension of the spiral lamina (spiral hook) and the posterior semicircular canal.
The bony roof of the vestibule contains a segment of the facial nerve (the labyrinthine portion).
Osseous Semicircular Canals
There are three osseous semicircular canals per side—lateral (horizontal), superior (anterior vertical), and posterior (posterior vertical)—which are positioned at approximately right angles to each other. These canals are located above and behind the vestibule and form about two-thirds of a ring. The lateral semicircular canal measures approximately 12–15 mm, while the superior and posterior canals are longer, measuring around 15–20 mm and 18–22 mm, respectively.
Each canal has a diameter of approximately 0.8–1 mm, except at one end, where it expands to form an ampulla (with a diameter twice that of the canal). The ampullated ends of the lateral and superior canals open into the anterosuperior vestibule, while the ampullated end of the posterior canal opens into the posteroinferior vestibule. The non-ampullated ends of the superior and posterior semicircular canals converge to form a common limb (the common crus), which opens into the middle part of the inner vestibular wall. The non-ampullated limb of the lateral canal opens below the common crus. In total, the three canals connect to the vestibule through five openings.
Each canal is oriented at distinct angles:
- Ipsilateral canals sit at right angles to each other.
- The lateral canals on both sides are oriented in the same plane and form a 30° angle with the horizontal plane.
- The planes of the anterior canals on each side are perpendicular to each other and are perpendicular to the long axis of their respective petrous parts.
- The planes of the posterior canals on each side are also perpendicular to each other but are parallel to the long axis of their respective petrous parts.
- The plane of one anterior semicircular canal is parallel to the plane of the contralateral posterior semicircular canal.
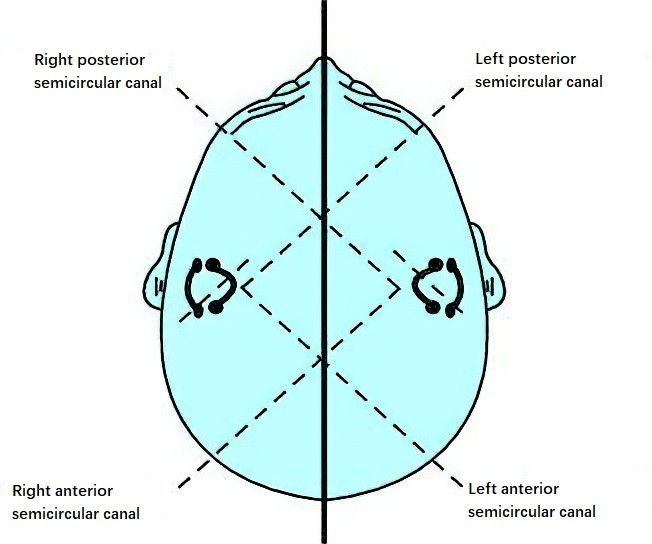
Figure 25 Schematic positions of the bony semicircular canals
Cochlea
The cochlea is located anterior to the vestibule and resembles a snail shell. It consists of a central axis known as the modiolus and a surrounding osseous cochlear duct.
The osseous cochlear duct spirals around the modiolus for 2.5 to 2.75 turns. The base of the cochlea forms the promontory, which bulges into the middle ear cavity. The cochlear apex, or cupula, points anterolaterally toward the opening of the auditory tube and is approximately 5 mm high.
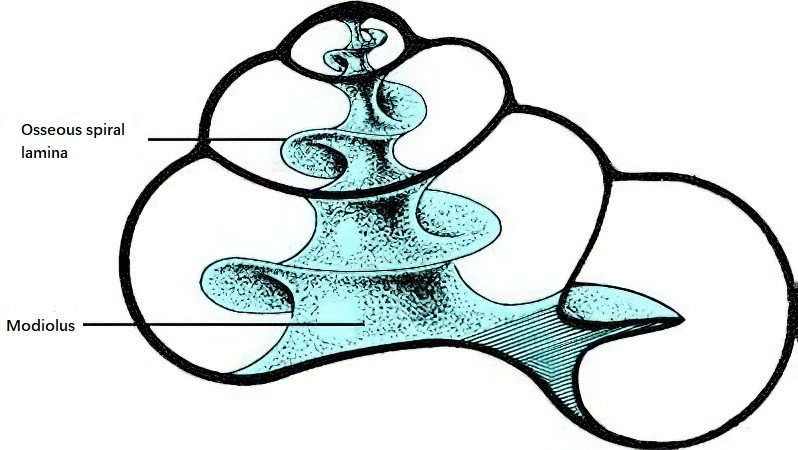
Figure 26 Cochlea
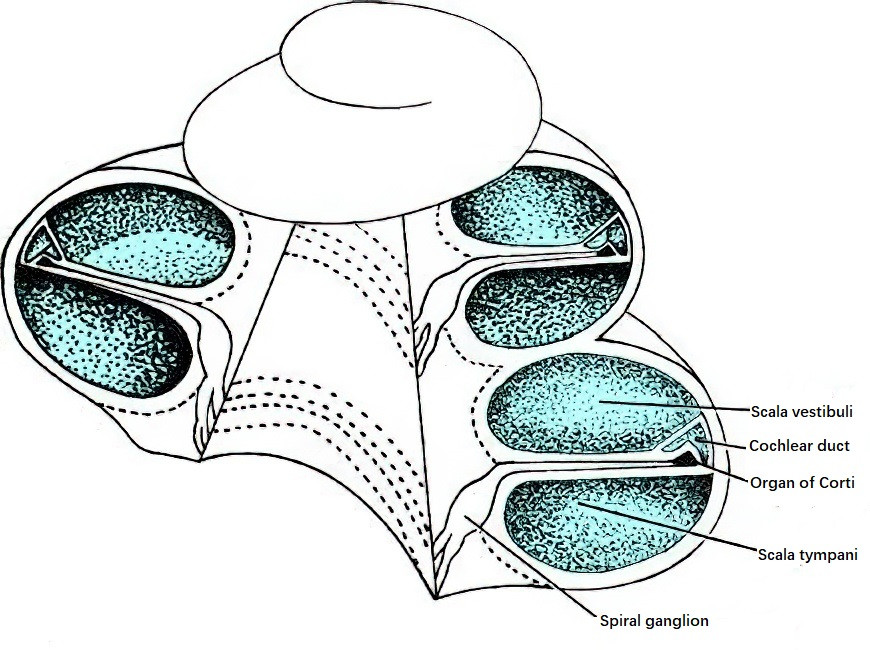
Figure 27 Section view of the cochlea
Within the osseous cochlear duct, the bony spiral plate emanates from the modiolus and extends outward, dividing the duct into upper and lower chambers. Additionally, the cochlear duct is divided into three compartments by the vestibular membrane and the basilar membrane:
- Scala vestibuli (upper chamber), beginning at the vestibule.
- Scala media (middle chamber or membranous cochlear duct), which houses the organ of Corti and is part of the membranous labyrinth.
- Scala tympani (lower chamber), beginning at the round window.
The scala vestibuli and scala tympani communicate at the helicotrema, located at the apex of the cochlea. Cochlear nerve fibers access the spiral ganglion through small foramina between the modiolus and the bony spiral plate. Near the round window, the cochlear aqueduct connects the perilymph of the scala tympani to the subarachnoid space, with its external opening situated in a triangular depression between the jugular fossa and the carotid canal.
Membranous Labyrinth
The membranous labyrinth consists of membranous ducts and sacs, suspended in perilymph by fine reticular fibers, forming a closed system known as the endolymphatic system. It can be divided into the utricle, saccule, membranous semicircular canals, and cochlear duct, which are interconnected. Within the membranous labyrinth are structures responsible for balance and hearing, including the maculae, cristae ampullares, endolymphatic sac, and cochlear duct.
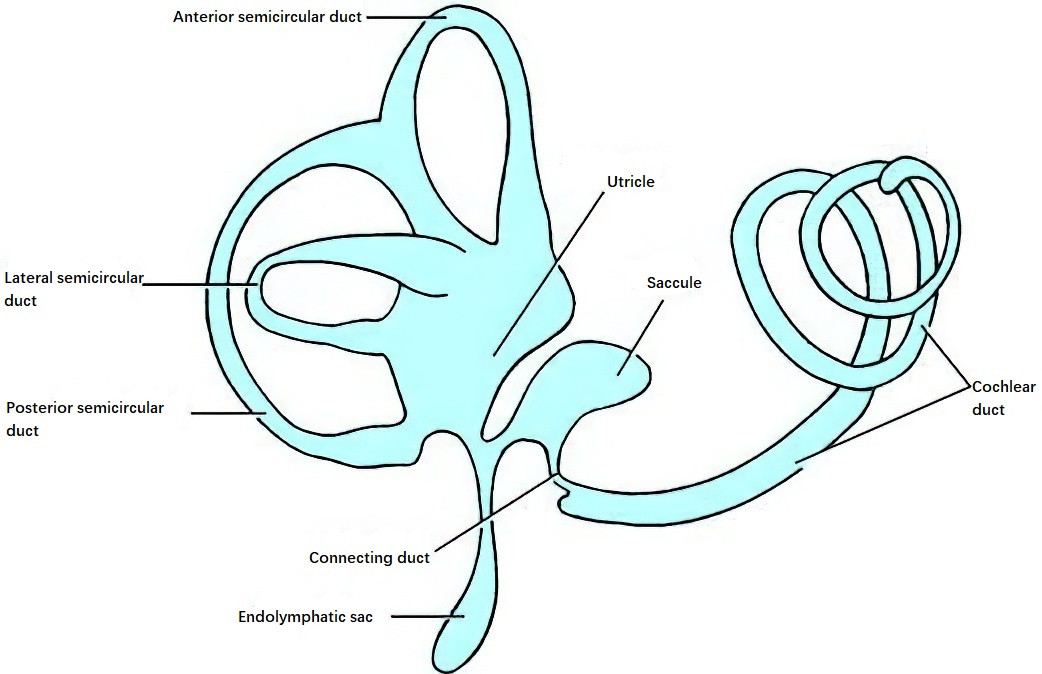
Figure 28 Membranous labyrinth
Utricle
The utricle is located in the posterosuperior part of the vestibule, where it attaches to the elliptical recess through connective tissue, microvasculature, and nerve fibers from the utricular branch of the vestibular nerve. On the floor and anterior wall of the utricle is the macula utriculi (utricle macula), a region of thickened sensory epithelium that is innervated by the utricular branch of the vestibular nerve. The macula utriculi, also referred to as the static macula, is responsible for detecting linear acceleration and head position relative to gravity. The sensory epithelium contains supporting cells and hair cells, with a gelatinous layer covering its surface. The stereocilia of the hair cells project into this gelatinous layer.
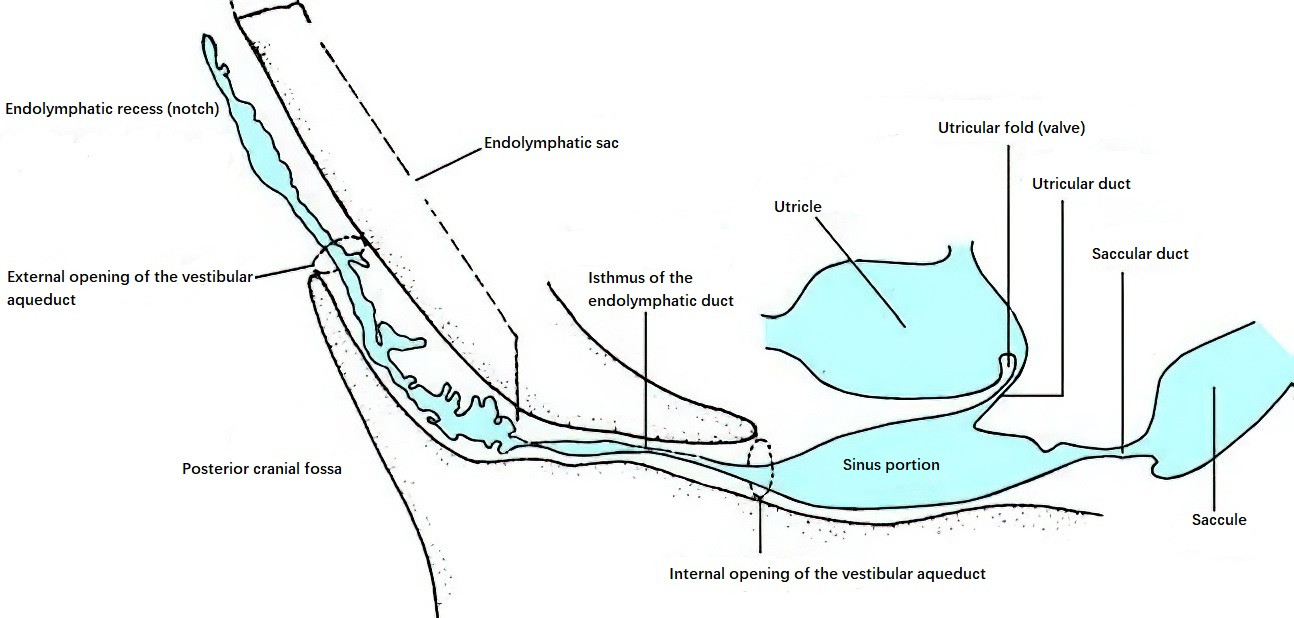
Figure 29 Endolymphatic system
Five openings on the posterior wall of the utricle connect it to the three semicircular canals. On the medial side of the anterior wall is the utriculosaccular duct, which links the utricle to the saccule and the endolymphatic duct. The endolymphatic duct terminates in the endolymphatic sac, which resides within the dura mater in the posterior petrous portion of the temporal bone (posteroinferior to the internal acoustic meatus). A valve near the utricle in the endolymphatic duct prevents backflow.
The endolymphatic sac is partially located within the vestibular aqueduct and partially between the two layers of the dura mater. The sac’s inner surface contains numerous folds with abundant small blood vessels and connective tissue, while the part of the sac between the dura mater layers has a smoother wall.
Saccule
The saccule, slightly smaller than the utricle, is spherical in shape and situated in the anteroinferior part of the vestibule within the spherical recess. On its anteromedial wall lies the macula sacculi (saccular macula), also known as the static macula, which is innervated by the saccular branch of the vestibular nerve. The saccule connects to the endolymphatic duct and the utriculosaccular duct at its posteroinferior side. Its lower end communicates with the cochlear duct through the ductus reuniens.
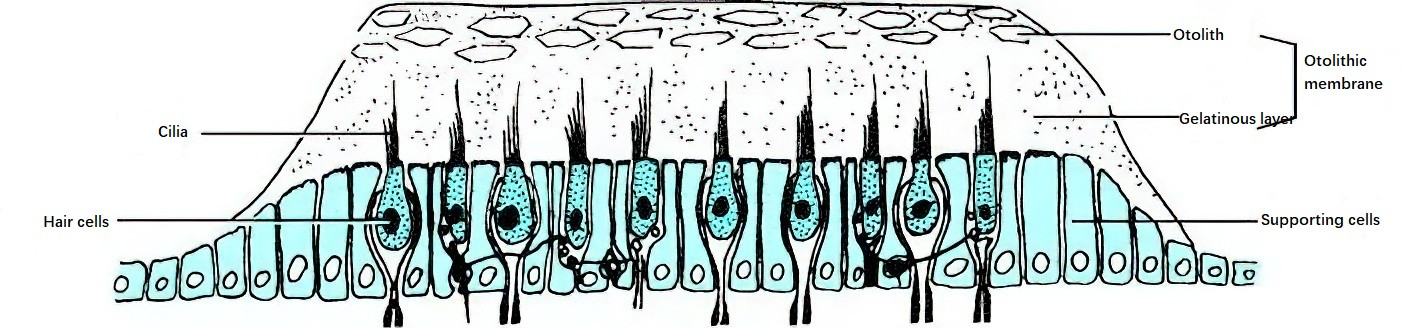
Figure 30 Macula
The maculae utriculi and maculae sacculi are oriented perpendicular to each other and have identical construction. Each consists of supporting cells and hair cells, the cilia of which are shorter compared to those in the cristae ampullares. A gelatinous layer known as the otolithic membrane overlies the hair cells. This membrane contains particles called otoliths (also referred to as "statoconia" or "otoconia"), which are composed predominantly of calcium carbonate crystals and protein.
Membranous Semicircular Canals
The membranous semicircular canals are attached to the lateral walls of the osseous semicircular canals and occupy about one-quarter of the lumen. They have five openings that communicate with the utricle. Near the ampullated ends of the osseous semicircular canals, the membranous semicircular canals expand to form membranous ampullae, which contain transverse crescent-shaped sensory ridges known as the cristae ampullares.
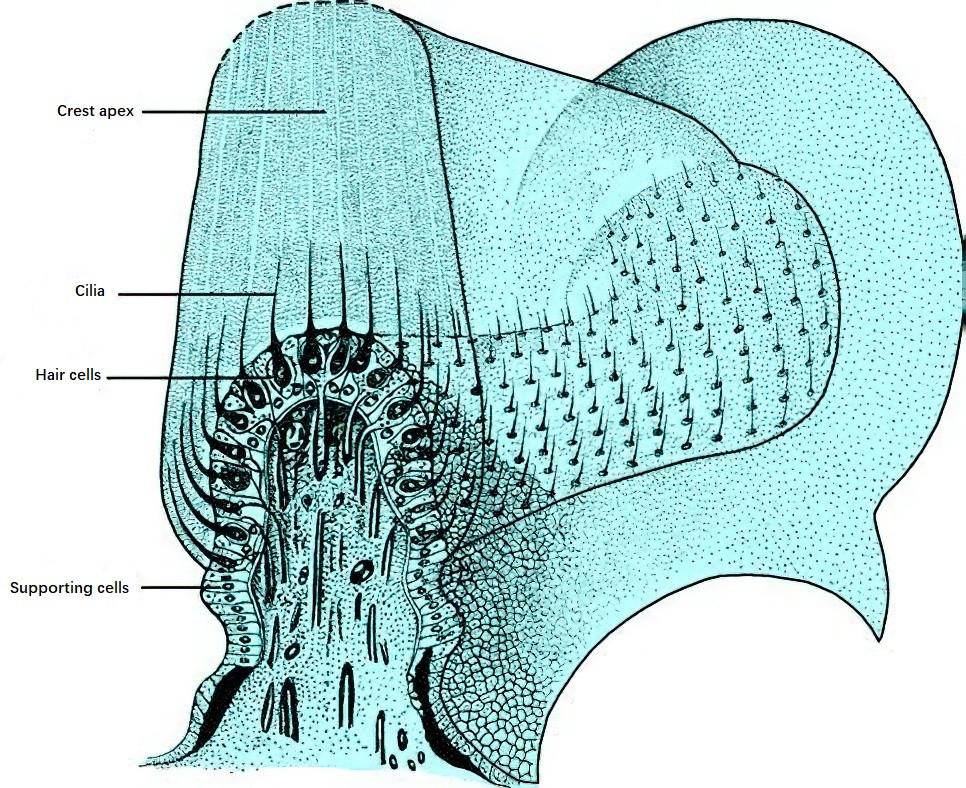
Figure 31 Ampullary crest
The cristae ampullares consist of highly specialized sensory epithelium made up of supporting cells and hair cells. The cilia of the hair cells are longer than those of the utricle and saccule and often cluster into bundles that project into a dome-shaped gelatinous mass known as the cupula. The cupula is composed of glycosaminoglycans and has a density similar to that of the surrounding endolymph (approximately 1.003), which allows it to move in response to the motion of the endolymph.
Hair cells in the cristae ampullares are classified into two types based on their ultrastructure:
- Type I hair cells: Flask-shaped, concentrated in the central region of the crista.
- Type II hair cells: Cylindrical, more abundant in the peripheral areas of the crista.
In the crista ampullaris of the lateral semicircular canal, the kinocilia of the hair cells are oriented toward the utricle. In the anterior and posterior canals, however, the kinocilia are oriented away from the utricle. Movement of the stereocilia in the direction of the kinocilium increases the firing rate of the hair cell, creating an excitation state in the semicircular canal. Conversely, bending of the stereocilia away from the kinocilium decreases the firing rate, leading to an inhibition state.
Hair cells in the maculae of the utricle and saccule convert mechanical stimuli generated by linear acceleration into electrical signals. Both Type I and Type II hair cells are anchored by supporting cells. The base of each stereocilium is embedded in an apical cuticular plate, while the base of each kinocilium lacks a cuticular plate and is instead anchored in a basal body.
The otolithic membrane, which overlies the hair cells, has a dual-layer composition. The outer layer is made up of calcium carbonate crystals forming the otoliths, while the inner layer is gelatinous and composed predominantly of glycosaminoglycans. The otoliths increase the mass of the otolithic membrane. When stereocilia bend toward the kinocilium, the hair cells depolarize, leading to an increased firing rate of the vestibular nerve and subsequent excitation. By contrast, when the stereocilia bend away from the kinocilium, the hair cells hyperpolarize, reducing the firing rate of the vestibular nerve and creating an inhibitory state.
Endolymphatic Duct and Sac
The endolymphatic duct lies between the vestibule and the endolymphatic sac, forming a Y-shaped structure. It connects to the utricle and saccule through the utricular duct and the saccular duct, respectively. The terminal dilated portion of the endolymphatic duct forms the endolymphatic sac, which is partly located within the vestibular aqueduct and partly between the two layers of dura mater near the posterior semicircular canal and the sigmoid sinus. The sac's wall, where it lies between the dura layers, is smooth and is referred to as the smooth part.
The epithelial lining of the inner wall of the endolymphatic sac is composed of two types of cells. Type I cells, which account for approximately 80%, form the majority of the middle portion and feature numerous villi projecting into the sac lumen. These cells are primarily involved in resorption. Type II cells are less abundant, comprising about 20%, and have fewer villi. Additionally, the endolymphatic sac contains phagocytes with cytoplasm rich in digestive vacuoles, lipid droplets, multivesicular bodies, and phagocytic bodies. These phagocytes play a role in the degradation of metabolic byproducts and cellular debris from the endolymph.
Membranous Cochlear Duct
The membranous cochlear duct, located between the bony spiral lamina and the outer wall of the osseous cochlear duct, is a spiral membranous tube in the cochlea. It is also referred to as the scala media and is filled with endolymph. The cochlear duct is a blind-ended structure, with its two ends sealed off. The end at the apex of the cochlea is termed the apical blind end, and the basal end near the vestibule is termed the vestibular blind end.
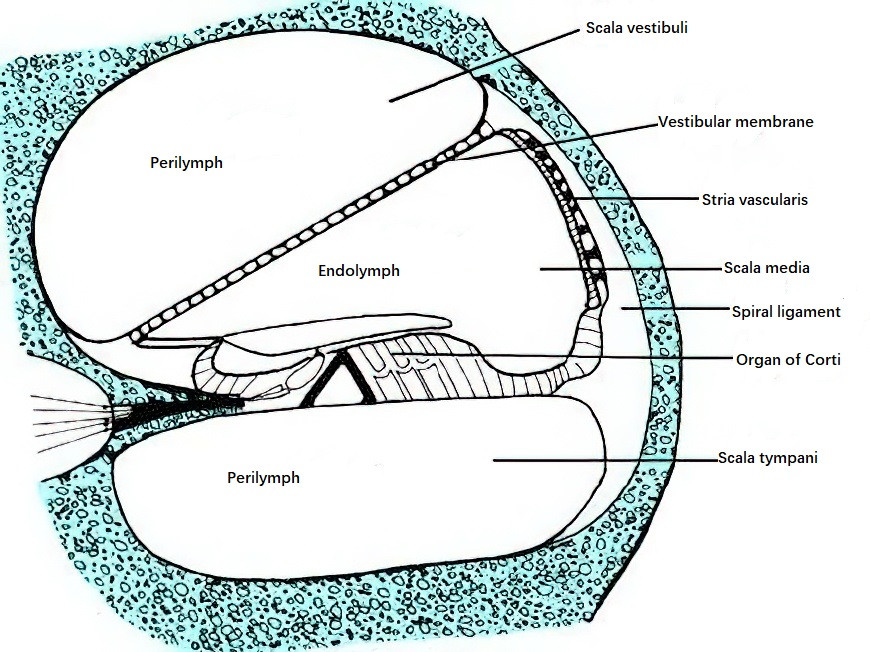
Figure 32 Cross-section of the cochlea
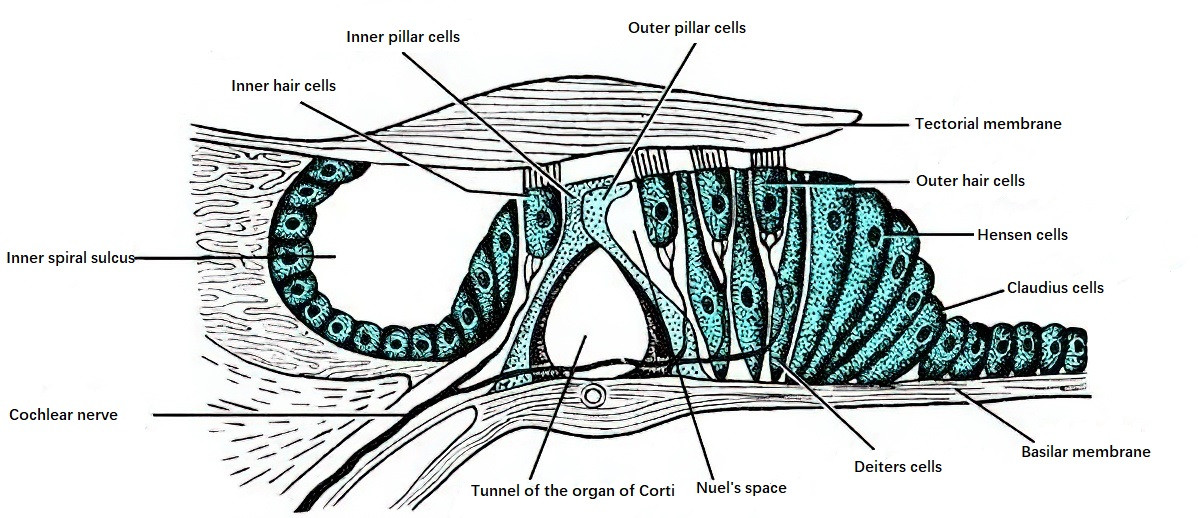
Figure 33 Schematic diagram of the organ of corti
The transverse section of the cochlear duct appears triangular, with three walls:
- The vestibular membrane (Reissner’s membrane), forming the upper wall. It originates from the bony spiral lamina and extends upward and outward to attach to the lateral wall of the osseous cochlear duct.
- The spiral ligament, forming the outer wall. This region is covered by a pseudostratified epithelium that contains abundant blood vessels, known as the stria vascularis.
- The basilar membrane, forming the lower wall. It is made up of two parts: the periosteum of the upper surface of the bony spiral lamina, which thickens to form the spiral limbus, and the basilar crest, where the membrane attaches to the outer wall of the cochlear duct.
The organ of Corti (or spiral organ), the primary sensory organ for hearing, is located upon the basilar membrane. This structure extends along the entire length of the cochlear duct from base to apex, measuring approximately 32 mm in total length.
The basilar membrane widens from the base of the cochlea to the apex, while the bony spiral lamina, along with its corresponding basilar crest, gradually narrows. Within the organ of Corti, there are fluid-filled spaces such as the tunnel of Corti, Nuel’s space, and the outer tunnel, which are filled with Cortilymph. This fluid has properties similar to perilymph and communicates with it via small pores in the lower layer of the bony spiral lamina and openings for cochlear nerve fibers that lead to the scala tympani. Other spaces within the membranous labyrinth are filled with endolymph.
The Cortilymph primarily serves as the nutritional source for the hair cells of the organ of Corti, as its ionic composition resembles that of perilymph. Conversely, the utricle and saccule maculae, as well as the cristae ampullares of the semicircular canals, are nourished by endolymph.
The organ of Corti houses the sensory cells for hearing, including inner and outer hair cells, supporting pillar cells, and the tectorial membrane. Inner hair cells, which are flask-shaped, form a single row on the side closer to the modiolus and number approximately 3,500. Outer hair cells, which are cylindrical in shape, form three or more rows on the outer side and number approximately 12,000. These are the auditory sensory cells.
On the apices of the hair cells is a thick cuticular plate, in which the roots of the stereocilia are embedded. The inner hair cells have two rows of stereocilia arranged in a birdwing-like formation, while the outer hair cells feature three rows of stereocilia arranged in a W-shaped, tiered pattern. The height of hair cells varies along the length of the basilar membrane; from the base to the apex of the cochlea, the hair cells gradually become taller. At the cochlear base (the high-frequency region), the stereocilia of hair cells are shorter, while near the apex, the stereocilia become gradually longer.
The varying height of the cochlear hair cells and the gradient in stereocilia length likely form the morphological foundation for the cochlear frequency-place mapping and tuning functions.
Vascular Supply of the Inner Ear
The blood supply to the labyrinth is primarily derived from the labyrinthine artery, also known as the internal auditory artery, which typically originates from the anterior inferior cerebellar artery of the vertebrobasilar system. In certain individuals, it may originate directly from the basilar artery or the vertebral artery. Upon entering the internal acoustic meatus, the labyrinthine artery divides into two branches:
- The anterior vestibular artery, which supplies the superior and lateral semicircular canals, as well as the upper portions of the utricular and saccular maculae.
- The common cochlear artery, which supplies the posterior semicircular canal and the lower portions of the utricular and saccular maculae.
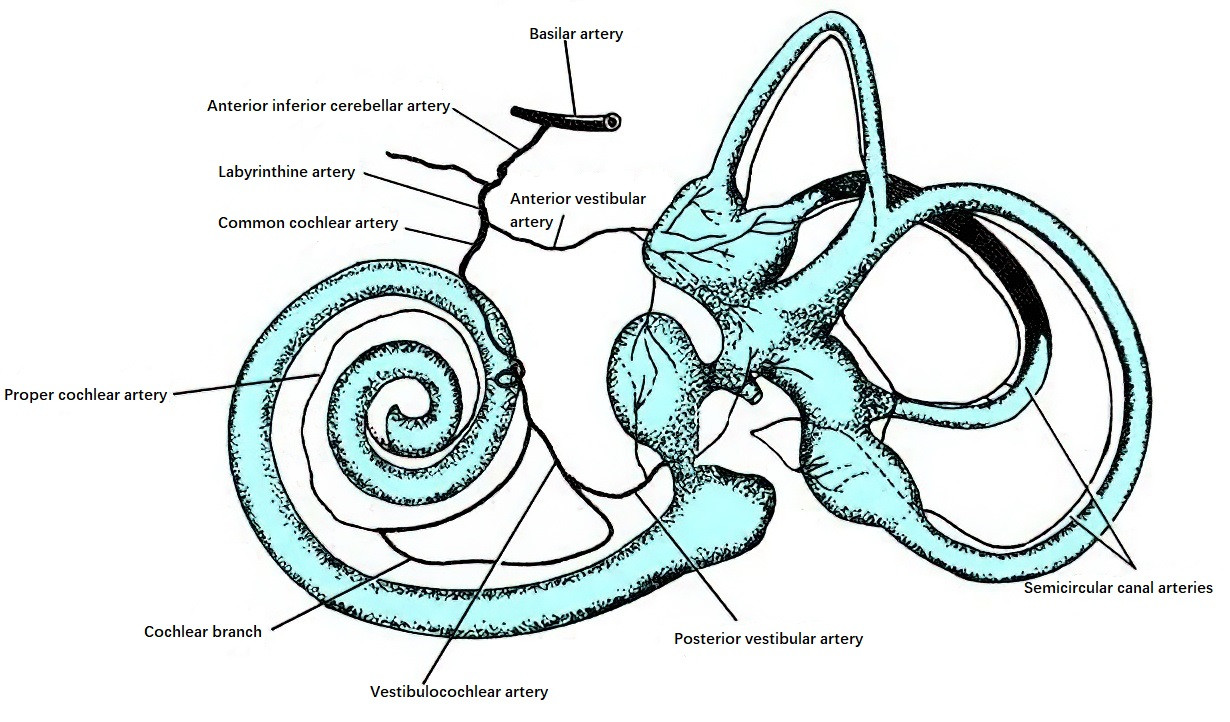
Figure 34 Blood supply of the inner ear
The venous drainage of the inner ear differs from its arterial distribution. Venous blood from this region drains into the labyrinthine vein, vestibular aqueduct vein, and cochlear aqueduct vein, which in turn empty into the sigmoid sinus, superior petrosal sinus, or internal jugular vein.
The Eighth Cranial Nerve and Its Conduction Pathways
The eighth cranial nerve exits the brainstem at the junction of the medulla and pons and enters the internal acoustic meatus alongside the facial nerve, where it divides into an anterior branch (cochlear nerve) and a posterior branch (vestibular nerve).
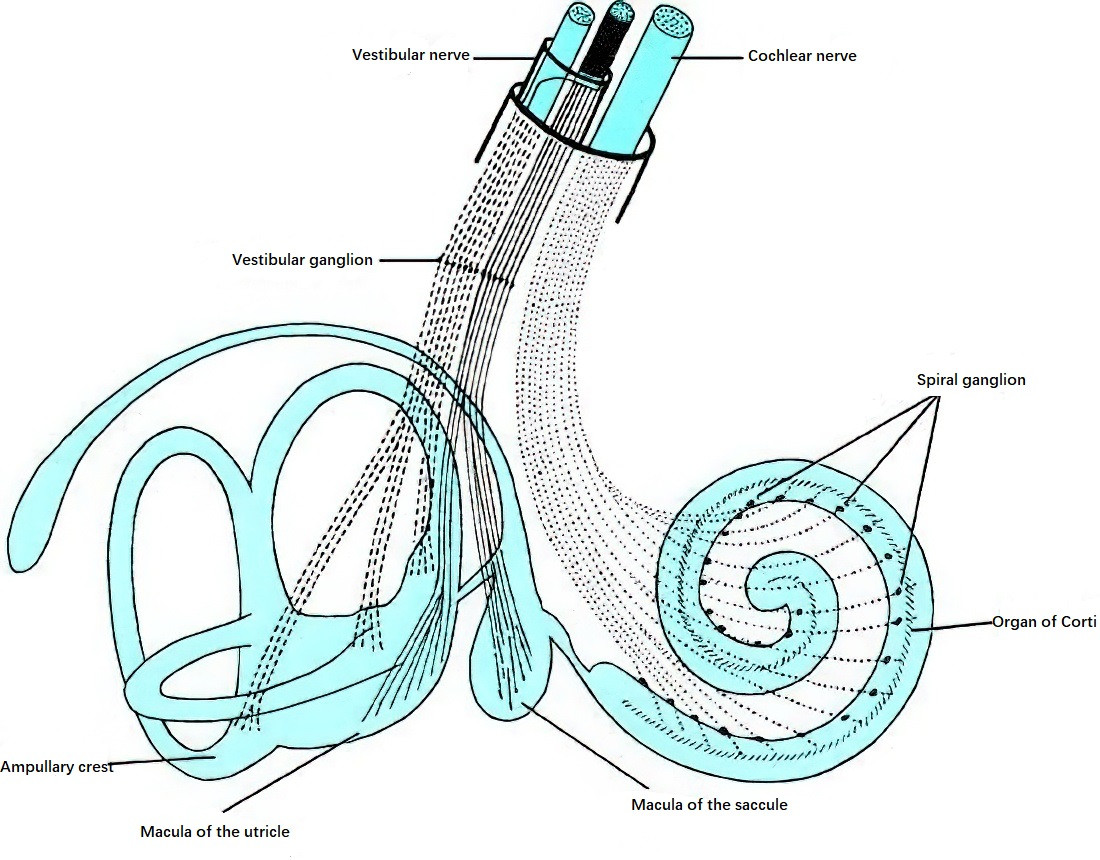
Figure 35 Distribution of the eighth cranial nerve in the inner ear
Cochlear Nerve and Its Conduction Pathway
The cochlear nerve enters the modiolus of the cochlea and branches into numerous fibers. Fibers that terminate in the basal and middle turns of the cochlea pass through spiral foramina around the modiolus to reach the spiral ganglia in the spiral canals. Fibers that terminate in the apical turn pass through the central canal of the modiolus to reach the spiral ganglia. The spiral ganglia, located where the modiolus connects to the osseous spiral lamina, are composed of bipolar neurons.
The central processes of the bipolar neurons form the cochlear nerve. The outer layer of the nerve bundle is comprised of fibers originating from the basal turn of the cochlea, which transmit high-frequency sound signals. The central portion of the nerve contains fibers from the apical turn, which transmit low-frequency sound signals. The peripheral processes of the bipolar neurons in the spiral ganglia penetrate the osseous spiral lamina and innervate the hair cells of the organ of Corti. The cochlear nerve consists of afferent fibers, which transmit sensory signals from the cochlea to the central nervous system, and efferent fibers, which send signals from the central nervous system to the cochlea.
The conduction pathway of the cochlear nerve proceeds as follows:
- The central processes of the bipolar neurons in the spiral ganglia form the cochlear nerve after passing through the cribriform area at the floor of the internal acoustic meatus. The cochlear nerve passes through the internal acoustic meatus to enter the cranial cavity and terminates at the dorsal and ventral cochlear nuclei located at the junction of the medulla and pons. These bipolar neurons represent the first-order neurons for the auditory pathway, with their cell bodies situated in the spiral ganglia.
- The second-order neurons have their cell bodies in the ventral and dorsal cochlear nuclei. Their axons project to bilateral superior olivary complexes, with some fibers directly entering the lateral lemniscus and terminating in the nuclei of the lateral lemniscus.
- The third-order neurons originate from the superior olivary nuclei and project afferent fibers along the lateral lemniscus to terminate in the inferior colliculus. Fibers from the nuclei of the lateral lemniscus also ascend as third-order neurons, terminating in the medial geniculate bodies and, in part, in the nuclei of the contralateral inferior colliculus.
- The fourth-order neurons project from the inferior colliculus or the medial geniculate bodies via the internal capsule to the auditory cortex, located in the superior transverse temporal gyrus of the temporal lobe.
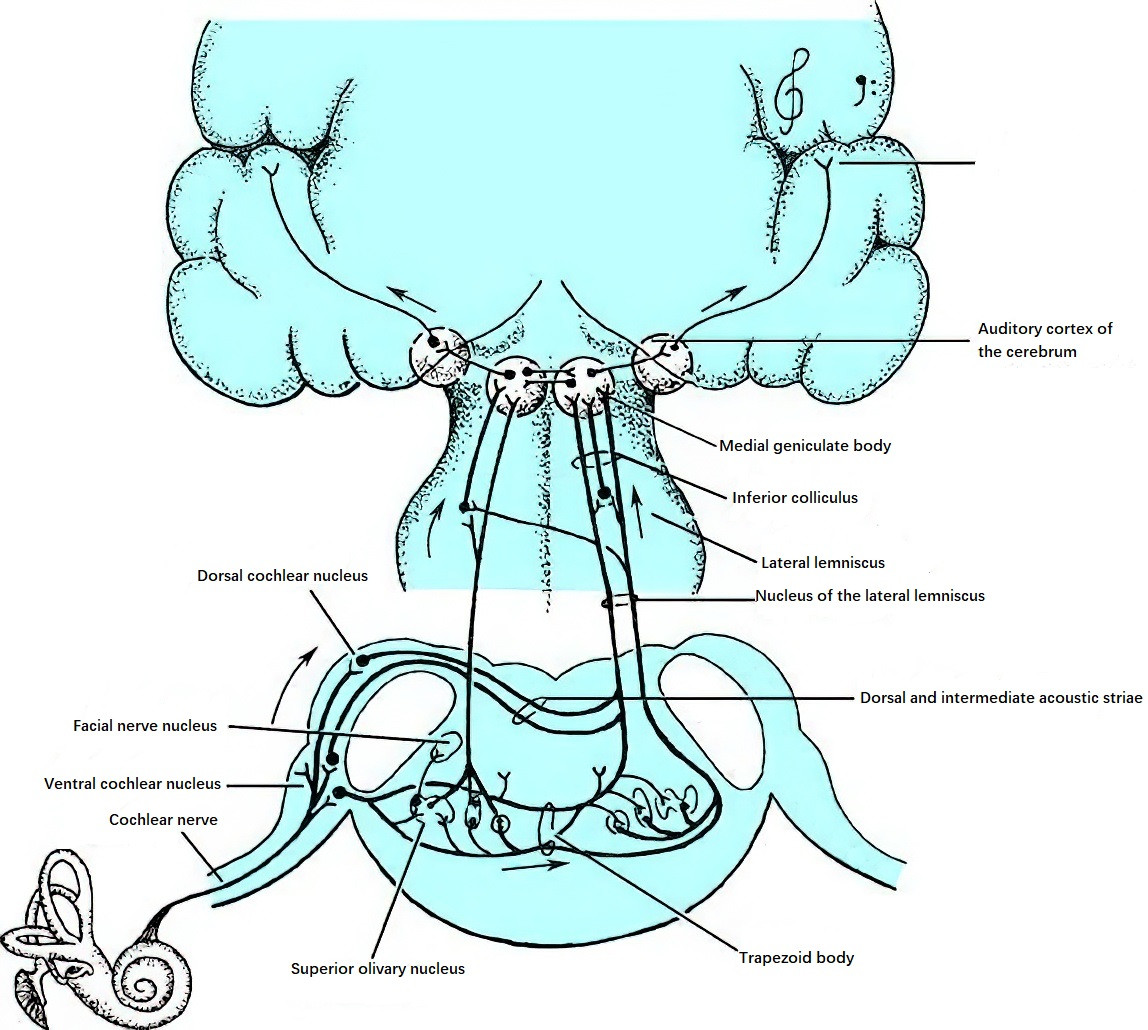
Figure 36 Conduction pathway of the cochlear nerve
If one cochlear nerve or its nuclei is damaged, complete hearing loss occurs on the same side. However, due to the crossing and uncrossing fibers in second- and third-order neurons, auditory impulses from one ear can reach the auditory cortex on both sides of the brain. Consequently, lesions in the lateral lemniscus or auditory cortex on one side do not result in significant bilateral hearing impairment.
Vestibular Nerve and Its Conduction Pathway
The first-order neurons of the vestibular nerve are located in the vestibular ganglia at the floor of the internal acoustic meatus. In the vestibular ganglia, the peripheral processes of bipolar neurons originating from the upper part of the ganglion innervate the cristae ampullares of the superior and lateral semicircular canals and the macula of the utricle. The peripheral processes of neurons from the lower part of the ganglia innervate the crista ampullaris of the posterior semicircular canal and the macula of the saccule. The central processes of these bipolar neurons form the vestibular nerve.
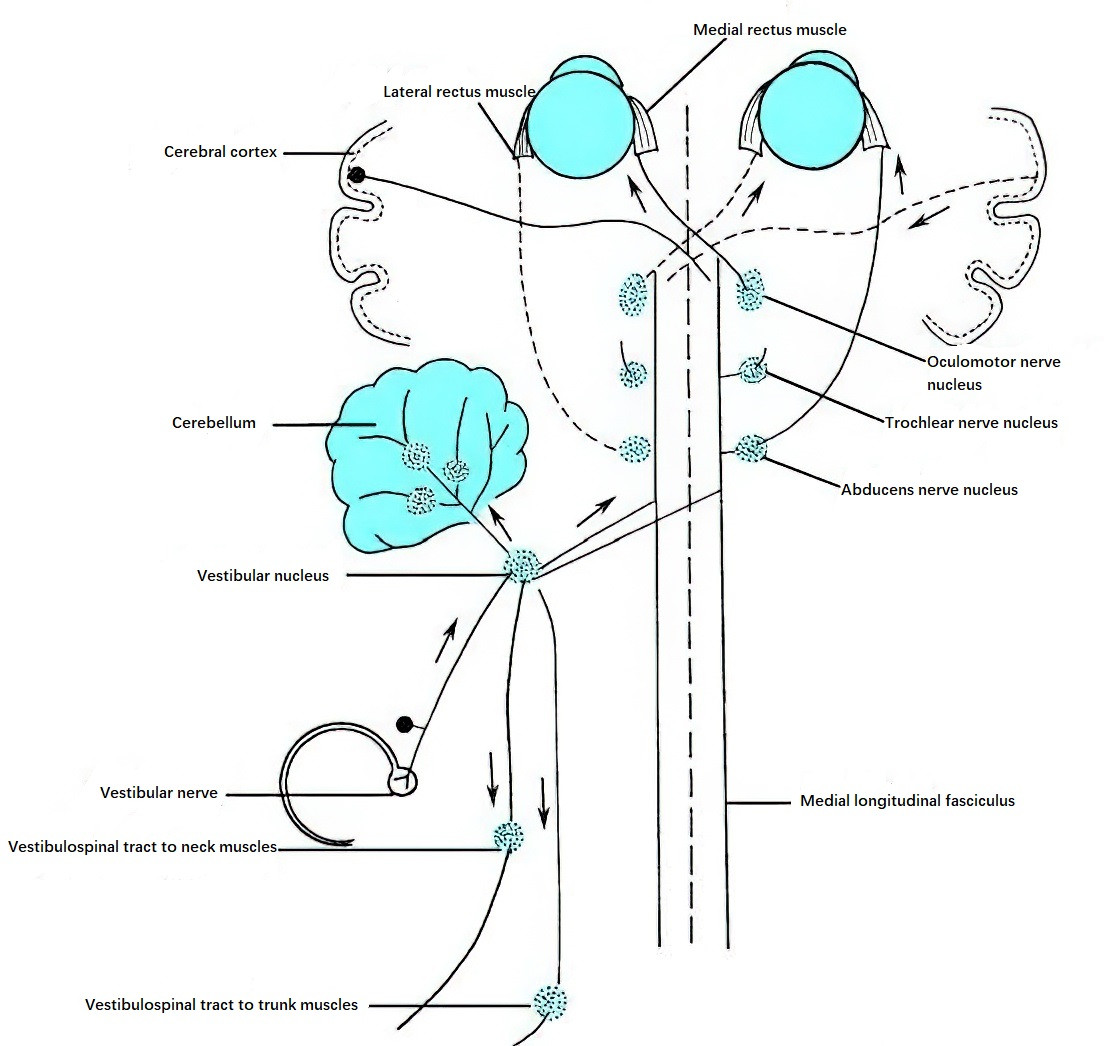
Figure 37 Conduction pathway of the vestibular nerve
The following describes the pathway of the vestibular nerve:
The vestibular nerve enters the brainstem at the pons-medulla junction above the cochlear nerve. Most of its fibers terminate in the vestibular nuclei, while a small portion bypasses them to reach the cerebellum via the juxtarestiform body. The vestibular nuclei, located in the pons and medulla, consist of four nuclei on each side: the superior vestibular nucleus, lateral vestibular nucleus, medial vestibular nucleus, and inferior vestibular nucleus.
- The superior nucleus receives afferent fibers from the cristae ampullares of the semicircular canals.
- The lateral and medial nuclei primarily receive afferent fibers from the macula of the utricle and the cristae ampullares.
- The inferior nucleus receives afferent fibers from all vestibular end organs.
The second-order neurons originating in the vestibular nuclei follow several conduction pathways:
- Vestibulospinal fibers originating from the vestibular nuclei descend via the medial longitudinal fasciculus and terminate in the spinal cord. Descending fibers from the lateral vestibular nucleus also enter the ipsilateral anterior funiculus of the spinal cord. All vestibulospinal fibers connect with anterior horn cells of the spinal cord, allowing impulses from the vestibular apparatus to induce reflex responses in the muscles of the neck, trunk, and limbs.
- Ascending fibers from the vestibular nuclei travel via the medial longitudinal fasciculus to reach the oculomotor, trochlear, and abducens nuclei on both sides. This connection enables changes in head position to induce reflexive movements of the eyes, which help maintain balance in ocular muscle tension.
- Fibers from the medial vestibular nucleus connect through the brainstem reticular formation to autonomic nervous system centers. This connection is responsible for autonomic responses such as pallor, sweating, nausea, and vomiting.
- Most afferent fibers from the inferior vestibular nucleus ascend via the juxtarestiform body to the cerebellum. Additionally, a small number of fibers from the medial vestibular nucleus project to the cerebellum.
The vestibular nerve’s pathway to the cerebral cortex has not been clearly established. The vestibular centers in the cerebral cortex are located in the temporal lobe, potentially near the auditory cortex. There may also be vestibular representation in the parietal lobe.