The pancreas is an elongated retroperitoneal organ that weighs approximately 75–125 g and measures about 15–20 cm in length. It traverses the anterior aspects of the first and second lumbar vertebrae from right to left. Anatomically, the pancreas is divided into four parts: the head, neck, body, and tail, though there are no distinct boundaries separating these regions. The pancreatic head, the most prominent part, is encircled by the C-shaped duodenum. The posterior superior segment of the head is traversed by the common bile duct. The lower portion extends leftward posterior to the superior mesenteric vein, leading to the uncinate process, located behind the superior mesenteric artery. The pancreatic neck lies anterior to the superior mesenteric vein. Between the neck and the tail is the pancreatic body, which is positioned in close proximity to the vertebral bodies. The pancreatic tail, the leftmost section of the pancreas, is adjacent to the splenic hilum.
The main pancreatic duct, or Wirsung duct, is approximately 2–3 mm in diameter, running the length of the pancreas and receiving tributary ducts along its course. In about 85% of individuals, the main pancreatic duct merges with the common bile duct to form a common channel, with its dilated segment known as the ampulla of Vater. This is surrounded by the sphincter of Oddi and terminates at the major duodenal papilla. In some individuals, the two ducts share a common opening but are separated by a septum, while in others, they enter the duodenum via separate openings. The shared channel forms the anatomical basis for the interplay between pancreatic and biliary diseases. In some individuals, an accessory pancreatic duct (Santorini duct) is present above the main duct in the head of the pancreas. It often communicates with the main pancreatic duct and drains the anterior-superior portion of the head, opening at the minor duodenal papilla.
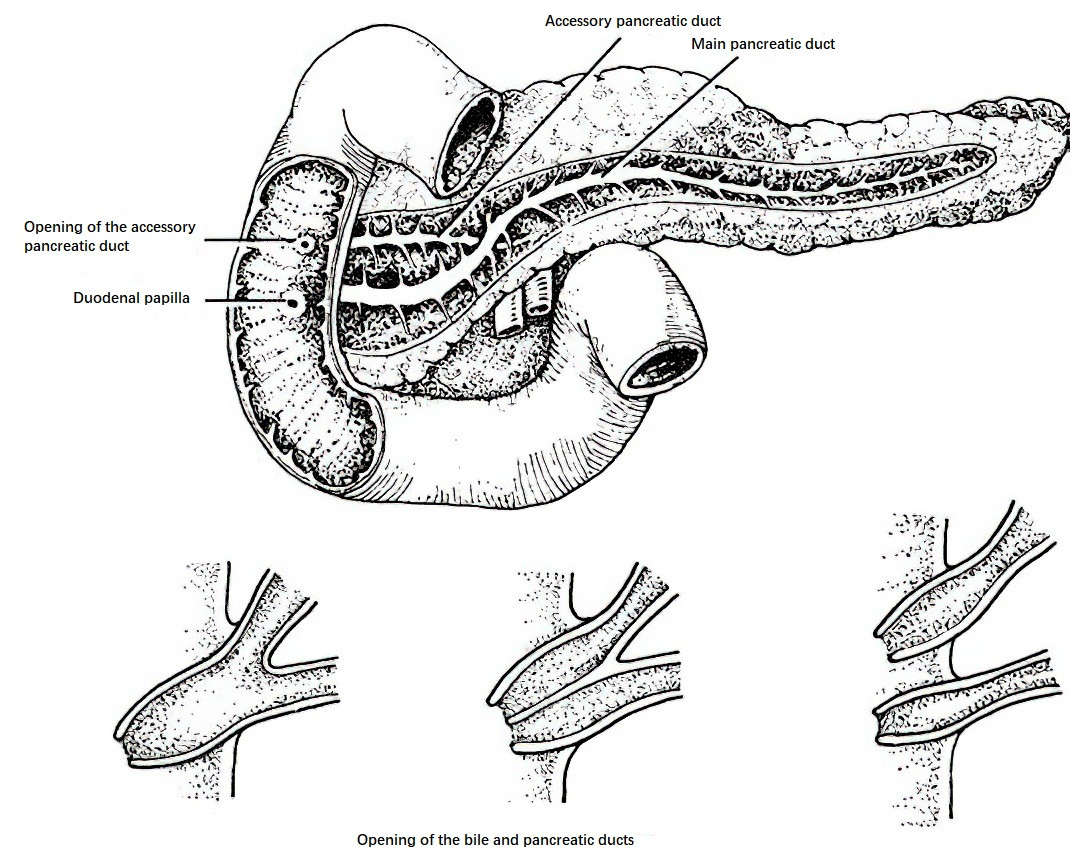
Figure 1 Anatomical relationships of the pancreatic ducts
The blood supply to the pancreatic head originates from the anterior and posterior pancreaticoduodenal arterial arcades, which arise from branches of the gastroduodenal artery and the superior mesenteric artery. The body and tail are vascularized by branches of the splenic artery, including the dorsal pancreatic artery and the great pancreatic artery, which form an intrapancreatic arterial network via the transverse pancreatic artery. Variations in the arterial anatomy are common; for example, the dorsal pancreatic artery may stem from the splenic artery or the common hepatic artery, and the transverse pancreatic artery may originate from the dorsal pancreatic artery, the superior mesenteric artery, or the common hepatic artery. The venous drainage of the pancreas generally follows the course of its arteries, ultimately emptying into the portal vein.
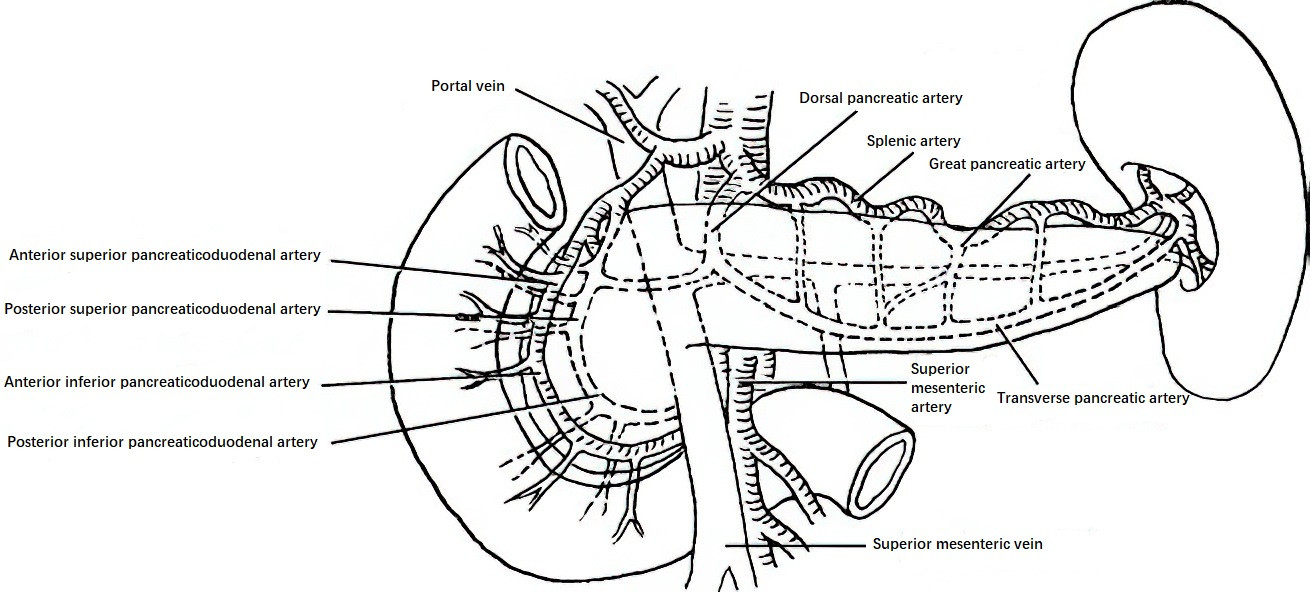
Figure 2 Blood supply of the pancreas
The lymphatic drainage of the pancreas begins with the periacinar capillary lymphatic vessels, which coalesce into larger interlobular lymphatic vessels. These vessels travel along the accompanying blood vessels to the surface of the pancreas and drain into lymph nodes located anterior and posterior to the pancreaticoduodenal area, along the superior margin of the pancreas, and at the splenic hilum. These lymph nodes connect with nodes at the upper and lower pylorus, the hepatic hilum, the transverse mesocolon, and the abdominal aorta. The pancreas receives innervation from both the sympathetic and parasympathetic nervous systems. The sympathetic nerves serve as the primary pathway for pain sensation, while parasympathetic efferents regulate the functions of islet cells, acinar cells, and ductal cells.
The pancreas has both exocrine and endocrine functions. Its exocrine secretion, pancreatic juice, is a clear isotonic fluid with a daily volume of approximately 750–1500 ml and a pH of 7.4–8.4. The primary components are digestive enzymes secreted by acinar cells and water and bicarbonate secreted by ductal cells. The major digestive enzymes include trypsin, chymotrypsin, elastase, amylase, and lipase. The secretion of pancreatic juice is regulated by both the vagus nerve and humoral factors, with humoral control being predominant. Under physiological conditions, these digestive enzymes are stored in their inactive zymogen forms within acinar cells. When released into the duodenal lumen, they are activated by enterokinase to facilitate the digestion of proteins, fats, and starches.
The endocrine hormones of the pancreas are produced by the islets of Langerhans, which are clusters of cells of varying sizes and shapes scattered among the acini. There are an estimated 105 to 106 islets in the human pancreas, with a higher density of islet cells in the body and tail regions compared to the head. The primary cell types within the islets include B (β) cells, which secrete insulin and are the most abundant; A (α) cells, which produce glucagon; and D (δ) cells, which release somatostatin. Additionally, a small number of pancreatic polypeptide (PP) cells secrete pancreatic polypeptide, while D1 cells secrete vasoactive intestinal peptide (VIP).