Ophthalmoscopy involves two commonly used types of ophthalmoscopes: the direct ophthalmoscope and the indirect ophthalmoscope.
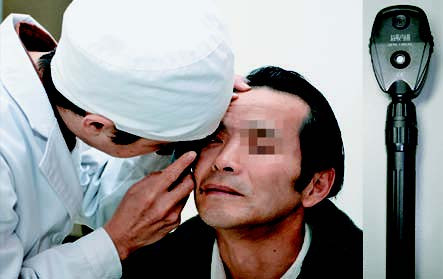
Figure 1 Direct ophthalmoscopy
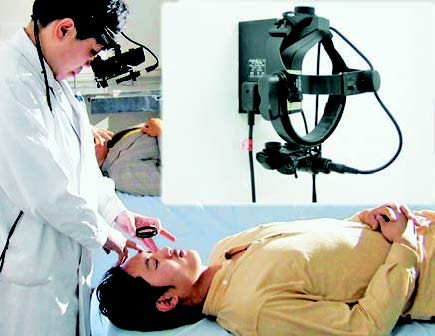
Figure 2 Indirect ophthalmoscopy
Direct Ophthalmoscopy
Direct ophthalmoscopy is the most frequently employed method for examining the fundus and holds significant value in preliminary evaluation and screening. The observed fundus image is upright and magnified approximately 16 times. It allows for the assessment of posterior segment structures and the estimation of the height of fundus lesions, as well as a rough evaluation of the fixation point. However, its limitations include a narrow field of view, lack of stereoscopic perspective due to monocular observation, and susceptibility to interference from media opacities. It is particularly suitable for non-ophthalmologists.
Examination Sequence and Details:
Retroillumination
This technique assesses the transparency of the eye's refractive media. The lens dial is set to +8 to +10D, and the examiner observes the eye from a distance of 10–20 cm. Under normal conditions, the pupil appears as a red reflex; if there is opacification in the refractive media, black shadows appear against the red reflex. If these shadows move in the same direction as ocular movement, the opacity is located anterior to the lens. If they move in the opposite direction, the opacity is posterior to the lens. If the shadow remains stationary, it is likely within the lens.
Fundus Examination
The lens dial is adjusted to "0," and the examiner approaches to 2 cm from the patient’s eye. The lens dial is further adjusted based on the refractive states of both the examiner and the patient until the fundus becomes clear. The patient is instructed to gaze straight ahead. The ophthalmoscope’s light source at an angle approximately 15° nasal to the pupil is used to examine the optic disc. The blood vessels are then followed to observe the periphery, and finally, the patient is asked to gaze directly at the ophthalmoscope's light to examine the macula.
Binocular Indirect Ophthalmoscopy
Binocular indirect ophthalmoscopy offers a lower magnification (3–4x) and produces an inverted image (both vertically and horizontally reversed) with a stereoscopic effect. The field of view is broader compared to direct ophthalmoscopy, allowing for a more comprehensive evaluation of the fundus. The device includes a fixed headband-mounted ophthalmoscope and a specially designed light source (6V, 15W bulb). A double aspheric lens is used as a condensing lens, with options such as +14D, +20D, or +28D, depending on the specific needs. Examination is performed after the patient undergoes full mydriasis. The examiner holds the lens approximately 7 cm in front of the patient’s eye to conduct the examination. When combined with a scleral depressor, the ora serrata and retinal breaks can be visualized, aiding in the identification of retinal tears. It is compatible with retinal treatments such as direct laser photocoagulation of retinal breaks and scleral buckling procedures.
Fundus Examination Recording Criteria
Key observations include the size, shape (e.g., congenital anomalies), and color (e.g., optic atrophy) of the optic disc; the disc's borders (e.g., swelling or inflammation) and pathologic cupping (e.g., increased cup-to-disc ratio, often seen in glaucoma). Retinal vessels should be assessed for their caliber, uniformity, color, arteriovenous ratio (normally 2:3), morphology, pulsatility, and the presence of arteriovenous nicking. The macular region and foveal light reflex should also be evaluated. Additionally, the retina should be examined for tears, degenerations, hemorrhages, exudates, or pigmentary changes, with descriptions of size, shape, and quantity. For significant abnormalities, retinal drawings can be created for documentation.
Slit-Lamp Fundus Lens Examination
The slit-lamp fundus lens (contactless lens) is a diagnostic tool for assessing the posterior segment of the eye, including the vitreous and retina. It produces stereoscopic inverted images with high illumination, deep depth of field, strong stereoscopic perception, and no direct corneal contact. Commonly used lenses include +60D, +78D, +90D, and Super Field NC. During the examination, the examiner holds the lens between the thumb and forefinger while using the middle finger to separate the patient’s eyelids. The lens is positioned in front of the patient’s eye, and the slit-lamp joystick is slowly pulled back until the fundus comes into focus through the light beam. For peripheral retinal examination, mydriasis is required, and the patient rotates their eyeball in the direction of interest while the light beam is repositioned as needed. This method provides an initial evaluation of the fundus, and if abnormalities are detected, further imaging studies may be performed. For patients with angle-closure glaucoma or shallow anterior chambers, care should be taken when performing mydriatic examinations.