Slit-Lamp Biomicroscope and Its Applications
The slit-lamp biomicroscope is one of the most essential devices in ophthalmology. It consists of an adjustable slit-lamp illumination system and a binocular microscope, enabling in vivo, stereoscopic, and microscopic observation of the eye. By adjusting the focus and the width of the light source, it creates an optical cross-section, with magnifications ranging from 10x to 16x. This allows detailed, three-dimensional observation of the anterior segment structures as well as the topographic relationships of pathological changes. With the use of accessories such as the Goldmann three-mirror lens and fundus lens, it is possible to examine posterior segment structures like the retina. Gonioscopy facilitates the evaluation of the otherwise non-visible anterior chamber angle. Quantitative measurements of ocular biometric parameters can also be performed using tools like the anterior chamber depth gauge, Goldmann applanation tonometer, and endothelial microscopy. A digital camera can be attached to capture and document slit-lamp findings. Additionally, lasers and other treatment equipment can be integrated for managing ocular diseases. Certain ophthalmic procedures can also be conducted under direct visualization using the slit lamp.
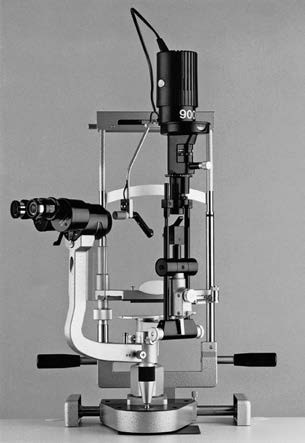
Figure 1 Slit-lamp biomicroscope
Operational Methods
The slit-lamp biomicroscope can be utilized through various illumination techniques, such as diffuse illumination, slit illumination, and retroillumination.
Diffuse Illumination
The light source is adjusted to produce a broad, diffuse beam, resembling a flashlight. This method provides an overall view and is useful for the general examination of the eyelids, conjunctiva, and sclera, as well as the comprehensive observation of the cornea, iris, and lens.
Slit Illumination
The light source is adjusted to produce a narrow slit of light that is projected onto specific tissues. This permits detailed observation of pathological changes and their three-dimensional relationships to surrounding structures.
Retroillumination
Performed typically after pharmacologic dilation, this method projects the light source onto tissues behind the area of interest. The reflected light is used to examine structural changes in anteriorly located pathological tissues.
Examination of Anterior Segment Structures
Cornea
Morphological Observation
Key observations include the size, curvature, transparency, and smoothness of the corneal surface, alongside any foreign bodies, neovascularization, opacities (e.g., scarring or inflammation), bulging, or conical protrusions (e.g., keratoconus). The presence of keratic precipitates (KP) on the posterior corneal surface should also be noted, as these are frequently associated with iridocyclitis and keratitis.
Fluorescein Staining
This test identifies epithelial and tissue defects. A sterile applicator dipped in 1%–2% fluorescein sodium is applied to the inferior conjunctival fornix, or a fluorescein strip is placed there. After 1–2 minutes, the yellow-green staining highlights areas of epithelial defects or ulceration.
Corneal Sensitivity Test
A simple method involves twisting a strand from a sterile cotton swab and using its tip to lightly touch the cornea from the side while observing for blinking reflexes. A lack of reflex or a significant difference in tactile force between the two eyes suggests reduced corneal sensitivity, often seen in herpes simplex keratitis or trigeminal nerve impairment.
Sclera
Observations focus on the presence of yellow discoloration, hyperemia, nodules, or tenderness.
Anterior Chamber
Depth Assessment
Central and peripheral anterior chamber depths, as well as symmetry between both eyes, are evaluated. The slit beam is narrowed and brightened, and illumination is directed at the peripheral limbal region. This produces three light bands: the epithelial surface of the cornea, the endothelial surface of the cornea, and the surface of the iris. The depth of the peripheral anterior chamber is assessed by estimating the distance between the endothelial surface and the iris compared to the corneal thickness (corneal epithelial to endothelial distance). For patients with significantly shallow anterior chambers, dilated examinations should be avoided to minimize the risk of angle closure and intraocular pressure elevation.
Aqueous Humor Observation
The clarity of the aqueous humor is surveyed for signs of Tyndall phenomenon (flare), cells, turbidity, hyphema, or hypopyon.
Iris
Observations include iris color, texture, and the presence of neovascularization, pigment loss, atrophy, or nodules. Other findings include anterior synechiae (adhesions to the cornea), posterior synechiae (adhesions to the lens), root detachments, defects, or tremors (indicating lens dislocation).
Pupil
This can be seen in the specific sections on pupil examination for detailed evaluation.
Lens
Lens observations include the presence, location, and extent of opacities, examination of lens color and morphology, and checks for subluxation or complete dislocation.