Intraocular pressure (IOP) refers to the pressure exerted by the contents of the eyeball (including the lens, vitreous, uvea, retina, and intraocular fluids such as aqueous humor and blood) on the ocular walls. IOP measurement methods (tonometry) include palpation and tonometer-based methods.
Palpation Method
The palpation method is the simplest qualitative approach to estimate IOP and requires clinical experience. During the procedure, the patient is asked to look downward. The examiner gently alternates pressure on the patient's upper eyelids using the index fingers, assessing the tension of the globe and estimating its firmness, similar to checking for fluctuation. Beginners can practice by pressing the forehead, the tip of the nose, or the lips to develop a basic sense of high, medium, or low IOP. Documentation uses "Tn" to indicate normal IOP, "T+1" to "T+3" to indicate increasing levels of IOP elevation, and "T-1" to "T-3" to indicate decreasing levels of IOP.
Tonometry Methods
Conventional tonometers are generally divided into indentation tonometers and applanation tonometers.
- Indentation Tonometer: Applies a fixed weight to indent the cornea. The deeper the indentation under the same weight, the lower the IOP. This method is influenced by scleral rigidity. The Schiötz tonometer falls under this category.
- Applanation Tonometer: Flattens the corneal surface with a controlled force without indentation, minimizing the influence of scleral rigidity since the change in ocular volume is negligible.
Non-Contact Tonometer (NCT)
This tonometer uses a controlled burst of air to flatten the central cornea while projecting a directional light beam toward it. The reflected light is captured by a photocell. When the diameter of the flattened corneal area reaches 3.6 mm, the amount of reflected light received by the photocell is maximized, and the pressure of the air stream at this point corresponds to the IOP. Advantages of this method include a short examination time, no need for corneal contact, and elimination of cross-infection risks. It is well-suited for screening and patients allergic to topical anesthetics.
Goldmann Applanation Tonometer
Designed by Goldmann in 1948, this device is currently regarded as the international "gold standard" for IOP measurement. It is mounted on a slit-lamp biomicroscope and consists of a measuring prism, measuring apparatus, and a balancing arm. The measurement is performed with the patient in a seated position. When the corneal flattened area reaches 3.06 mm (an area of 7.354 mm2), the inner edges of two semicircles observed through the slit lamp coincide. The IOP is then recorded as the pressure scale reading. Central corneal thickness (CCT) can influence the measured IOP values.
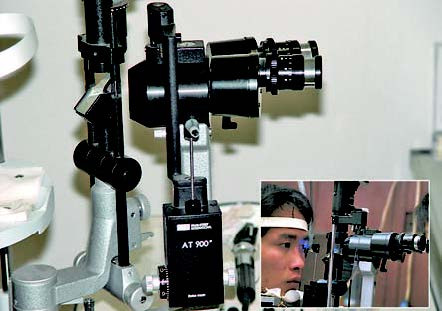
Figure 1 Goldmann applanation tonometer
Schiötz Tonometer
Invented by Schiötz in 1905, this cost-effective, durable, and portable device remains widely used, particularly for glaucoma screenings and emergency evaluations of acute angle-closure glaucoma. The instrument comprises a metal plunger, footplate, movable weight, scale, handle, and counterweight. The scale reading depends on the extent of corneal depression induced by the device, and measurements are influenced by scleral rigidity.
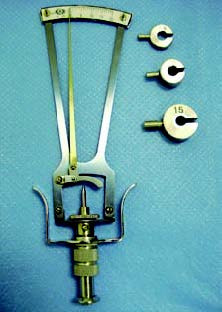
Figure 2 Schiötz tonometer
Other Tonometers
The Perkins tonometer is a handheld applanation tonometer that can be used without a slit-lamp biomicroscope. The patient can be in a seated or supine position.
The Tono-Pen tonometer is also a handheld, electronic applanation tonometer equipped with a microcomputer analysis system and an LCD display for results. Its portability makes it convenient for mobile use.