The visual field refers to the spatial area perceived when the eyes are fixated straight ahead. In contrast to central visual acuity, it reflects peripheral visual sensitivity. The central visual field encompasses the area within 30° of the fixation point, while the peripheral visual field extends beyond 30°. The visual field has a significant impact on both work and daily life.
Normal Visual Field Range
Using a white target with a diameter of 3 mm to assess the peripheral visual field, the normal values are: superior 55°, inferior 70°, nasal 60°, and temporal 90°. When using blue, red, or green targets, the peripheral visual field decreases by about 10° for each color. The center of the physiological blind spot is located 15.5° to the temporal side of the fixation point and 1.5° below the horizontal midline. Its vertical diameter is 7.5° ± 2°, and its horizontal diameter is 5.5° ± 2°. The size and position of the physiological blind spot vary slightly from person to person. Narrow areas of reduced sensitivity can also be observed along the upper and lower edges of the blind spot, corresponding to the projections of large blood vessels near the optic disc.
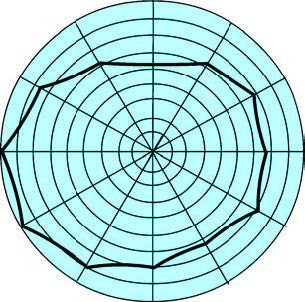
Figure 1 Normal visual field range (Left eye)
Characteristic changes in the visual field occur in many eye and neurological diseases, making visual field examination important for their diagnosis.
Design and Methods of Visual Field Testing
Development Stages of Perimetry
The development of perimeters has progressed through three stages: the earliest manual perimeters, the Goldmann manual hemispherical kinetic perimeter, and the currently used computer-controlled static quantitative perimeter.
Types of Visual Field Testing
Visual field testing is divided into kinetic perimetry and static perimetry.
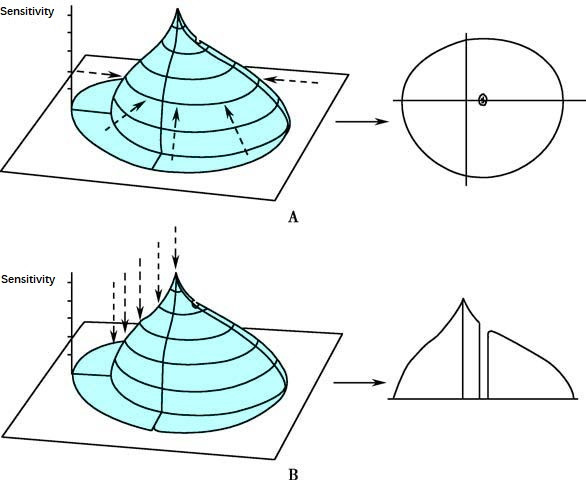
Figure 2 Visual field testing
A. Kinetic Visual Field
B. Static Visual Field
Kinetic Perimetry
This is the conventional method of visual field testing, such as using a planar perimeter. Targets of different sizes are moved from various directions in the periphery toward the center. The points where the examinee first perceives the targets are recorded, forming isopters (lines of equal sensitivity) for different targets. These form a contour map of the "island of vision." The advantage of kinetic perimetry lies in its speed and its suitability for evaluating the peripheral visual field. However, it has a lower detection rate for small scotomas or relative paracentral defects.
Static Perimetry
This is a computerized automated method of visual field testing. At predetermined points on the screen, the brightness of the target is incrementally increased from dim to bright. The brightness at which the examinee first perceives the target represents the retinal light sensitivity or the light threshold at that point. Static quantitative perimetry provides faster and standardized results.
Factors Influencing Visual Field Testing
As a psychophysical test, the visual field examination reflects the subjective perception of the individual being tested. Three main factors influence the outcomes:
- The Examinee: Influential factors include mental state (e.g., alertness, attention, visual fatigue, and retinal light threshold variability) and physiological or pathological factors (e.g., pupil size, media opacities, and refractive errors).
- The Equipment: Variations arise from differences between kinetic and static perimetry, planar versus hemispherical screens, single-point versus multi-point stimulation, as well as differences in background illumination and targets.
- The Operator: Variability in methods and experience among examiners can lead to human error.
Common Methods of Visual Field Testing
Confrontation Method
This is the most basic technique for visual field testing. The method involves comparing the visual field of the examiner (assumed to be normal) with that of the examinee to determine if abnormalities are present. The process involves seating the examiner and the examinee facing each other at the same eye level, approximately 1 meter apart. During the test of the right eye, the examinee's right eye fixates on the examiner's left eye while their other eye is covered. The reverse applies when testing the left eye. A finger or a small object is used as the target and is positioned midway between the two individuals. It is moved toward the center from the superior, inferior, nasal, and temporal directions. If the examinee can perceive the target simultaneously with the examiner in all directions, the visual field is considered normal. The advantage of this method is that it does not require specialized equipment. However, it lacks precision and does not provide objective records.
Arc Perimeter
This is a simple dynamic perimetry device for evaluating the peripheral visual field. It consists of a 180° arc with a radius of 33 cm. The knob for moving the target and the recording pen operate synchronously, making it easy to use.
Campimeter
This device uses dynamic perimetry to evaluate the visual field within 30°. It features a black screen positioned at a distance of 1 or 2 meters, with a central fixation point. Horizontal lines on either side span 15°–20°, and physiological blind spots are marked using black upright circles. Visual targets of different sizes are used to plot isopters corresponding to respective sensitivity thresholds.
Goldmann Perimeter
The Goldmann projected hemispherical perimeter is the most representative among hemispherical perimeters. It integrates multiple features and can perform both kinetic and static visual field testing, allowing for an understanding of the overall visual field. This perimeter has provided standardized parameters for stimulus in the development of subsequent perimeters.
Automated Perimeter
Computer-controlled static quantitative perimeters, such as the Octopus and Humphrey perimeters, are representative devices. They include specialized testing programs tailored for conditions like glaucoma, macular diseases, and neurological disorders.
The examination methods of automated perimeters can be classified into three main types:
- Suprathreshold Testing: This is a qualitative assessment of the visual field, which categorizes results as normal, relative scotoma, or absolute scotoma. This method is fast but has lower reliability, making it primarily suitable for screening ocular diseases.
- Threshold Testing: This is the most precise quantitative visual field test. Its drawback is that it takes about 15 minutes per eye, which can lead to fatigue in the examinee.
- Fast Threshold Testing: Programs like TOP (Tendency Oriented Perimetry) utilize intelligent trend analysis to reduce the number of testing steps, requiring only 5 minutes per eye.
Key points for interpreting automated perimeter results:
The variability of normal values is small in the central part of the visual field but larger in the peripheral parts. Scotomas within 20° from the center are more likely to be pathological, while those located in the upper or lower regions at 25°–30° are often due to eyelid obstruction. Variability in the 30°–60° range of the visual field is high, requiring caution when diagnosing visual field defects in this region.
Changes in threshold values at a single isolated point are usually insignificant. Diagnostic relevance is only found when several adjacent points show changes in threshold values.
An abnormal result during an initial automated visual field examination might be due to the examinee's lack of familiarity with the testing procedure. Reexamination of the visual field is recommended to confirm defects, as any scotomas must be reproducible to establish a diagnosis.
Some perimeters include defect probability maps, which can assist in the diagnostic process.
Amsler Grid
This test is used to detect early macular abnormalities, monitor their progression, or identify central and paracentral scotomas.