The eyeball is located in the front part of the orbital cavity, where it is connected to the orbital walls via orbital fascia and ligaments. It is cushioned by orbital fat pads and is protected anteriorly by the eyelids and posteriorly by the orbital bones. At birth, the axial length (the anteroposterior diameter) of the eyeball is approximately 16 mm, reaching about 23 mm by the age of three and eventually 24 mm in adulthood. Its vertical diameter is slightly shorter than its horizontal diameter. While looking straight ahead, the average protrusion of the eyeball from the lateral orbital rim is about 12–14 mm. Variations may occur based on factors such as ethnicity, skull development, and refractive status, but the difference in prominence between the two eyes generally does not exceed 2 mm.
The eyeball consists of the eyeball wall and its internal contents.
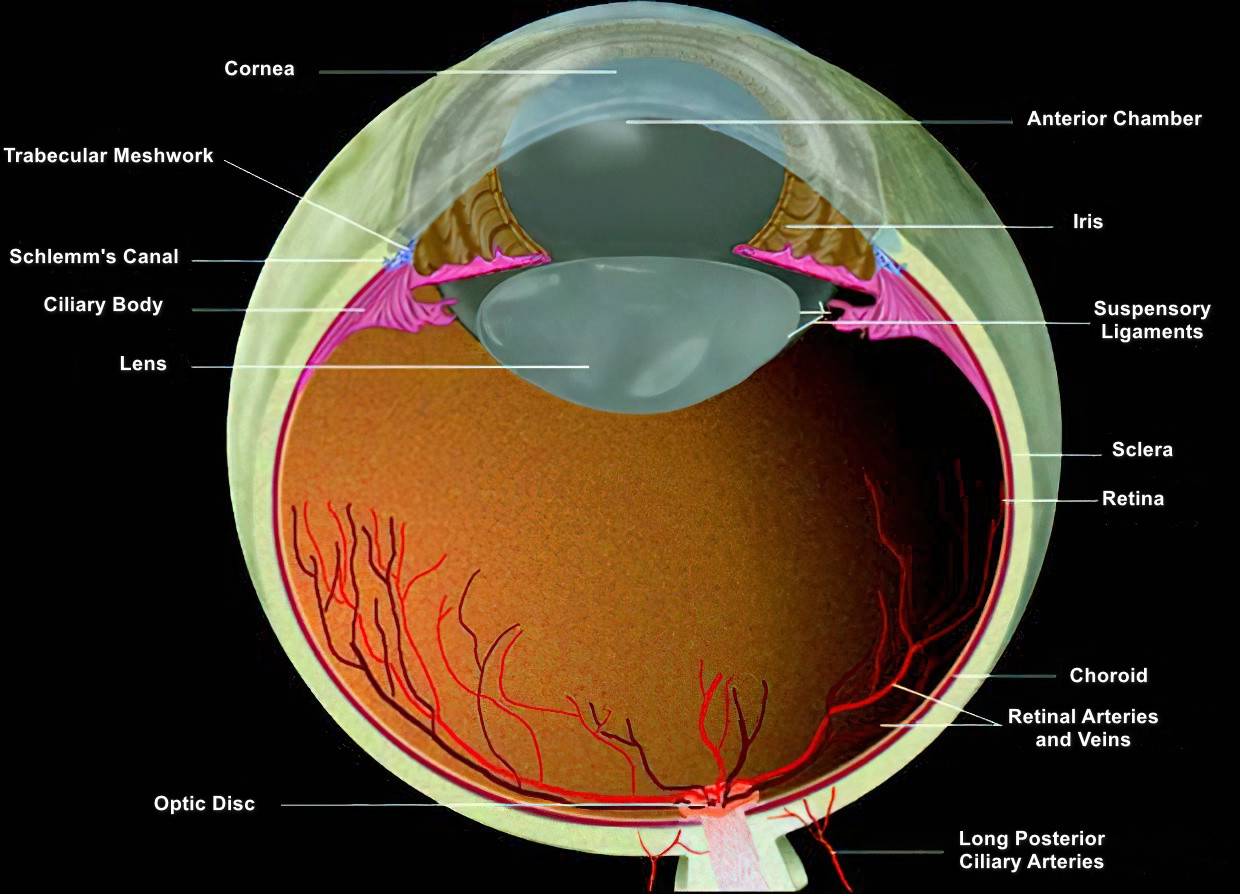
Figure 1 Schematic cross-section of the eye
Eyeball Wall
The anterior portion of the eyeball wall is the cornea, a single-layered fibrous membrane, whereas the posterior portion is composed of three layers: the outer fibrous layer, the middle uveal tract, and the inner retinal layer.
Outer Layer
The outer layer is mostly composed of collagenous fiber tissue and consists of the transparent anterior cornea and the opaque posterior sclera, together forming the complete outer wall of the eyeball. This layer serves to protect intraocular structures and maintain the shape of the eyeball.
Cornea
The cornea is situated at the anterior part of the eyeball, slightly convex to the front. It is a transparent, horizontally oval structure and a vital part of the refractive system. Its horizontal diameter measures 11.5–12 mm, while its vertical diameter is 10.5–11 mm. The radius of curvature of its anterior surface is approximately 7.8 mm, while that of the posterior surface is about 6.8 mm. The central corneal thickness is about 0.5 mm, increasing to about 1.0 mm toward the periphery.
Histologically, the cornea can be divided into five layers from anterior to posterior:
- Epithelium Layer: Approximately 35 μm thick, this layer is composed of 5–6 layers of non-keratinized squamous epithelial cells arranged in an exceptionally orderly manner. It is easily separable from the Bowman membrane beneath it.
- Bowman Membrane: A homogeneous, acellular, transparent membrane approximately 12 μm thick.
- Stroma Layer: This is the thickest layer of the cornea, about 500 μm thick and constituting 90% of its total thickness. It is composed of nearly 200 layers of regularly arranged collagen fiber lamellae, interspersed with keratocytes and a small number of migrating cells, as well as mucopolysaccharides and glycoproteins.
- Descemet Membrane: A robust, homogeneous, transparent membrane about 10–12 μm thick.
- Endothelium Layer: Comprising a monolayer of flattened hexagonal cells about 5 μm thick, the apical surface of these cells faces the anterior chamber, while the basal surface adjoins the Descemet membrane.
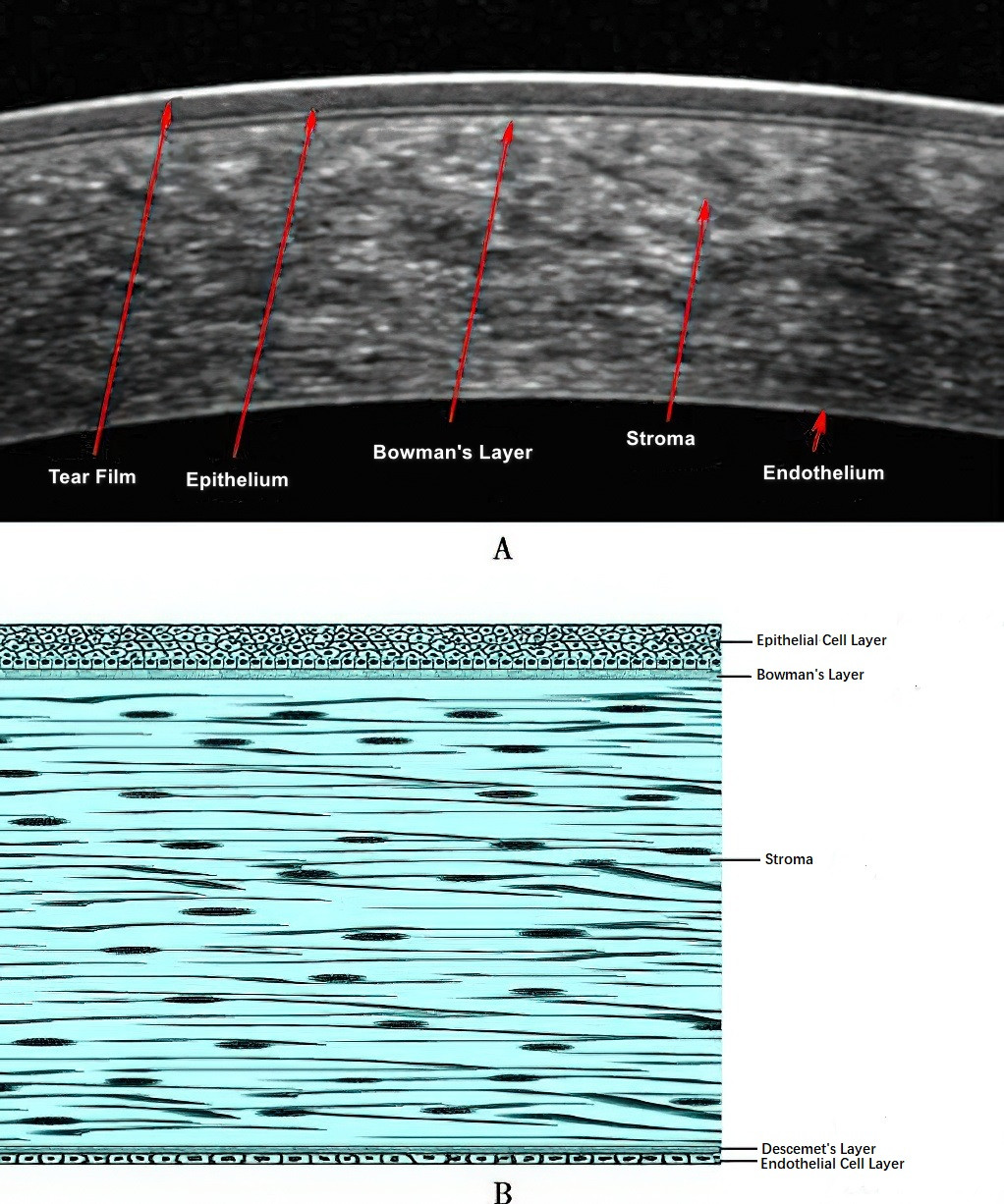
Figure 2 OCT section of the cornea and schematic diagram of corneal histology
Sclera
The sclera is a tough, dense, white structure mainly composed of tightly interwoven collagen fibers. It is connected anteriorly to the cornea and posteriorly to the optic nerve. At the posterior segment, the sclera divides into an outer two-thirds that transitions into the optic nerve sheath and an inner one-third that takes on a sieve-like structure called the scleral lamina cribrosa, which allows optic nerve fibers to exit the eyeball. The thickness of the sclera varies; it is thinnest at the insertion points of the rectus muscles (about 0.3 mm) and thickest near the optic nerve and the corneoscleral junction (about 1.0 mm).
Histologically, the sclera is divided into three layers: the episclera, the scleral stroma, and the lamina fusca. The episclera consists of dense vascularized connective tissue, and the region behind the limbus contains an episcleral vascular plexus (aqueous veins). Additionally, the scleral canals house arteries, veins, and nerves that pass through the entire scleral thickness. The remaining areas of the sclera are almost avascular.
The sclera is encased externally by the Tenon capsule (bulbar fascia), which is further covered anteriorly by the conjunctiva. At the limbus, the cornea, sclera, conjunctiva, and fascia merge and attach to one another.
Limbus
The limbus, also known as the corneoscleral junction, is the transitional zone between the cornea and the sclera. Because the transparent cornea transitions into the opaque sclera, there is no sharp demarcation line on the surface or histologically. Anatomically, the limbus is the location of the anterior chamber angle and the aqueous outflow system. Clinically, it serves as the landmark for many intraocular surgical incisions. Histologically, it contains the corneal stem cells, highlighting its importance. The anterior boundary of the limbus is generally considered the plane connecting the terminations of the Bowman and Descemet membranes, while its posterior boundary lies at the scleral spur or the root of the iris, perpendicular to the ocular surface. The limbus varies in width from 1.5 to 2.5 mm across different quadrants. Visually, the limbus contains an approximately 1 mm-wide translucent anterior zone (from the edge of Bowman to the edge of Descemet membrane) and a posterior white scleral zone (from the edge of Descemet membrane to the scleral spur or iris root, encompassing structures such as the trabecular meshwork and Schlemm's canal).
Angle of the Anterior Chamber
The angle of the anterior chamber is located at the junction of the peripheral cornea and the root of the iris. This region forms the primary pathway for aqueous humor outflow from the eye. Within the inner surface of the limbus lies a depression called the scleral sulcus, which houses a trabecular meshwork and Schlemm's canal. The inner posterior portion of the scleral sulcus features a prominent structure known as the scleral spur. In this way, the angle of the anterior chamber comprises an anterior-external wall formed by the limbus (extending from Schwalbe’s line—corresponding to the termination of the posterior limiting lamina of the cornea—to the scleral spur) and a posterior-internal wall formed by the anterior portion of the ciliary body and the root of the iris. Structures identifiable within the angle of the anterior chamber, from anterior to posterior, include Schwalbe's line, the trabecular meshwork and Schlemm's canal, the scleral spur, the ciliary band (representing the face of the ciliary body), and the root of the iris.
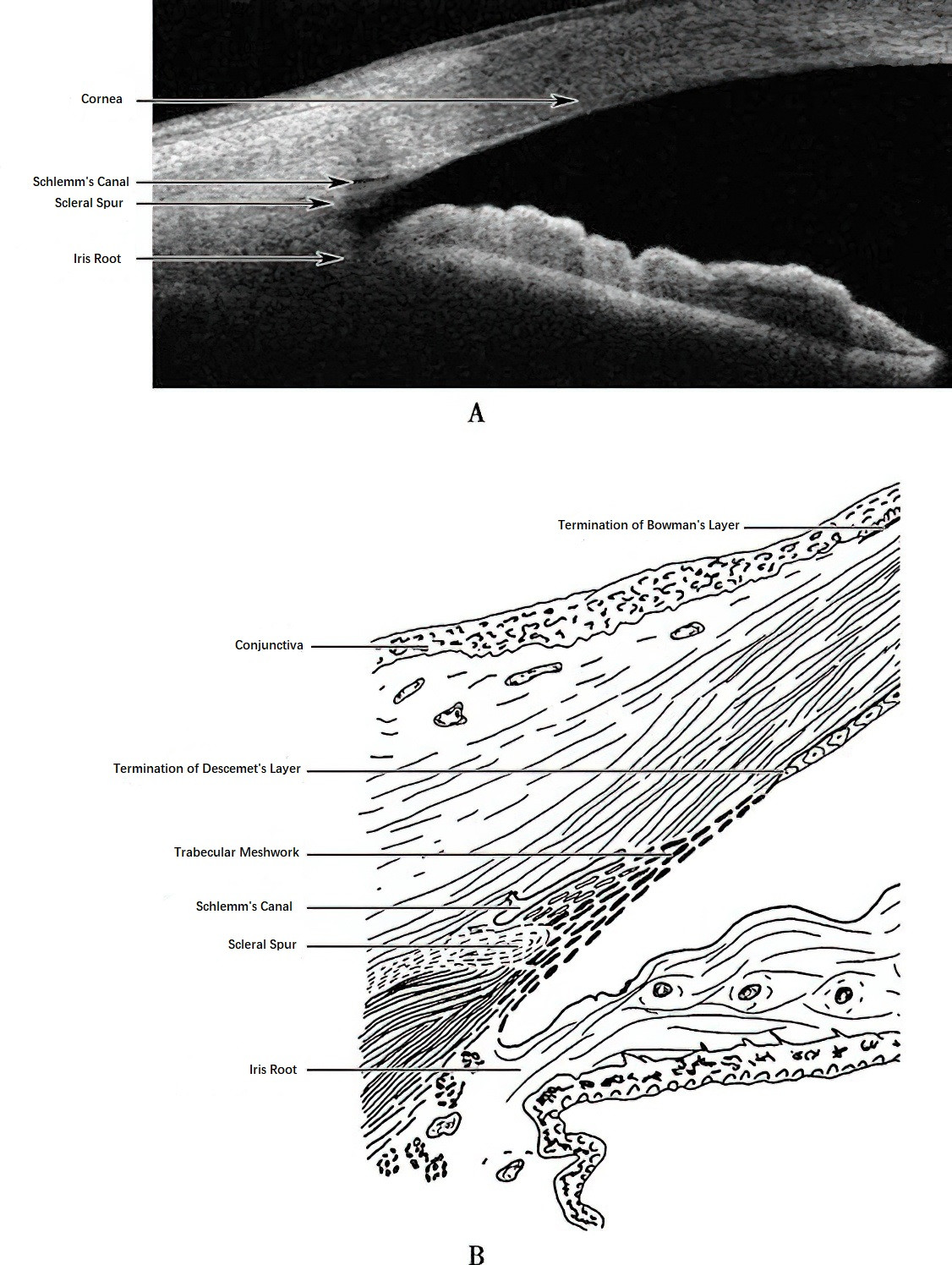
Figure 3 Schematic diagram of the anterior chamber angle
The trabecular meshwork consists of flat, interconnected, lamellar, or beam-like structures forming a network. Each trabecular beam is composed of a core of collagen fibers encased in endothelial cells. The trabecular meshwork involved in filtering aqueous humor is divided into three parts: the uveal trabecular meshwork (facing the anterior chamber), the corneoscleral trabecular meshwork, and the juxtacanalicular trabecular meshwork (adjacent to Schlemm’s canal). The juxtacanalicular portion is the primary site of resistance to aqueous humor outflow. Schlemm’s canal, a circumferential drainage channel surrounding the angle of the anterior chamber, is formed by interconnected flattened spaces. Its inner wall, composed of a single layer of endothelial cells, is adjacent to the trabecular meshwork, while its outer wall connects to 25–35 aqueous collector channels that communicate with intrascleral veins (aqueous veins).
Middle Layer
The middle layer, also known as the uvea or vascular layer, is a pigmented membrane rich in blood vessels and melanin. It is composed of three interconnected parts, arranged from anterior to posterior: the iris, the ciliary body, and the choroid. The uvea is firmly attached to the sclera at three points: the scleral spur, the exit of Schlemm’s canal, and around the optic nerve. In other areas, it is separated from the sclera by a potential space called the suprachoroidal space.
Iris
The iris is a circular, disk-like tissue that extends from the ciliary body and lies in front of the lens, dividing the anterior section of the eye into the anterior chamber and the posterior chamber. The iris is suspended within the aqueous humor, and its surface is characterized by radially arranged folds and crypts called iris texture and crypts. At its center lies a circular opening, the pupil, with a diameter of approximately 2.5–4 mm. Around 1.5 mm from the pupil margin, a ring-like ridge called the collarette divides the iris into two regions: the pupillary zone and the ciliary zone.
The iris is connected peripherally to the ciliary body at its base, the iris root, which is a thin region prone to detachment from the ciliary body when subjected to blunt trauma. The location of the iris in front of the lens can result in the phenomenon of iridodonesis (iris tremor) when the lens is dislocated or surgically removed, as the iris loses its structural support.
The iris is composed of an anterior stroma and a posterior pigmented epithelium. The stroma consists of a loose framework of connective tissue intermingled with blood vessels, nerves, and pigment cells. Within the stroma lies the sphincter pupillae muscle (a circular smooth muscle near the pupillary margin), innervated by parasympathetic nerves and responsible for pupillary constriction. The density of pigment in the pigment cells of the stroma determines the color of the iris; densely pigmented iris tissues are brown, while less pigmented ones appear blue.
The posterior pigmented epithelium is composed of two layers. Both layers are densely packed with melanin, giving the posterior surface of the iris a deep black appearance. Muscle fibers from the anterior layer differentiate into the dilator pupillae muscle (a smooth muscle), which is innervated by sympathetic nerves and functions to dilate the pupil. The posterior epithelial layer forms a narrow, serrated black fringe at the pupillary margin, a structure referred to as the pupillary ruff.
Ciliary Body
The ciliary body is a 6–7 mm wide circular structure located between the root of the iris and the choroid. In sagittal view, it is roughly triangular, with the scleral spur marking its base of attachment.
The anterior third of the ciliary body is thickened and referred to as the ciliary crown. This 2 mm-wide region is vascularized and characterized on its inner surface by 70–80 longitudinally arranged radial ridges known as ciliary processes. The posterior two-thirds of the ciliary body are thinner and flatter, forming the pars plana. The pars plana is an important surgical entry site for vitreoretinal procedures. At its posterior boundary, the pars plana connects to the choroid and the peripheral retina at the ora serrata, a serrated, transitional zone marking the posterior border of the ciliary body.
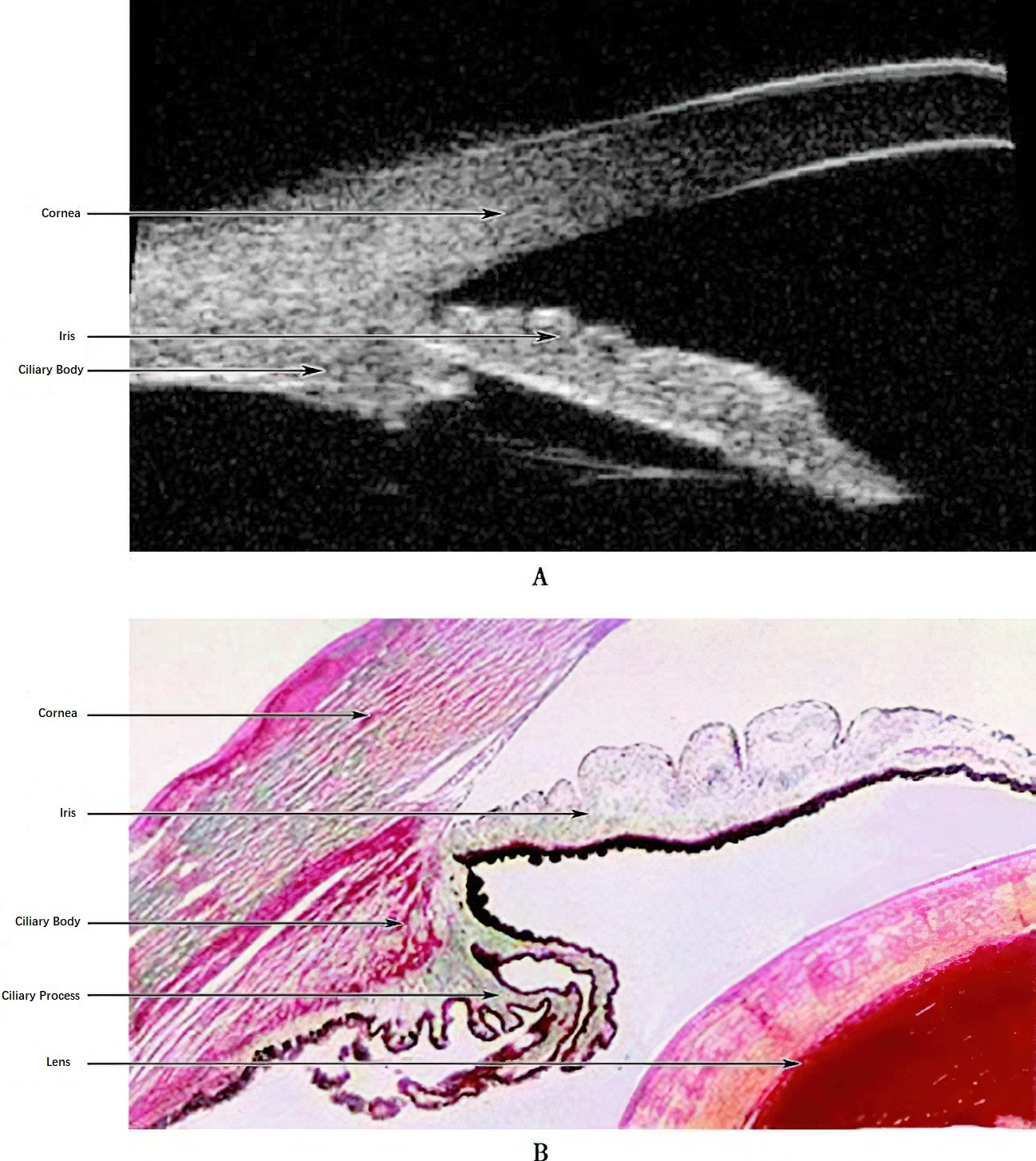
Figure 4 Schematic diagram of the ciliary body
The ciliary body consists mainly of the ciliary muscle and ciliary epithelium. The ciliary muscle is composed of three groups of smooth muscle fibers: longitudinal, radial, and circular. The longitudinal fibers, extending anteriorly, reach the trabecular meshwork. The muscle is innervated by parasympathetic nerves. The ciliary epithelium consists of two layers: an outer pigmented epithelial layer and an inner non-pigmented epithelial layer.
Choroid
The choroid forms the posterior portion of the uvea. It begins at the ora serrata and ends around the optic disk. It is situated between the sclera and the retina and is rich in blood vessels and melanocytes, forming a lobular structure. The average thickness of the choroid is around 0.25 mm. It contains three vascular layers: the outermost large vessel layer, the intermediate medium vessel layer, and the innermost choriocapillaris layer. The choroid is connected to the retinal pigment epithelium by Bruch’s membrane.
The posterior ciliary arteries, short posterior ciliary arteries, and ciliary nerves all pass through the suprachoroidal space. At the sclerocorneal junction, blood vessels and nerves traverse the scleral canal, attaching the choroid tightly to the sclera.
Inner Layer
The inner layer of the eye is the retina, a transparent membrane located on the inner surface of the choroid.
The retina features a central avascular depression known anatomically as the fovea, which is referred to clinically as the macula lutea due to its high concentration of yellow pigment. At the center of the fovea lies a small depression, anatomically termed the foveola and clinically known as the fovea centralis. This is the region of the retina with the highest visual acuity. Retinal pigment epithelial (RPE) cells in the macular region contain a higher concentration of pigment, giving this area a darker appearance under an ophthalmoscope. A reflection of light, known as the foveal reflex, can often be observed at the foveal center.
The optic disc, also referred to as the optic papilla, is an anatomical concept closely associated with the optic nerve. It is located approximately 3 mm nasal to the macula and has a size of about 1.5 mm by 1.75 mm. The optic disc is a well-defined, vertically oval, orange-red structure where retinal ganglion cell axons converge to exit the eyeball and form the optic nerve, transmitting visual information to the central nervous system. At the center of the optic disc is a small depressed region called the optic cup. The central retinal artery and vein pass through the optic disc and branch out across the retina.
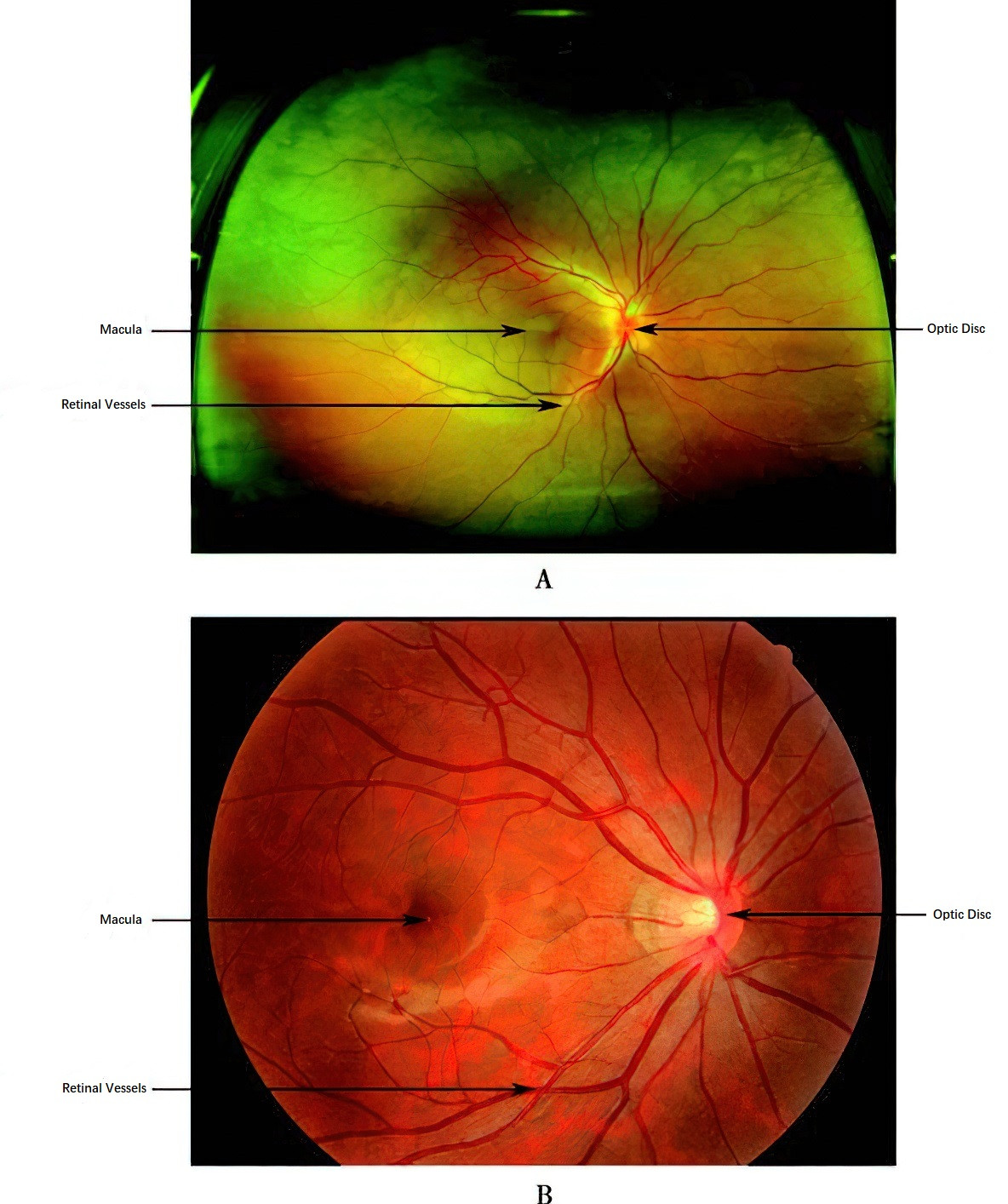
Figure 5 Fundus images
The retina develops embryologically from the optic cup, which arises from the neuroectoderm. The outer layer of the optic cup forms the single-layer retinal pigment epithelium (RPE), while the inner layer differentiates into the neural retina. A potential space exists between these two layers, and retinal detachment occurs clinically at this junction.
The retinal pigment epithelium (RPE) consists of a single layer of hexagonal cells arranged in an orderly pattern. It is thicker in the macular region and becomes thinner toward the periphery. The RPE is polarized, with its basal side tightly adherent to Bruch's membrane of the choroid, while the apical side features numerous microvilli that encapsulate the outer segments of photoreceptor cells within a mucopolysaccharide matrix.
The neural retina consists of several layers, arranged from outer to inner as follows:
- Photoreceptor Layer: Composed of the outer and inner segments of rod and cone cells, which are the primary light-sensing cells.
- External Limiting Membrane: A thin, net-like membrane formed at the junctions of photoreceptor and Müller cells.
- Outer Nuclear Layer: Contains the nuclei of photoreceptor cells.
- Outer Plexiform Layer: A loose, reticular layer where the axons of rod and cone cells synapse with the dendrites of bipolar cells and the projections of horizontal cells.
- Inner Nuclear Layer: Predominantly composed of the cell bodies of bipolar cells, horizontal cells, amacrine cells, and Müller cells.
- Inner Plexiform Layer: The synaptic region where bipolar cells, amacrine cells, and ganglion cells make mutual connections.
- Ganglion Cell Layer: Contains the cell bodies of ganglion cells.
- Nerve Fiber Layer: Composed of the axons of ganglion cells, which form the optic nerve fibers.
- Internal Limiting Membrane: A thin membrane separating the retina from the vitreous body, formed by the basement membrane of Müller cells.
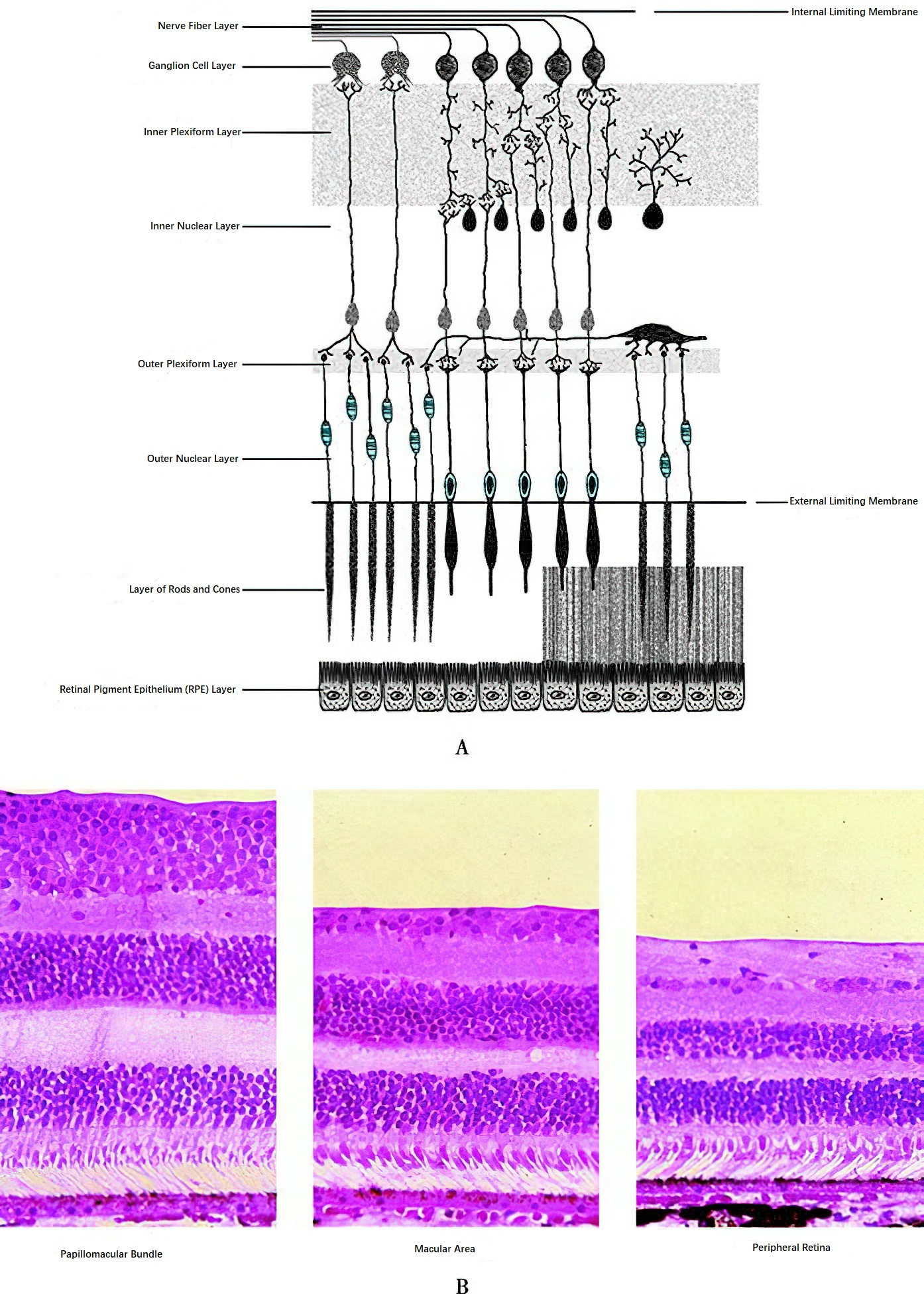
Figure 6 Diagram of retinal structure
The photoreceptor cells, which include rods and cones, have five structural components: the outer segment, connecting cilium, inner segment, cell body, and synaptic terminal. Each outer segment consists of approximately 700 stacked flattened disc membranes. Rod cell outer segments are cylindrical, while cone cell outer segments are conical in shape. These membrane discs are continuously shed and renewed. Neural signals from the photoreceptors are transmitted to ganglion cells through bipolar cells, which serve as intermediaries.
The axons of ganglion cells converge at the optic disc to form the optic nerve. The fibers in the macular region follow an arcuate pattern, grouped above and below a horizontal raphe, as they converge on the temporal side of the optic disc. These fibers collectively form the papillomacular bundle. Similarly, temporal peripheral fibers are divided into superior and inferior portions and enter the optic disc above and below the papillomacular bundle. In contrast, fibers from the superior and inferior nasal regions of the retina travel directly to the optic disc.
Contents of the Eyeball
The contents of the eyeball include aqueous humor, the lens, and the vitreous body. These three transparent substances, along with the cornea, constitute the refractive media of the eye and form the pathway through which light enters the eye and reaches the retina.
Aqueous Humor
Aqueous humor is a transparent fluid within the eye that fills the anterior and posterior chambers. The anterior chamber refers to the intraocular space between the posterior surface of the cornea and the anterior surface of the iris and the lens in the pupillary zone. Its volume is approximately 0.2 ml, and its central depth is about 2.5–3 mm, becoming shallower toward the periphery. The posterior chamber is a ring-shaped space located behind the iris, bound by the inner side of the ciliary body, the anterior surface of the lens, and the zonules that suspend the lens. Its volume is about 0.06 ml. Aqueous humor constitutes approximately 4% of the total volume of the eye and is involved in dynamic circulation.
Lens
The lens is a biconvex, transparent structure located behind the pupil and iris and anterior to the vitreous body. It is held in position by the zonules of the lens, which connect it to the ciliary body. The radius of curvature of the anterior surface of the lens is about 10 mm, while that of the posterior surface is about 6 mm. The junction between the anterior and posterior surfaces is termed the equator, while the tips of the anterior and posterior surfaces are referred to as the anterior pole and posterior pole, respectively. The diameter of the lens is approximately 9 mm, and its thickness increases slowly with age, with a central thickness typically around 4 mm.
The lens consists of the lens capsule and the lens fibers. The capsule is an elastic, homogeneous basement membrane. The anterior capsule is about twice as thick as the posterior capsule, being thinnest at the posterior pole (around 4 μm) and thickest at the equator (up to 23 μm). Beneath the anterior capsule and the equatorial capsule lies a layer of cuboidal epithelial cells, which is absent beneath the posterior capsule. The lens fibers are formed by the elongation of epithelial cells at the equator, which extend toward the anterior and posterior poles. Lens fibers are continuously generated throughout life, pushing older fibers inward, where they harden to form the lens nucleus. The newer, outer fibers constitute the lens cortex. The lens is highly elastic, but with advancing age, the lens nucleus gradually becomes more condensed and larger, leading to a decrease in elasticity.
Vitreous Body
The vitreous body is a gel-like, transparent substance that fills the vitreous cavity, accounting for four-fifths of the total volume of the eyeball at approximately 4.5 ml. A concave depression, called the vitreous fossa, is located on the anterior surface of the vitreous body, accommodating the lens. The rest of the vitreous body is in contact with the retina and the ciliary body, forming closely adhered connections at certain areas, particularly at the optic disc margin, around the macular fovea, and along the vitreous base (an area 2 mm anterior to and 4 mm posterior to the ora serrata). These adhesions are particularly tight. The anterior surface of the vitreous body is connected to the posterior capsule of the lens by a circular adhesion, which is tighter in young individuals but loosens with age.
Within the central part of the vitreous body, a region with lower optical density, known as the Cloquet's canal, may be observed. It extends from the posterior pole of the lens to the anterior portion of the optic disc and represents the remnant of the primary vitreous from the embryonic stage, where it housed the hyaloid vasculature during development.