The main symptoms are categorized into four groups: (1) symptoms directly related to the urinary or male reproductive system, such as hematuria or scrotal masses; (2) symptoms associated with other organ systems, such as nausea, vomiting, or bone pain; (3) systemic symptoms, such as fever or weight loss; and (4) asymptomatic cases where abnormalities, such as kidney stones or renal tumors, are discovered incidentally during other examinations. Key aspects discussed in this section include pain, lower urinary tract symptoms, urinary abnormalities, and sexual dysfunction.
Pain
Pain is a common and significant symptom, which can manifest as colicky, burning, dull, or aching pain. Based on its duration, pain is classified as continuous or intermittent. Colicky and burning pain are often more intense and are typically caused by obstructions or inflammation. Obstruction can increase the pressure within hollow organs, such as the ureter, while inflammation may trigger smooth muscle spasms, capsular edema, or increased tension and swelling (e.g., in acute prostatitis or acute epididymitis), all of which may lead to severe pain. Tumors of the urinary system generally do not cause pain until late-stage disease when associated pain suggests advanced progression of the condition.
Pain in the Kidney and Ureter
Renal pain is usually localized to the ipsilateral costovertebral angle (the junction of the 12th rib and the lateral border of the erector spinae muscle). Pain in this region occurs when the affected kidney experiences capsular distension, inflammation, or dilation of the collecting system. The pain is generally dull, continuous, and localized to the costovertebral angle. Occasionally, it may be sharp and radiate to the flank, groin, or ipsilateral testis or scrotum. Ureteral pain typically presents as an acute onset and is most often caused by urinary stones or blood clots obstructing the upper urinary tract.
Pain due to acute obstruction or dilation at the ureteropelvic junction or ureter is referred to as renal colic. This pain is characterized by its colicky, paroxysmal nature and extreme severity, often accompanied by restlessness, profuse sweating, nausea, and vomiting. Since the kidney and its capsule receive sensory innervation from the T10–L1 spinal nerves, the pain location for upper ureteral disease is similar to pain originating from kidney conditions. Obstruction of the mid-ureter may cause pain that radiates to the right lower quadrant (mimicking appendicitis) on the right side and to the left lower quadrant (mimicking diverticulitis) on the left side. Disorders of the distal ureter often result in bladder irritation symptoms, such as urinary frequency and urgency, along with discomfort in the suprapubic region. Pain from ureteral disease may sometimes radiate to the scrotum, labia, or glans penis.
Bladder Pain
Bladder pain is generally caused by acute urinary retention, bladder overdistension, or inflammation. Acute urinary retention may lead to distension and discomfort in the bladder region, with the presence of a palpable lower abdominal mass and dullness on percussion over the suprapubic area. Chronic urinary retention or slow bladder distension, such as in hypotonic neurogenic bladder caused by diabetes, may not elicit pain even when the residual urine volume exceeds 1,000 mL. Bladder infections typically present with intermittent discomfort in the suprapubic area, with pain worsening during bladder filling and significantly relieved after voiding. The pain is often sharp or burning in nature, particularly at the end of urination when stabbing pain may be felt in the suprapubic area, radiating to the distal urethra, and accompanied by bladder irritation symptoms.
Prostate Pain
Prostate pain results from tissue edema and capsular distension due to prostatitis. This may cause perineal, rectal, or lower back pain, occasionally radiating to the suprapubic region, inguinal area, or testicles. Associated symptoms may include urinary frequency or dysuria.
Scrotal Pain
Scrotal pain is typically caused by testicular or epididymal conditions such as trauma, testicular torsion, torsion of testicular or epididymal appendages, or infection. Testicular torsion and acute inflammation of the testis or epididymis may result in testicular swelling and intense pain, requiring differentiation. Scrotal pain may also be due to inflammation of the scrotal wall itself, such as folliculitis or sebaceous cysts. Additionally, conditions like hydrocele, varicocele, or testicular tumors may cause chronic dull pain or a sensation of heaviness without radiation. Groin hernias may present with dull pain radiating to the scrotum.
Penile Pain
Penile pain, in the non-erect state, is often related to bladder or urethral inflammation, such as gonorrhea, with referred pain at the urethral meatus. It may also be caused by paraphimosis, which results from venous and lymphatic congestion due to entrapment of the penile foreskin and glans. In the erect state, penile pain is associated with conditions such as priapism.
Lower Urinary Tract Symptoms (LUTS)
Lower urinary tract symptoms (LUTS) encompass all symptoms related to voiding dysfunction. They are broadly categorized into storage phase symptoms and voiding phase symptoms, with the former mainly presenting as irritative symptoms and the latter as obstructive symptoms.
Irritative Symptoms
Frequency
In healthy adults, the normal frequency of urination is approximately 5–6 times per day, with 0–1 nighttime urinations. Each void typically yields about 300 mL, though urination frequency and volume are influenced by factors such as ambient temperature, hydration, and activity levels. Frequency refers to a noticeable increase in the urge to urinate, which can become severe enough that urination occurs every few minutes, each time producing only a small amount of urine. Conditions such as genitourinary inflammation, bladder stones, tumors, or prostatic hyperplasia may result in frequency, often due to inflammatory edema or reduced bladder compliance leading to decreased bladder capacity, or to persistent urinary retention reducing effective bladder capacity.
If the frequency increases without a reduction in voided volume—sometimes with increased volume—it may be physiological (e.g., increased fluid intake, consumption of diuretic food) or pathological (e.g., diabetes mellitus, diabetes insipidus, or impaired renal concentrating ability). Psychological factors, such as anxiety, may also contribute to frequent urination. Nocturnal frequency, or nocturia, often arises from bladder outlet obstruction and/or decreased bladder compliance. Generally, normal nighttime urinary frequency does not exceed two episodes. Increased urinary frequency, especially nocturia, is one of the earliest and most prominent symptoms of benign prostatic hyperplasia (BPH).
Urgency
Urgency refers to a sudden, irresistible urge to void, often resulting in the passage of only a small amount of urine. It frequently coexists with frequency. Common causes include acute lower urinary tract infections, hypersensitive and low-compliance neurogenic bladder, and bladder outlet obstruction. Additionally, psychological factors such as anxiety or fear can lead to urgency. A clinical syndrome known as overactive bladder (OAB) is characterized by urgency, often accompanied by frequency and nocturia, with or without urge incontinence. Though the pathogenesis of OAB remains unclear, it can manifest in association with various conditions, including bladder outlet obstruction, neurogenic bladder dysfunction, and genitourinary infections. OAB symptoms in BPH may occur as secondary effects or as overlapping primary symptoms.
Dysuria
Dysuria refers to painful urination, which may occur at the beginning, during, or at the end of urination, or even afterward. The pain is burning in nature and is often related to infections of the bladder, urethra, or prostate. In males, the pain is more commonly felt at the distal urethra, while in females, it tends to involve the entire urethra. Dysuria often coexists with frequency and urgency, and when they occur together, they are collectively referred to as irritative bladder symptoms.
Obstructive Symptoms
Difficulty in Urination
This encompasses several manifestations, including urinary hesitancy, straining, incomplete emptying, reduced urinary stream force, split or forked urinary stream, thinning of the urinary stream, and post-void dribbling. These symptoms are often caused by obstruction of the lower urinary tract below the bladder and are frequently seen in BPH.
- Urinary hesitancy refers to a delayed onset of urination.
- Straining involves the use of abdominal pressure to initiate urination.
- Incomplete emptying describes the sensation of residual urine remaining in the bladder after voiding.
- Split or forked urinary stream refers to the division of the urinary flow into two streams or a scattered pattern.
- Thinning of the urinary stream occurs due to increased outflow resistance.
- Dribbling refers to the leaking of small amounts of urine from the urethral meatus following voiding.
Interruption of Urinary Stream:
This refers to an involuntary interruption of urinary flow during voiding, which subsequently resumes and repeats in a cyclic manner. It is often accompanied by pain that may radiate to the distal urethra. A common cause is bladder stones forming a ball-valve obstruction at the bladder neck, temporarily blocking urinary flow. It can also be seen in BPH due to intermittent obstruction caused by enlarged lateral or middle lobes of the prostate.
Urinary Retention:
Urinary retention is classified as acute or chronic.
Acute urinary retention occurs due to severe obstruction of the lower urinary tract below the bladder or due to an inability to void following abdominal or perineal surgery. Men may experience this condition more frequently in BPH, prostate tumors, or urethral strictures causing bladder outlet obstruction. The sudden inability to void leads to retention of urine in the bladder, causing suprapubic distension.
Chronic urinary retention occurs in cases of incomplete bladder outlet obstruction or neurogenic bladder and is characterized by difficulty in urination, suprapubic swelling, discomfort, or pain. Severe cases may result in overflow incontinence. Intermittent clean self-catheterization is often necessary for chronic retention caused by dynamic obstruction. Patients unable to perform self-catheterization or those with severe upper urinary tract hydronephrosis may require suprapubic cystostomy or urinary diversion procedures.
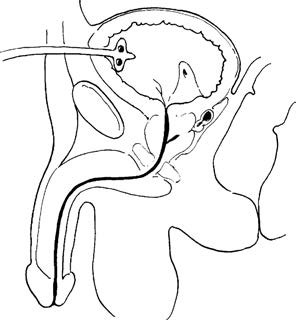
Figure 1 Suprapubic cystostomy
Differentiating between irritative and obstructive symptoms is of critical importance within LUTS. Although BPH commonly causes urinary obstruction, it may also lead to secondary decreased bladder compliance, resulting in irritative symptoms that are even more prominent, particularly nocturia. It should be noted that LUTS are nonspecific and may result not only from prostate enlargement but also from other conditions such as cerebrovascular accidents, diabetes, or Parkinson's disease.
Urinary Incontinence
Urinary incontinence refers to the involuntary leakage of urine due to a loss of control over urination. It is classified into four main types:
Continuous Urinary Incontinence
Also referred to as true incontinence, this is characterized by a complete loss of the ability to control urination. Urine leaks continuously and involuntarily from the urethral orifice regardless of time or body position. This condition is commonly caused by trauma, surgery, or congenital abnormalities leading to damage to the bladder neck or urethral sphincters. It is frequently observed in cases of vesicovaginal fistula caused by gynecological surgeries or obstetric injuries. Ureterovaginal fistula is less common. In men, prostate surgery can result in damage to the external urethral sphincter, leading to incontinence. In congenital cases, an ectopic ureter may open into the urethra, vagina, or the vestibule of the external genitalia. Since ectopic ureters are often associated with underdeveloped kidneys, most female patients experience continuous, mild urinary leakage but still maintain normal bladder urination. This often leads to a misdiagnosis of chronic vaginal discharge.
Overflow Urinary Incontinence
This refers to intermittent, involuntary urine leakage from the urethral orifice, typically occurring as dribbling, which is most noticeable at night. It often affects individuals with chronic lower urinary tract obstruction, such as those with benign prostatic hyperplasia, tumors, or urethral strictures. In such cases, the bladder fails to empty completely during each urination, leading to a gradual increase in residual urine. When the bladder becomes excessively distended and the intravesical pressure surpasses the resistance of the urethra, urine begins to leak out in a dribbling manner. Overflow incontinence can also occur when detrusor muscle weakness is caused by neurological conditions. Since overflow incontinence can often be resolved by relieving bladder outlet obstruction, it is sometimes referred to as "pseudo-incontinence."
Urge Urinary Incontinence
This type occurs when severe urinary frequency and urgency culminate in involuntary urination without conscious control over the bladder. It is typically secondary to bladder inflammation, neurogenic bladder dysfunction, or severe bladder outlet obstruction. This type of incontinence is commonly associated with unstable bladder contractions.
Stress Urinary Incontinence
This refers to instances where individuals maintain normal control over urination under ordinary conditions but experience involuntary leakage of small amounts of urine during situations of increased intra-abdominal pressure, such as coughing, laughing, sneezing, standing, or running. It primarily occurs in multiparous or postmenopausal women due to weakened support of the anterior vaginal wall or dysfunction of pelvic tissues. Stress urinary incontinence can also occur in men after prostate surgery, particularly following radical prostatectomy, as a result of damage to the external urethral sphincter; however, most cases are reversible.
Enuresis
Enuresis refers to involuntary nocturnal urination occurring during sleep, separate from normal voluntary urination. This condition is physiological in newborns and young children. Beyond the age of three, pathological factors such as neurogenic bladder, infections, or posterior urethral valves may contribute to enuresis, in addition to functional causes. It is necessary to differentiate enuresis from continuous urinary incontinence. For younger women, enuresis is commonly associated with an ectopic ureter opening. Children older than six years with enuresis should undergo urinary system examinations.
Changes in Urine
Urine Volume
Normal 24-hour urine output in healthy individuals is between 1,000 and 2,000 ml. Oliguria and anuria result from decreased renal excretion, and the causes of reduced urine output can be classified into prerenal, renal, and postrenal factors. Determining the presence of ureteral or urethral obstruction is essential. Urine output of less than 100 ml/24 h is classified as anuria, which is typically a manifestation of persistent anuria caused by organic renal damage, often associated with azotemia or uremia. Urine output less than 400 ml/24 h or less than 17 ml/hour is classified as oliguria. This condition is most frequently observed in cases of prerenal renal failure caused by severe dehydration, shock, or renal artery stenosis; renal renal failure caused by glomerulonephritis, polycystic kidney disease, or rejection following kidney transplantation; or postrenal renal failure caused by urinary tract malformations or obstructions. Polyuria is characterized by a urine output of 3,000 to 5,000 ml/24 h, often observed during the diuretic phase of acute postrenal kidney injury due to impaired renal concentrating ability and solute diuresis.
Appearance of Urine
Hematuria
The presence of red blood cells in the urine is classified into gross hematuria and microscopic hematuria. Gross hematuria refers to visible blood in the urine, which typically becomes apparent when 1 ml of blood is present in 1,000 ml of urine. Microscopic hematuria requires the use of a microscope to detect red blood cells in the urine. Centrifuging fresh urine and observing more than three red blood cells per high-power field in the sediment is generally considered pathologically significant. Hematuria is one of the critical symptoms of urinary system diseases. The presence or absence of pain is an essential factor in distinguishing between benign and malignant urological conditions. Hematuria with painful urination is often associated with cystitis or urinary calculi, while painless hematuria in middle-aged and elderly individuals commonly suggests urinary tract tumors.
The color of hematuria varies depending on the blood content, urine pH, and bleeding source. Hematuria originating from the kidneys or ureters or occurring in acidic urine tends to appear darker, whereas hematuria from the bladder or in alkaline urine appears brighter red. Severe hematuria may present as diverse blood clots, with worm-like clots often originating from the kidneys or ureters, while clots of varying sizes point to bladder bleeding. Some medications or foods can discolor urine and mimic hematuria, such as rhubarb, phenolphthalein, rifampin, tetracycline antibiotics, phenol red, and purine-related drugs. Hemoglobinuria or myoglobinuria may occur due to significant trauma or massive red blood cell or tissue destruction caused by erroneous blood transfusion.
Cloudy Urine
Cloudy urine may result from crystalluria, pyuria, or chyluria. Crystalluria refers to the presence of organic or inorganic crystalline substances in the urine, often observed when the urinary salt concentration is supersaturated. Pyuria indicates a high number of white blood cells in the urine and is a typical sign of urinary tract infection. After centrifuging fresh urine, an observed white blood cell count of more than five per high-power field in sediment indicates infection or inflammation in the urinary tract. Chyluria appears milky white due to the presence of lymphatic fluid in the urine, which may also contain significant amounts of protein or blood. Cloudy urine that clears upon the addition of ether is indicative of chyluria, confirmed using the ether test (also referred to as the chyle test). The most common cause of chyluria is filarial infection.
Pneumaturia
Pneumaturia refers to the simultaneous expulsion of gas and urine during urination. This condition suggests the presence of a urogenital-gastrointestinal fistula or a urinary tract infection caused by gas-producing bacteria.
Sexual Dysfunction
Male sexual dysfunction includes manifestations such as reduced libido, erectile dysfunction (ED), and ejaculation disorders (including premature ejaculation, anejaculation, and retrograde ejaculation). The most common conditions are erectile dysfunction and premature ejaculation. ED refers to the inability of the penis to achieve normal erection during sexual arousal, insufficient penile rigidity, or inability to sustain an erection long enough for satisfactory sexual activity. The factors contributing to ED are multifaceted and include psychological and emotional factors, vascular abnormalities, neurological conditions, endocrine disorders, medication effects, and systemic diseases.
Premature ejaculation (PE) is divided into primary and secondary types. Primary premature ejaculation refers to onset from the first sexual experience, often occurring within about one minute of vaginal penetration. Secondary premature ejaculation refers to a significant reduction in intravaginal ejaculatory latency, typically occurring within three minutes. Both conditions are characterized by poor control over ejaculation, with an inability or near-inability to delay ejaculation, accompanied by negative impacts on mental and physical well-being, such as distress, anxiety, depression, and/or avoidance of sexual activity.
Hematospermia refers to the presence of blood in normal semen. The most common cause of hematospermia is nonspecific inflammation of the prostate, seminal vesicles, or urethra. Symptoms often gradually subside within a few weeks. If hematospermia persists for several weeks or longer, underlying causes such as genitourinary tuberculosis, tumors, or calculi should be considered.