Laboratory Examinations
Urine Testing
Urine Collection
Fresh midstream urine is generally preferable for collection. For male patients with redundant foreskin, retraction of the foreskin and cleaning of the glans penis are required. For female patients, cleansing of the vulva and separation of the labia are necessary, with urine collection avoided during menstruation. Clean midstream urine is recommended for urine culture, while catheterized specimens can be used for female patients. Suprapubic bladder aspiration offers uncontaminated bladder urine samples. For neonates and infants, sterile plastic bags are used for urine collection.
Urine Sediment
Centrifuged fresh urine is analyzed under a microscope to assess urine sediment. A count of over three red blood cells per high-power field indicates microscopic hematuria, and more than five white blood cells per high-power field indicates pyuria (also referred to as leukocyturia). Crystals, casts, bacteria, yeast, and parasites are also examined in the sediment.
Three-Glass Test
The first 5–10 ml of urine is designated as the first sample, the last 2–3 ml of urine is the third sample, and the remainder in between is the second sample. Continuous and uninterrupted urinary flow is necessary during collection. Test results provide an initial assessment of the origin and location of microscopic hematuria or pyuria. Abnormalities in the first sample suggest lesions in the urethra, while abnormalities in the third sample indicate lesions in the bladder neck or posterior urethra. Uniform abnormalities across all three samples suggest lesions in the bladder or the upper urinary tract.
Urinary Bacteriology
Gram staining of urinary sediment smears facilitates a preliminary identification of bacterial types, providing guidance for appropriate antibiotic use. Acid-fast staining or Mycobacterium tuberculosis culture of urinary sediment aids in diagnosing renal tuberculosis. A clean midstream urine culture showing a colony count greater than 105/ml suggests a urinary tract infection. For patients with urinary symptoms, a pathogenic bacterial colony count greater than 102/ml is considered significant.
Urinary Cytology
This method is employed for the preliminary screening or postoperative follow-up of bladder tumors. Positive findings suggest the possibility of urothelial tumors at any location within the urinary tract. The sensitivity for detecting early low-grade tumors is low, while the positivity rate for high-grade tumors and carcinoma in situ is relatively high.
Prostatic Fluid Examination
Normal prostatic fluid appears pale white and is thin in consistency. Microscopic examination reveals abundant lecithin bodies, with fewer than 10 white blood cells per high-power field. A high concentration of clustered white blood cells indicates prostatitis. Comparing white blood cell counts in urine samples obtained before and after prostatic massage offers clinical insight into whether the urinary infection is prostatitis-induced. For suspected bacterial prostatitis, bacterial culture and drug sensitivity testing of prostatic fluid are performed.
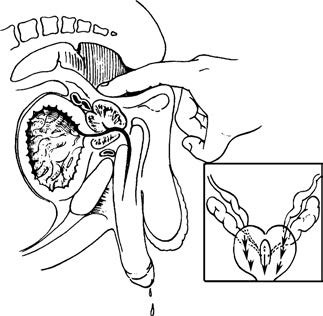
Figure 1 Prostate massage
Semen Analysis
Semen samples are collected via masturbation, coitus interruptus, or a semen collection device. Abstinence from sexual activity or masturbation is required for five days before testing. Routine semen analysis evaluates parameters such as color, volume, pH, viscosity, sperm characteristics, and seminal plasma biochemistry.
Urinary Tumor Markers
Bladder tumor antigen (BTA) testing provides a simple method with approximately 70% accuracy in diagnosing bladder cancer. Fluorescence in situ hybridization (FISH) has high specificity for urothelial tumors and is more sensitive than cytology for detecting shed tumor cells.
Prostate-specific antigen (PSA) is a single-chain glycoprotein comprising 237 amino acids, secreted by epithelial cells of prostate acini and ducts, with specificity for prostate tissue. Elevated PSA levels suggest a likelihood of prostate cancer and are used for screening, early diagnosis, staging, treatment efficacy evaluation, and follow-up monitoring of prostate cancer. Normal PSA levels range from 0–4 ng/ml, while levels above 10 ng/ml strongly indicate suspected prostate cancer. Procedures such as digital rectal examination, prostatic massage, needle biopsy, transurethral ultrasound, transurethral resection, or prostatitis episodes can cause varying degrees of elevation in serum PSA. Testing should be delayed for at least two weeks after these procedures. PSA levels correlate with age and prostate volume, increasing as these factors rise. The influence of medications such as finasteride on PSA levels should also be considered. PSA density (PSAD) and the ratio of free PSA (fPSA) to total PSA (tPSA) aid in distinguishing between benign prostatic hyperplasia and prostate cancer.
Imaging Examinations
Ultrasound
Ultrasound is widely utilized in urology for the screening, diagnosis, and follow-up of diseases. During ultrasound examination, fluids appear as anechoic areas and provide optimal imaging, while homogeneous solid tissues and materials can also be observed. It can detect radiolucent calculi but has limited visibility for gas. Clinically, it is used to determine the nature of renal masses, detect stones and hydronephrosis, measure residual urine, assess prostate volume, and evaluate scrotal masses, as well as the spatial relationship between the testes and epididymis. Transrectal ultrasound facilitates the diagnosis and staging of bladder and prostate tumors. Contrast-enhanced ultrasound is applicable to patients with renal failure or those for whom intravenous urography (IVU) or X-ray exposure is contraindicated.
X-ray Examinations
Plain Film of the Kidney-Ureter-Bladder (KUB)
The renal contour, location, size, psoas muscle opacity, and radio-opaque opacities can be visualized. Absence of the psoas muscle opacity suggests retroperitoneal inflammation or perirenal infection. Lateral X-ray views assist in identifying the source of radio-opaque opacities such as stones. Adequate bowel preparation is required before imaging.
Excretory Urography (Intravenous Urogram, IVU)
This technique involves intravenous injection of an iodinated contrast agent, allowing assessment of urinary tract morphology for any irregularities, dilatation, displacement, compression, or filling defects. Contralateral renal function can also be evaluated. In individuals with normal renal function, the urinary tract becomes visible within five minutes, with complete visualization of both kidneys, ureters, and a partially filled bladder by ten minutes. A pretest iodine sensitivity check is necessary. IVU is contraindicated during pregnancy or in cases of severe renal impairment.
Retrograde Pyelography (RP)
Catheterization of the ureter via cystoscopy and injection of an iodinated contrast agent reveal the ureter and renal collecting system. This examination serves cases where IVU produces unclear results or is contraindicated, helping identify causes of filling defects in the renal pelvis or ureter. Air may also be introduced as a negative contrast for detecting radiolucent stones.
Anterograde Pyelography
Under ultrasound guidance, percutaneous renal pelvis puncture is performed to inject contrast agents and visualize the upper urinary tract. It is indicated for suspected obstructive lesions when other contrast imaging methods fail or are contraindicated.
Cystography
A catheter is introduced into the bladder to instill contrast agents, demonstrating bladder morphology and lesions such as injuries, deformities, fistulas, neurogenic bladder, and bladder tumors. Voiding cystourethrography provides additional information on vesicoureteral reflux and urethral lesions.
Angiography
This imaging modality is applicable for assessing renal vascular diseases, renal injuries, and renal parenchymal tumors. Digital subtraction angiography (DSA) clearly visualizes blood vessels with a diameter greater than 1 mm, aiding in the identification of microaneurysms, arteriovenous malformations, and fistulas within the renal parenchyma and permitting immediate embolization therapy. Embolization therapy for advanced renal tumors can also be conducted.
Lymphangiography
Injection of iodized oil into the dorsal lymphatics of the foot visualizes the inguinal, pelvic, retroperitoneal lymph nodes, and lymphatic vessels. This assessment provides evidence of lymph node metastasis and lymphatic obstruction in bladder, penile, testicular, and prostate cancers, as well as evaluates lymphatic pathways in patients with chyluria.
Seminal Ductography
Contrast agents are injected through vas deferens puncture or ejaculatory duct catheterization, outlining the vas deferens, seminal vesicles, and ejaculatory ducts. This examination applies to conditions such as hematospermia.
CT Scanning
CT imaging is valuable for differentiating renal cysts from solid renal lesions, determining the extent and severity of renal injuries, and diagnosing and staging renal cell carcinoma, bladder cancer, prostate cancer, and adrenal tumors. It can also detect metastatic lymph nodes in the abdomen and pelvis. CT urography (CTU), performed before and after intravenous contrast injection, produces continuous scans of the renal calyces, renal pelvis, ureters, and bladder using multi-slice spiral CT. This technique generates three-dimensional images of the entire urinary system, offering superior imaging quality compared to IVU.
Magnetic Resonance Imaging (MRI)
MRI provides more reliable evidence compared to CT in differentiating between benign and malignant renal tumors, assessing the depth of bladder wall invasion by bladder tumors, staging of prostate cancer, and confirming incidentally identified adrenal masses. Magnetic Resonance Angiography (MRA) is a non-invasive three-dimensional vascular imaging technology. It is used for conditions such as renal artery aneurysms, renal arteriovenous fistulas, renal artery stenosis, renal vein thrombosis, and staging of renal cancer, particularly in evaluating vascular infiltration and assessing vascular patency following renal transplantation. Magnetic Resonance Urography (MRU) is a form of magnetic resonance water imaging. It does not rely on renal function and enables visualization of the morphology and structure of the renal calyces, renal pelvis, and ureters without the use of contrast agents or catheterization. This provides a non-invasive method for evaluating upper urinary tract obstructions. Static body fluids, like urine, have a prolonged T2 relaxation time. Using heavily T2-weighted imaging, water appears as high signal intensity, while soft tissue appears as low signal intensity. After processing, the urinary tract containing urine can be visualized in a manner similar to intravenous urography, making it suitable for cases where urography fails or produces suboptimal imaging.
Radionuclide Imaging
Radionuclide imaging involves small quantities of radioactive materials, causing minimal radiation harm and allowing visualization of organ structure and function without disrupting normal physiological processes.
Renography
Renography provides a function curve based on radionuclide activity measured over time in both kidney regions. It can assess tubular secretion function and reveal obstructions in the upper urinary tract. As a test of unilateral renal function, it reflects urinary tract patency and urinary excretion rates. While its sensitivity is high, its specificity and quantitative reliability are relatively lower.
Renal Scintigraphy
Renal scintigraphy includes both static and dynamic imaging. Static imaging demonstrates the distribution of radionuclides within the kidneys, while dynamic imaging captures the entire process of radionuclide uptake, concentration, and excretion by the kidneys. Dynamic imaging allows assessment of renal size, shape, the presence of space-occupying lesions, renal function, glomerular filtration rate, and effective renal blood flow. Single Photon Emission Computed Tomography (SPECT) enables the observation of dynamic organ functions and provides anatomical and functional imaging in sagittal, coronal, and transverse planes. Renal scintigraphy is more sensitive than urography in patients with impaired renal function and is especially useful for postoperative observation of complications such as obstructions, urinary leakage, or arterial anastomotic stenosis in renal transplant patients.
Adrenal Cortex and Medulla Scintigraphy
This method has diagnostic value for adrenal diseases and is particularly applicable for adrenal space-occupying lesions such as pheochromocytomas.
Scrotal Scintigraphy
Radionuclide blood flow imaging helps determine testicular viability and compare blood perfusion with the contralateral testis. This technique is commonly used in cases of suspected testicular torsion or varicocele.
Bone Scintigraphy
Bone imaging enables detection of systemic skeletal involvement in metastatic conditions, such as renal or prostate cancer bone metastases. SPECT bone imaging outperforms X-ray radiography in sensitivity and accuracy.
Specialized Equipment Examinations
Urethral Catheterization
Urethral catheters vary in material, shape, size, and purpose, with the Foley catheter being the most commonly used type. This type of catheter has two lumens, one of which is used for inflation with air or water to secure the catheter in the bladder. The size of a catheter is indicated by its circumference in French units (F), where 21F corresponds to a circumference of 21 mm and a diameter of 7 mm. Catheters are utilized for draining urine, relieving urinary retention, measuring residual urine, and introducing contrast agents to determine the presence of bladder injury. Both diagnostic and therapeutic procedures require adherence to strict aseptic techniques.
Urethral Sound
Typically made of metal, urethral sounds are primarily used as preparation for cystoscopy, as well as for treating urethral strictures and bladder neck contractures. Urethral dilation is generally performed with sounds measuring 18–21F. Extreme caution is required during dilation to avoid vigorous force that could result in posterior urethral rupture.
Cystourethroscopy
This examination allows for comprehensive evaluation of the urethra and bladder. Biopsy forceps can be used to obtain tissue samples for pathological examination. Ureteral catheters may be introduced via a catheterization bridge through the ureteral orifices to perform retrograde pyelography or collect renal pelvic urine for testing. Procedures such as ureterolithotomy and the placement of double-J stents for internal drainage can also be carried out. Moreover, resectoscopes enable more complex operations involving the urethra, bladder, or prostate. Conditions such as urethral strictures, bladder inflammation, or excessively small bladder capacity preclude the use of this procedure.
Ureteroscopy and Nephroscopy
Ureteroscopes are available in rigid and flexible types and are inserted into the ureters and renal pelvis via the urethra and bladder. Nephroscopes are introduced into the renal calyces and renal pelvis through percutaneous nephrostomy. These devices allow direct visualization of lesions in the ureters and renal pelvis, as well as the removal or fragmentation of stones, tumor resection or cauterization, and collection of biopsy specimens for pathological evaluation. Indications include urinary system calculi, unexplained gross hematuria or positive urinary cytology, and upper urinary tract filling defects. Contraindications include uncorrected systemic bleeding disorders, severe cardiopulmonary insufficiency, uncontrolled urinary tract infections, ureteral obstruction below the lesion, and other contraindications to cystoscopy.
Needle Biopsy of the Prostate
Needle biopsy is the most definitive diagnostic method for prostate cancer and can be performed via transrectal or transperineal approaches. Targeting is facilitated by transrectal ultrasound guidance. Prostate biopsies are conducted after PSA testing and MRI evaluation in patients presenting with palpable prostate nodules on digital rectal examination or abnormal PSA levels.
Urodynamics
Urodynamic studies utilize principles of fluid mechanics and electrophysiology to analyze and measure the functions of urine transport, storage, and voiding. They provide objective evidence for identifying the causes of voiding dysfunction, selecting appropriate treatment, and evaluating therapeutic outcomes. In clinical practice, urodynamic testing is primarily applied for diagnosing lower urinary tract obstruction (such as benign prostatic hyperplasia), neurogenic voiding dysfunction, urinary incontinence, and enuresis.