Infections of the urinary and male reproductive systems refer to inflammation caused by pathogenic microorganisms invading and proliferating within these systems. Most pathogens involved are Gram-negative bacilli. Due to the anatomical proximity and connection between the urinary and reproductive systems, as well as the urethral opening being exposed to external environments, infections often occur simultaneously or are transmitted between the two systems. Urinary system infections, also referred to as urinary tract infections (UTIs), can be categorized based on their location: upper urinary tract infections involve the kidneys, renal pelvis, and ureters, while lower urinary tract infections affect the bladder and urethra. Upper urinary tract infections often coexist with lower urinary tract infections, although the latter can occur independently. UTIs are highly prevalent, ranking second only to respiratory infections among infectious diseases. They can occur across different sexes and age groups, tend to recur, and are more common in females. Clinical presentations vary significantly.
Pathogens
Pathogenic microorganisms are a primary factor in the development of infections. Most pathogens originate from facultative anaerobic bacteria in the gastrointestinal tract. The most common pathogen is Escherichia coli (E. coli), accounting for 85% of community-acquired infections and 50% of hospital-acquired infections. Other pathogens include Escherichia coli var. communior, Klebsiella spp., Proteus spp., Staphylococcus spp., Enterococcus spp., Alcaligenes spp., and Pseudomonas aeruginosa. Additionally, fungi, Mycobacterium tuberculosis, Neisseria gonorrhoeae, Chlamydia spp., Ureaplasma spp., Trichomonas spp., anaerobic bacteria, protozoa, and viruses can also cause infections. Urogenital system infections caused by Mycobacterium tuberculosis are classified as specific infections.
Pathogenesis
Urinary tract infections result from the interaction between pathogens and the host. The occurrence of these infections is partially due to bacterial virulence, inoculation quantity, and an incomplete host defense mechanism. These factors influence the establishment of bacterial colonization and the extent of urinary tract damage. In healthy individuals, the skin and mucosa around the external urethral meatus are colonized by normal microbiota, such as Lactobacillus spp., Streptococcus spp., Staphylococcus spp., and Corynebacterium spp.. Under normal conditions, these commensals inhibit pathogenic bacteria when their numbers and virulence remain below a certain threshold. Additionally, the acidity, high osmolarity, urea content, and organic acids in healthy urine are unfavorable for bacterial growth, while bladder emptying helps expel bacteria. These factors provide a defense mechanism against infection in the urinary tract.
Bacterial virulence also plays a critical role. E. coli, for example, possesses an acidic polysaccharide antigen on its surface, known as the K antigen. Strains expressing specific K antigens exhibit high virulence and are more likely to cause urinary tract infections. The ability of pathogens to adhere to urinary tract epithelial cells is another important factor in the pathogenesis of UTIs. The mucus secreted by urinary tract epithelial cells contains mucoprotein, mucopolysaccharides, glycoproteins, and other components that reduce bacterial adhesion and regulate adherence strength. Mucus forms a protective barrier, and when pathogens bind to and damage this barrier, they can adhere to the epithelial cell surface and cause infection.
Factors Predisposing to Infection
When pathological changes occur in the urinary or male reproductive systems, the body's defense mechanisms are compromised, allowing pathogens to invade and cause infection. Four primary categories of predisposing factors are outlined below:
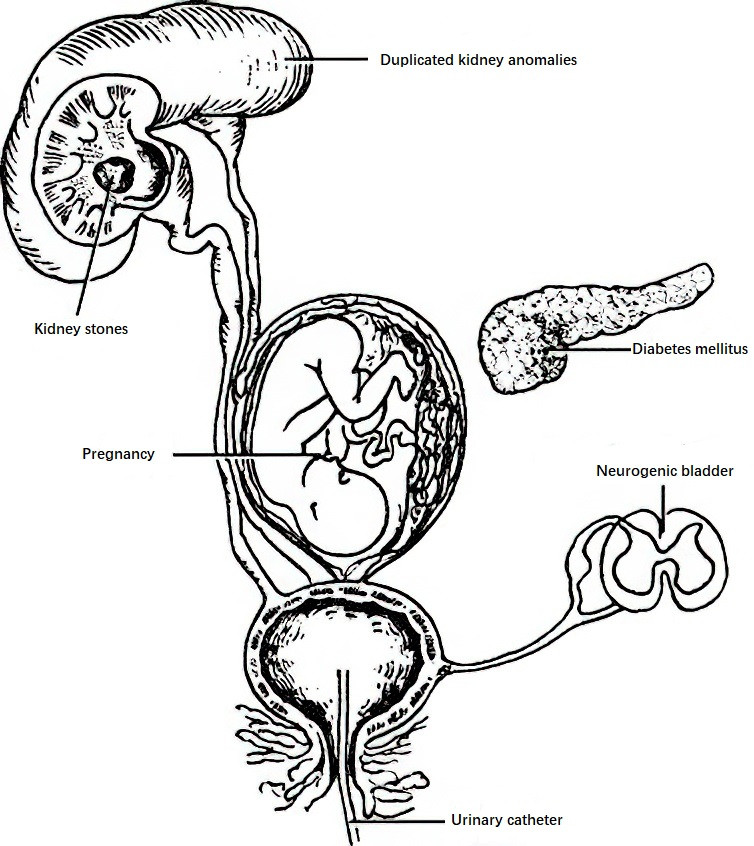
Figure 1 Factors contributing to infections of the urinary and male reproductive systems—reduction in host immunity
Reduced Host Immune Capacity
Conditions such as diabetes mellitus, pregnancy, anemia, chronic liver disease, chronic kidney disease, malnutrition, tumors, congenital immune deficiencies, or long-term use of immunosuppressive therapy impair the body's ability to combat infections.
Obstruction-Related Factors
Congenital anomalies of the urogenital system, stones, tumors, strictures, benign prostatic hyperplasia, or neurogenic bladder can obstruct urine flow. These conditions lead to urine retention and weaken the epithelial defense mechanisms of the urinary and reproductive tracts against bacterial invasion.
Iatrogenic Factors
Medical interventions such as the placement of urinary catheters, ureteral stents, or drainage tubes, as well as procedures like urethral dilation, prostate biopsies, or cystoscopy, can introduce pathogens due to mucosal injury or a lack of adherence to aseptic techniques. This can provoke or spread infections.
Other Factors
The shorter and wider urethra in females increases susceptibility to ascending infections, particularly during menstruation, menopause, or sexual activity. Pregnancy-associated endocrine or mechanical changes can lead to relaxation and dilation of the ureteral orifice, delaying urine flow and predisposing to ascending infections. Malformations of the urethral meatus or nearby infections, such as paraurethral gland inflammation or vaginitis, also serve as predisposing factors.
Routes of Infection
There are four primary routes of infection, with ascending infection being the most common.
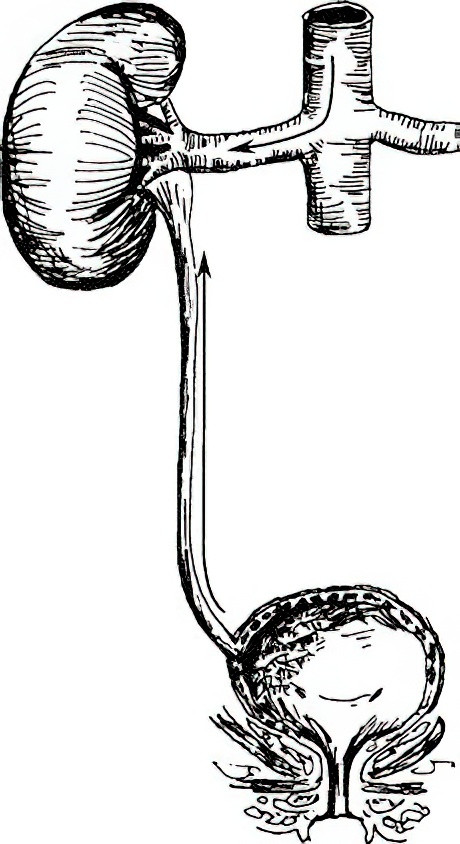
Figure 2 Ascending infection in the urinary system (Arrows within blood vessels indicate hematogenous spread)
Ascending Infection
Pathogenic bacteria invade the bladder via the urethra and can further spread through the ureter to the kidney. Approximately 50% of lower urinary tract infections lead to upper urinary tract infections. This occurs because bladder infections can cause mucosal edema, which may impair the anti-reflux mechanism at the vesicoureteral junction, resulting in urine reflux and allowing pathogens to ascend directly to the kidneys. Ascending infections are more likely when bacteria possess strong adhesive properties or when normal ureteral peristalsis is disrupted. Such infections frequently occur in women during their honeymoon period, pregnancy, infancy, or in patients with urinary obstructions. Escherichia coli is the most common pathogen associated with this route.
Hematogenous Spread
Although less common, bacteria can enter the urinary and genital systems via the bloodstream when the immune system is compromised or certain conditions facilitate the spread. Infections such as skin abscesses, boils, tonsillitis, otitis media, or dental caries may allow bacteria to disseminate hematogenously, often leading to renal cortical infections. Staphylococcus aureus is a common causative pathogen, and Mycobacterium tuberculosis can also be involved.
Lymphatic Spread
Pathogens can infiltrate the urinary and genital systems through lymphatic channels from nearby infected organs, such as during severe intestinal infections or retroperitoneal abscesses.
Direct Extension
This refers to the spread of infection from adjacent organs, as seen with infections like appendiceal abscesses or purulent pelvic inflammatory disease. Direct contamination may also occur due to external factors, such as infections introduced via nephrostomy drainage tubes or foreign objects.
Diagnosis
The classic symptoms of frequent urination, urgency, and dysuria are hallmark clinical manifestations of urinary tract infections, particularly during the acute phase. Diagnosis is generally straightforward but requires a comprehensive medical history to identify possible triggering factors.
The diagnosis of urinary tract infections relies on urinalysis, with confirmation through urine culture. Correct collection of urine specimens is a crucial step to minimize contamination, which may affect diagnostic accuracy.
Urine Specimen Collection
Urine specimens can be collected by three primary methods:
- Mid-stream urine collection, typically used in most cases.
- Catheterization, commonly employed for female patients.
- Suprapubic bladder aspiration, which is most reliable and suited for neonates and patients with spinal cord injuries.
Urine cultures are commonly performed using clean mid-stream or catheterized specimens. Collected specimens should be processed within two hours to prevent contamination or overgrowth of non-pathogenic bacteria.
Microscopic Urinalysis
Urine samples should ideally be examined promptly. A simple approach involves staining a drop of fresh urine with methylene blue for microscopic observation. Using this method, Gram-negative bacilli, Gram-positive cocci, fungi, and acid-fast bacilli can be visualized. Further tests such as bacterial, fungal cultures, and antibiotic sensitivity tests should be performed on a portion of the sample. Urinary sediment examination for white blood cells is also routine; more than five leukocytes per high-power field indicates pyuria, suggesting a urinary tract infection. Sterile pyuria may raise suspicion of conditions like tuberculosis.
Bacterial Culture and Colony Counting
Bacterial culture and colony counts are critical for diagnosing urinary tract infections. A colony count greater than 105/mL is generally indicative of infection, while counts below 104/mL suggest contamination. Colony counts between 104 and 105/mL are considered equivocal and warrant repeat testing. This diagnostic threshold is particularly meaningful in cases of acute infections and in patients who have not received prior antibiotics. In chronic or previously treated cases, clinical symptoms must also be considered for accurate interpretation.
Localization Testing
Differentiating between upper and lower urinary tract infections is important since the treatment and prevention strategies differ. Methods for this distinction include symptom-based differentiation, urinalysis, urine culture, urinary fluorescence immunoassays, urinary enzyme tests, and cystoscopy, which are discussed in detail in subsequent sections.
Imaging Studies
Imaging modalities include ultrasound, plain radiographs of the urinary tract, excretory urography, cystography or urethrography, CT or CT urography (CTU), radionuclide imaging, and magnetic resonance urography (MRU). The clinical significance of these studies includes:
- Determining the presence of urinary tract anomalies.
- Identifying obstructive lesions.
- Assessing whether stones, tumors, or benign prostatic hyperplasia are present.
- Evaluating abnormalities in urodynamic function.
- Assessing renal function in each kidney and comparing bilateral renal function.
- Detecting vesicoureteral reflux.
- Monitoring residual urine volume and the emptying time of the renal pelvis and bladder.
These imaging studies are particularly valuable in patients with chronic or refractory urinary infections.
Treatment Principles
Identification of the Nature of the Infection
When symptoms of urinary tract infection are present, it is essential to determine the nature of the infection and the causative organisms. Diagnosis can be guided by urine bacterial and fungal cultures, acid-fast bacilli staining, and antibiotic sensitivity tests. The selection of targeted treatments is critical. In the absence of urine culture results, a preliminary assessment of causative pathogens may be based on Gram staining of urinary sediment smears, with treatment tailored accordingly.
Differentiation Between Hematogenous and Ascending Infection
Hematogenous infections often present with acute onset, systemic symptoms such as chills and high fever, and typically require antibacterial agents with high blood concentrations, which are commonly administered intravenously. Ascending infections are characterized by symptoms of bladder irritation and generally require antibacterial agents with high urinary concentrations alongside spasmolytic medications.
Evaluation of Obstructive Factors in the Urinary System
Urinary obstruction is often a direct contributing factor in the development of urinary tract infections. If an infection coincides with an obstruction, it becomes more difficult to treat, increases the likelihood of resistant bacterial strains, and heightens the risk of recurrence. Timely removal of the obstruction is crucial.
Investigation of Additional Predisposing Factors for Infection
Other factors such as diabetes mellitus, immunosuppressant use, or malignancies should be identified and corrected when feasible, as these conditions can exacerbate infection risks.
Measurement of Urine pH
Urine pH should be determined prior to treatment. For acidic urine, alkalinizing agents such as sodium bicarbonate may be used to create an alkaline urine environment, inhibiting bacterial growth and enhancing the efficacy of antibiotics suited to such conditions. Conversely, for alkaline urine, acidifying agents such as vitamin C can be employed, alongside antibiotics optimized for acidic environments.
Distinction Between Upper and Lower Urinary Tract Infection
Differentiation between these two types of infections is important due to differences in treatment approaches. Upper urinary tract infections are more severe, prone to recurrence, and associated with poorer prognoses, while lower urinary tract infections are generally mild, less likely to recur, and have better outcomes.
Appropriate Use of Antibacterial Agents
The goal of treatment for urinary tract infections is the complete eradication of bacteria from the urinary system. Therapy must ensure that sufficient concentrations of antibacterial agents are achieved in the urine, as urinary drug concentrations should be several hundred times higher than blood concentrations for effective treatment. With properly administered antibiotics, bacteria can be eliminated within hours, but the treatment period should last 7–10 days, with follow-up urine cultures performed to confirm the eradication of bacteria. If the bacterial count remains suppressed at low levels (e.g., a few hundred colony-forming units per milliliter), the infection is likely to recur quickly after discontinuation of treatment. Therefore, the use of antibacterial agents should generally continue until symptoms resolve and urine cultures are negative for at least two weeks. During antibiotic therapy, bacterial mutations may occur, leading to resistant strains. To reduce the risk of resistance, the concurrent use of two or more antibacterial agents may be considered.