Cover Test
The cover test is one method used to disrupt fusion and assess the presence and type of strabismus. It is conducted at distances of 33 cm and 5 m, using an adjustable fixation target. This test can be further divided into the cover-uncover test and the alternate cover test. The alternate cover test detects the tendency for misalignment of the eyes, while the cover-uncover test distinguishes between manifest strabismus (heterotropia) and latent strabismus (heterophoria). The alternate cover test disrupts fusion more thoroughly, providing results that include both heterotropia and heterophoria components, whereas the cover-uncover test detects only heterotropia.
Measurement of the Strabismus Angle
Corneal Light Reflex Test (Hirschberg Test)
In this test, the patient fixes their gaze on a light source positioned at 33 cm. The degree of strabismus is estimated based on the position of the light reflex relative to the center of the pupil. A displacement of the reflex by 1 mm corresponds to an estimated deviation of 7.5° or 15 prism diopters. The primary advantages of this method include its simplicity and minimal patient cooperation requirements, but it lacks precision and does not account for the Kappa angle.
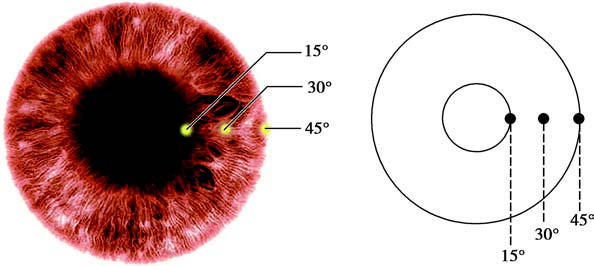
Figure 1 Corneal light reflex method for measuring strabismus angle
Prism Plus Cover Test
This is a more precise quantitative method for measuring the strabismus angle based on the optical principles of prisms. During the test, a prism is placed in front of the deviating eye with the prism's apex pointing toward the direction of the deviation, and the prism strength required to neutralize the deviation is recorded in prism diopters. This can be performed using either the cover-uncover method or the alternate cover method. However, this test is not suitable for patients with monocular blindness, eccentric fixation, or significant eye movement limitations.
Prism Corneal Reflex Test (Krimsky Test)
Although less precise than the prism plus cover test, this method is applicable for patients with monocular blindness, eccentric fixation, or other monocular viewing impairments, as well as for children who may not cooperate during testing. The patient gazes at a light source while a prism is placed in front of the deviating eye, with its apex pointing in the direction of the deviation. The prism strength is gradually increased until the corneal light reflex is centered in the pupil. The required prism diopter is the strabismus angle. In clinical practice, measurements are taken with and without glasses, for distances (near and far), and for each eye separately. These measurements provide valuable information for both diagnosis and treatment planning.
Synoptophore Test
Using special slides to assess simultaneous perception, this test yields the objective angle of strabismus. Quantitative measurements of strabismus angles in various diagnostic gaze positions help identify the affected muscle(s) in paralytic strabismus and assist in diagnosis and surgical planning.
Examination of Ocular Movement Function
Monocular Movement Test
One eye is occluded while the other tracks a moving target through all gaze directions. Any observed reduction in eye movement suggests weakened muscle strength or restrictive factors in that direction. Normal monocular movement is defined as follows: for adduction, the inner edge of the pupil reaches the line connecting the upper and lower lacrimal puncta; for abduction, the outer edge of the cornea reaches the lateral canthus; for elevation, the lower edge of the cornea reaches the line connecting the medial and lateral canthi; and for depression, the upper edge of the cornea reaches the same line.
Binocular Movement Test
Conjugate Movements
Based on Hering's Law of Equal Innervation, this test evaluates relative muscle function and identifies either underacting or overacting synergistic muscles. It helps distinguish between paralytic strabismus and comitant strabismus, identifies the affected muscle(s), and detects A- and V-pattern strabismus. The test is performed by observing both eyes as they gaze at diagnostic targets in different positions, noting changes in the strabismus angle. For example, if a patient with esotropia shows a significantly increased strabismus angle when gazing to the left during binocular movement testing, the muscles responsible for left gaze are implicated. If the left lateral rectus muscle is underacting, the angle of esotropia increases, indicating paralysis of the left lateral rectus.
Disconjugate Movements
Disconjugate eye movements include convergence and divergence, with convergence function being the primary focus in clinical practice. Convergence is a highly voluntary movement with involuntary components, playing an important role in extraocular muscle function testing. The near point of convergence (NPC) is assessed by having the patient focus on a target that elicits accommodation, gradually bringing it closer to the nasal bridge until diplopia or deviation of one eye from the convergent position occurs. The point at which convergence breaks is termed the NPC, with a normal range of 5 to 10 cm. The NPC moves farther away with increasing age.
Doll's Head Maneuver
This test differentiates between true and false restrictions of abduction. The head of a child is suddenly turned toward the side opposite the "restricted" abduction, and the ability of the eye to abduct to a normal position is assessed. If abduction is achieved, it indicates a lack of genuine abduction restriction. If abduction is not achieved, it suggests the presence of movement restriction.
Forced Duction Test
This test distinguishes whether ocular movement restriction is due to neuromuscular paralysis or mechanical constraints. It includes the Active Force Generation Test and the Passive Forced Duction Test.
- Active Force Generation Test: Performed under local anesthesia while the patient is awake. After topical anesthetic is applied, an eyelid speculum is used, and forceps hold the limbus at the site corresponding to the muscle being examined. The contraction force of the tested muscle is assessed. A difference in muscle contraction force suggests neuromuscular paralysis.
- Passive Forced Duction Test: Typically performed under local anesthesia, but general anesthesia yields more reliable results. Once adequate anesthesia is achieved, forceps hold the conjunctiva at the limbus at the 3 o'clock and 9 o'clock positions. The eyeball is rotated in all directions, with particular attention to the restricted direction. The absence of resistance excludes mechanical restrictions, whereas resistance indicates their presence. If performed under local anesthesia, the patient must gaze in the same direction as the manual pulling to avoid false positive results.
Parks’ Three-Step Test
This test identifies the primary paretic muscle in vertical strabismus, distinguishing between the superior oblique and the contralateral superior rectus. It involves a stepwise process of elimination:
- Step 1: Determining which eye exhibits hypertropia. If the right eye is hypertropic, it suggests paresis in one of its depressors (inferior rectus or superior oblique) or in one of the left eye’s elevators (superior rectus or inferior oblique).
- Step 2: Evaluating whether the vertical deviation increases in right or left gaze. If the deviation is greater in left gaze, it points toward the involvement of the right superior oblique or the left superior rectus.
- Step 3: Performing the Bielschowsky Head Tilt Test by tilting the head toward the hypertropic eye (right side in this case). An increase in vertical deviation (a positive test) indicates paretic involvement of the right superior oblique muscle. Conversely, a negative test suggests primary involvement of the left superior rectus muscle.
Binocular Function Tests Related to Strabismus
Suppression Test
This is one of the simplest methods for identifying monocular suppression in patients with obvious strabismus but no reports of diplopia. Other tests include the Worth Four-Dot Test and the Bagolini Striated Lens Test.
Fusion Reserves Test
This test, also known as the Red Filter and Prism Test, assesses the potential for fusion in strabismus patients. A red filter is placed in front of one eye, and both eyes focus on a light source. The patient perceives one red and one white light. A prism is then placed in front of one eye until the red and white images fuse into one pink image, indicating latent fusion potential. The prism strength is gradually increased until the patient again perceives one red and one white light. The prism strength required to transition from two lights to fusion and back to two lights represents the fusion reserves of the patient.

Figure 2 Fusion reserves test
Stereopsis Test
This test includes random dot stereograms and non-random dot stereograms. Patients wear polarized glasses or red-green glasses to view special images with horizontal disparity. Stereopsis is then quantitatively evaluated. The normal range is 40 to 60 arcseconds. Commonly used tests include the Titmus Stereo Test and the TNO Stereo Test.
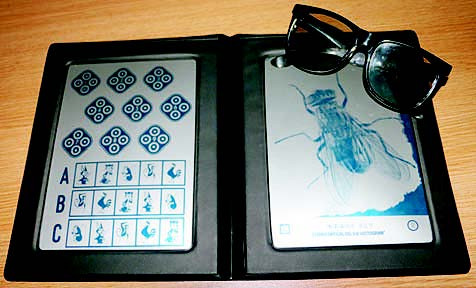
Figure 3 Titmus stereo test
Diplopia Testing
During this test, the patient's head is kept in a straight position without rotation. A red filter is placed in front of one eye, and the patient focuses on a light source at a distance of 1 meter. Diplopia is identified if both a red and a white light are seen. If only a single pink light is visible, it indicates no diplopia. Each diagnostic gaze position is assessed within approximately 20° of the central field of vision.
Steps to Analyze Diplopia:
- Determining the type of diplopia—whether it is horizontal, vertical, crossed, or uncrossed.
- Identifying the gaze direction in which diplopia is most pronounced.
- Recognizing that the peripheral image belongs to the paretic eye. Horizontal diplopia is determined by the relative position of peripheral images horizontally, while vertical diplopia is determined in the tertiary gaze position where peripheral images deviate vertically.
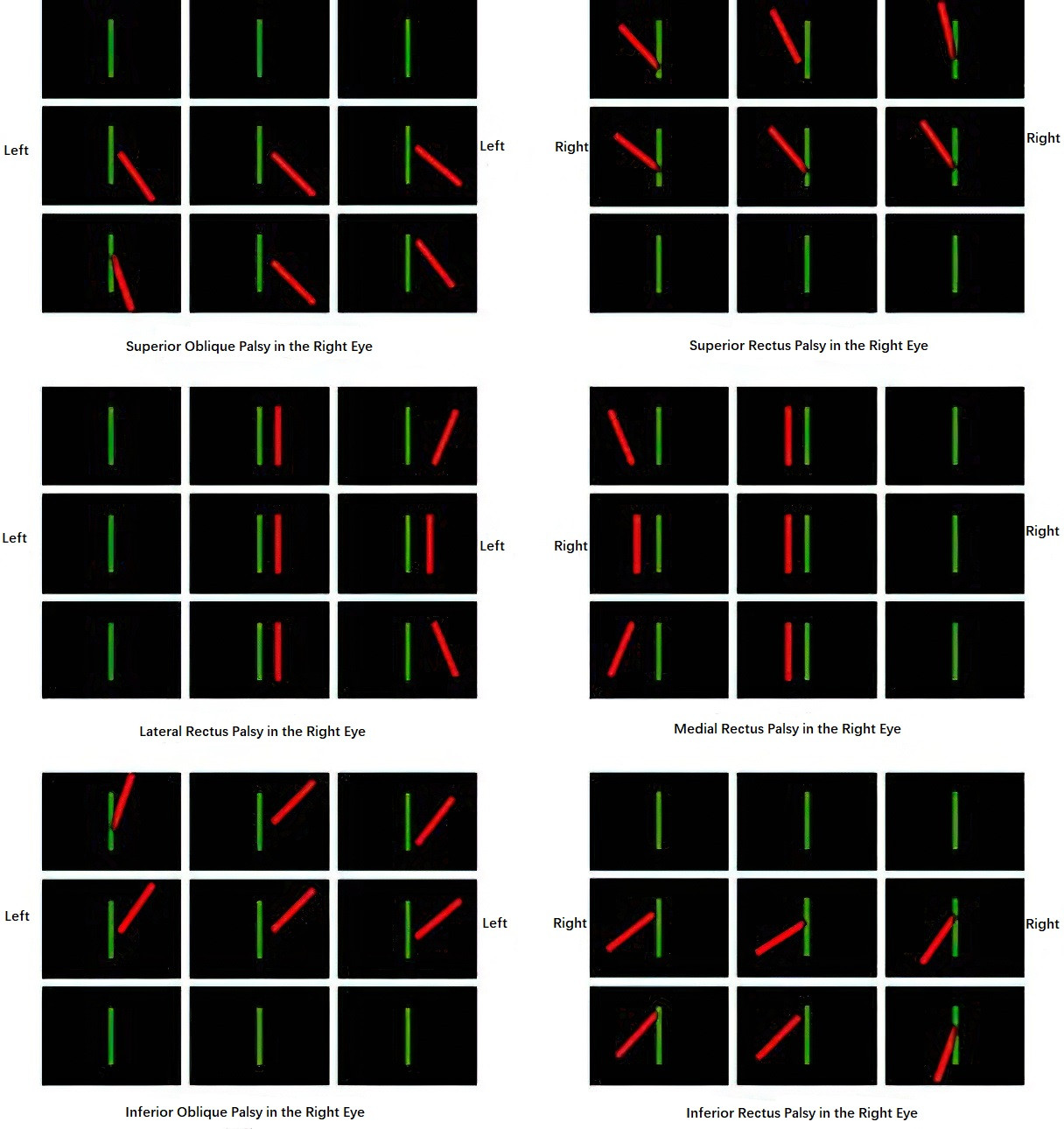
Figure 4 Diplopia patterns in extraocular muscle palsies of the right eye