The ocular adnexa includes the eyelids, conjunctiva, lacrimal system, extraocular muscles, and the orbit. Details on lacrimal system examinations are discussed in Chapter 5 on lacrimal disorders, and extraocular muscle examinations are covered in the section on strabismus evaluation.
Eyelids
Observations include the presence or absence of redness, swelling, bruising, emphysema, scars, or masses. The occurrence of entropion or ectropion, the symmetry of the palpebral fissures on both sides, as well as the normality of upper eyelid elevation and palpebral fissure closure are assessed. The arrangement and direction of eyelashes are evaluated for irregularities, discoloration, or loss, along with the presence of congestion, scales, crusts, or ulcers at their roots. Additionally, the lid margin is examined for congestion, thickening, secretions, and abnormalities in the meibomian gland orifices.
Conjunctiva
The eyelids are everted to inspect the palpebral conjunctiva and fornix conjunctiva. Observations include its color, transparency, and smoothness, and detection of conditions such as congestion, edema, papillary hypertrophy, follicular proliferation, scarring, ulcers, symblepharon, foreign bodies, or retained secretions. To assess the bulbar conjunctiva, the examiner separates the upper and lower eyelids using the thumb and forefinger while the patient rotates their eyes in the upward, downward, left, and right directions. Observations include the presence of vascular congestion, with a focus on distinguishing ciliary injection (located around the corneal limbus) from conjunctival injection (located in the peripheral conjunctiva), as well as the presence of vesicles, hemorrhage, foreign bodies, pigmentation, or neoplasms.
Position and Movements of the Eyeball
The corneal position in relation to the center of the palpebral fissure while gazing straight ahead is noted, along with the symmetry of vertical positions and the presence of nystagmus or strabismus. The size of the eyeballs is assessed for abnormalities, including proptosis or enophthalmos.
A simple method to assess proptosis involves seating the patient with the head slightly reclined. The examiner stands behind the patient and gently elevates both upper eyelids using the index fingers, observing the symmetry of the eyeball protrusion from a posterior-superior angle to an anterior-inferior perspective. For precise measurements of anteroposterior displacement of the eyeballs and the degree of proptosis, the Hertel exophthalmometer is used. This involves placing the exophthalmometer’s arms against the lateral orbital rims of both eyes while the patient gazes straight ahead. The projection of the corneal apex is then read off the ruler in millimeters. The normal average for adult proptosis is 12–14 mm, with a difference of no more than 2 mm between the two eyes.
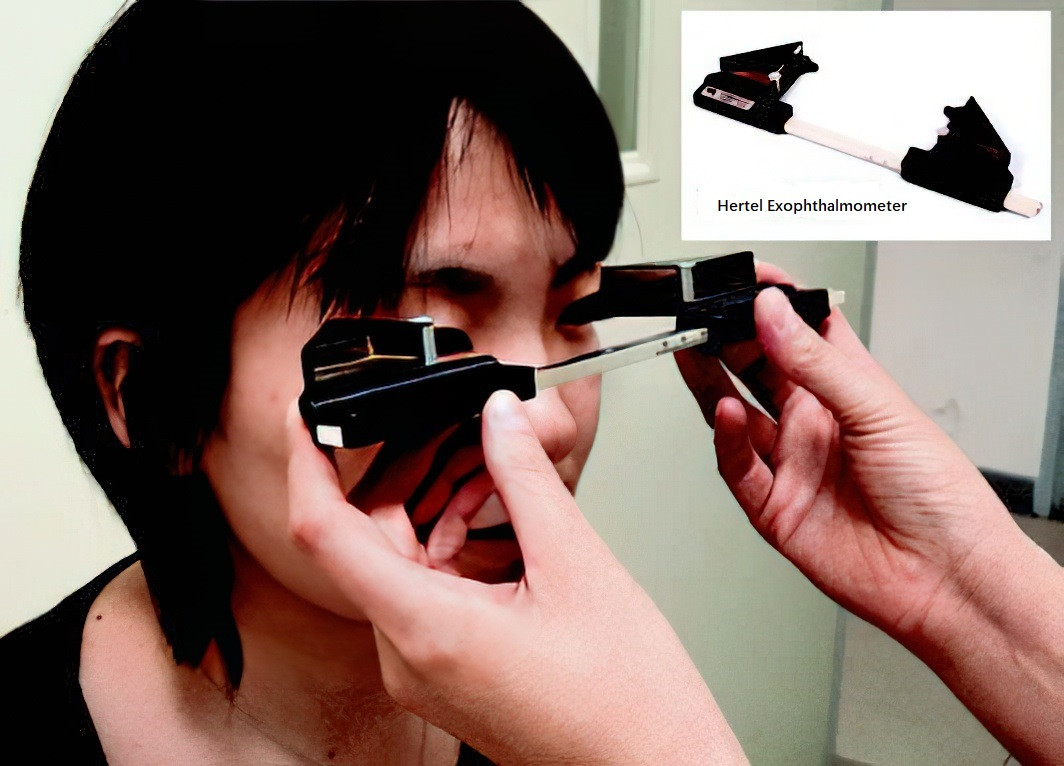
Figure 1 Measurement of proptosis
To evaluate ocular motility, the patient is asked to move their eyes in eight directions: left, right, up, down, up-right, down-right, up-left, and down-left, to determine whether there is any restriction in movement (refer to the section on strabismus evaluation).
Orbital Examination
The symmetry of both orbits is evaluated. Palpation of the orbital rims is performed to detect abnormalities such as defects, tenderness, or masses.