Applied Anatomy of the Biliary System
The biliary system develops from the embryonic foregut and is divided into the intrahepatic bile ducts and the extrahepatic biliary tract.
Intrahepatic Bile Ducts
The intrahepatic bile ducts originate from the bile canaliculi, which converge to form interlobular bile ducts, segmental ducts, lobar ducts, and the intrahepatic portions of the left and right hepatic ducts. The distribution and course of the branches of the intrahepatic bile ducts, hepatic artery, and portal vein are generally consistent, and they are all enclosed in a connective tissue sheath known as Glisson's sheath. The left and right hepatic ducts constitute the primary branches. The secondary branches include the ducts of the left medial and lateral segments and the right anterior and posterior segments. The tertiary branches correspond to the segmental ducts of the liver.
Extrahepatic Biliary Tract
The extrahepatic biliary tract consists of the left and right hepatic ducts, the common hepatic duct, the gallbladder, the cystic duct, and the common bile duct.
Left and Right Hepatic Ducts and the Common Hepatic Duct
The left hepatic duct is slender, measuring approximately 2.5–4 cm, while the right hepatic duct is shorter and broader, measuring about 1–3 cm. The left and right hepatic ducts exit the liver and converge at the hepatic hilum to form the common hepatic duct. The structures entering or exiting the hepatic hilum—including the left and right hepatic ducts, branches of the portal vein and hepatic artery, lymphatic vessels, and nerves—are collectively known as the hepatic pedicle, which resides within the hepatoduodenal ligament.
At the hepatic hilum, the left and right hepatic ducts and the common hepatic duct are typically located anteriorly and slightly to the right. The hepatic artery and its branches are positioned centrally and slightly to the left, while the portal vein and its branches are posteriorly situated. The convergence of the left and right hepatic ducts is at the highest anatomical position, followed by the bifurcation of the left and right branches of the portal vein at a slightly lower level, with the bifurcation of the left and right branches of the proper hepatic artery at the lowest level.
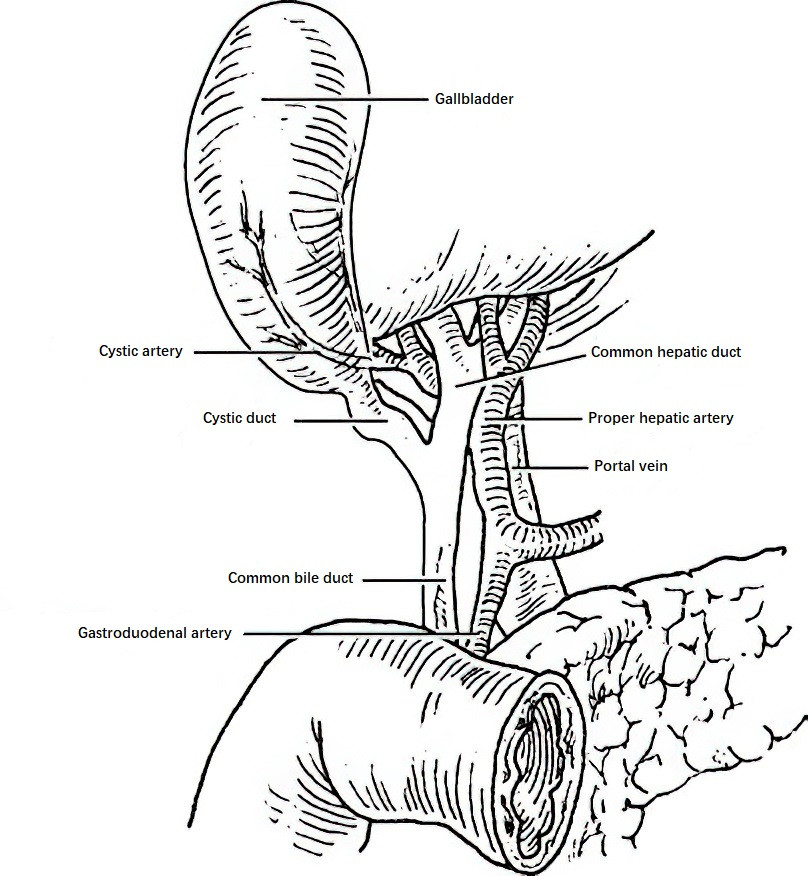
Figure 1 Key structures within the hepatoduodenal ligament
The common hepatic duct generally has a diameter of 0.4–0.6 cm and is approximately 3 cm in length, although it can occasionally reach up to 7 cm. The distal end of the common hepatic duct joins the cystic duct to form the common bile duct. Variations in the anatomy of the bile ducts and associated arteries frequently occur and require consideration during biliary surgery.
Common Bile Duct
The common bile duct is approximately 4–8 cm in length and 0.6–0.8 cm in diameter. It is divided into four segments:
- Supraduodenal Segment: Approximately 1.4 cm in length, this segment descends along the right margin of the hepatoduodenal ligament and is a common site for clinical exploration and drainage of the common bile duct.
- Retroduodenal Segment: Approximately 2 cm in length, this segment travels behind the bulb of the duodenum. The inferior vena cava lies posteriorly, while the portal vein and gastroduodenal artery are located on the left side.
- Pancreatic Segment: Approximately 1–2 cm in length, this segment runs within the bile duct groove or pancreatic parenchyma behind the head of the pancreas. Tumors or masses in the pancreatic head frequently compress or invade this segment, causing obstructive jaundice.
- Intramural Segment: Approximately 1 cm in length, this segment travels obliquely through the posteromedial wall of the descending section of the duodenum. Within the intestinal wall, the common bile duct converges with the main pancreatic duct at the ampulla of Vater, which is a bulb-shaped structure. The ampulla is surrounded by the sphincter of Oddi, and the opening is usually located at the duodenal papilla. Variations in the anatomy of the confluence of the common bile duct and pancreatic duct are common. The sphincter of Oddi comprises several components, including the sphincter of the common bile duct, the sphincter of the pancreatic duct, and the ampullary sphincter. The sphincter regulates the opening of the common bile duct and pancreatic duct and prevents the backflow of duodenal contents.
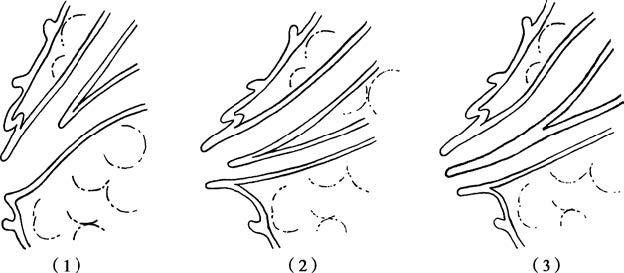
Figure 2 Anatomical variations at the junction of the common bile duct and main pancreatic duct
(1) The common bile duct and the main pancreatic duct merge to form a single duct that opens into the duodenum (approximately 70%).
(2) The common bile duct and the main pancreatic duct have a single opening into the duodenum, without merging into a common duct (approximately 20%).
(3) The common bile duct and the main pancreatic duct open separately into the duodenum (approximately 10%).
Gallbladder
The gallbladder is an intraperitoneal organ with a pear-shaped structure. One side is free and covered by visceral peritoneum, while the other side is located within the gallbladder fossa on the inferior surface of the liver, connected to the liver by connective tissue. The gallbladder measures 5–8 cm in length, 3–5 cm in width, and has a capacity of 30–60 ml. It consists of three parts: the fundus, body, and neck. The fundus is a blind end where perforations of the gallbladder often occur. The upper part of the neck of the gallbladder expands into a pouch known as Hartmann's pouch, where gallstones frequently become lodged.
Cystic Duct
The cystic duct extends from the neck of the gallbladder, measuring 1–5 cm in length and 0.2–0.4 cm in diameter. The mucosal lining of the cystic duct forms spiral folds known as the valves of Heister, which play an important role in preventing gallstones from entering the common bile duct. Various anatomical variations in the cystic duct occur, with an overly long cystic duct that joins the common bile duct at a low level serving as a key anatomical basis for Mirizzi syndrome.
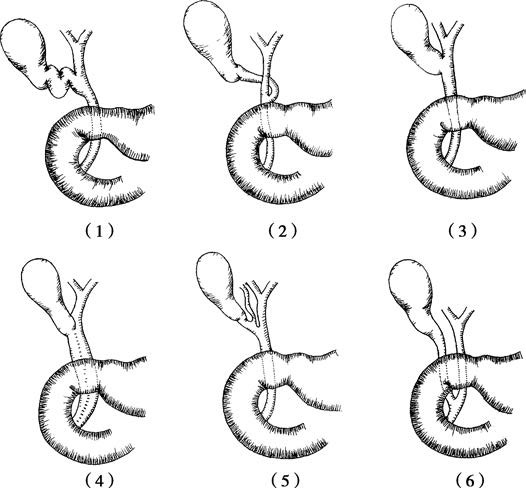
Figure 3 Anatomical variations of the cystic duct
(1) Long and tortuous cystic duct.
(2) Cystic duct merges with the common hepatic duct from the left side.
(3) Short cystic duct.
(4) Cystic duct shares a common wall with the common hepatic duct.
(5) Cystic duct abnormally merges with the anterior or posterior segmental bile duct of the right liver before joining the common bile duct.
(6) Long cystic duct that joins the common bile duct at a low position.
The cystic duct, common hepatic duct, and inferior border of the liver form a triangular area known as Calot's triangle. Important structures, such as the cystic artery, right hepatic artery, and accessory right hepatic duct, often pass through this triangle. The cystic lymph node, located above the angle where the cystic duct meets the common hepatic duct, serves as an anatomical landmark for locating the cystic artery and bile duct during surgery.
Blood Supply, Lymphatics, and Innervation of the Biliary Tract
The blood supply to the biliary tract primarily originates from the gastroduodenal artery, common hepatic artery, and right hepatic artery. Branches from these arteries anastomose around the bile duct walls in a plexiform pattern. The cystic artery supplies the gallbladder, cystic duct, and the upper portion of the common bile duct, while the lower portion of the common bile duct is supplied by branches of the pancreaticoduodenal artery and posterior duodenal artery. The venous drainage of the gallbladder and extrahepatic bile ducts directly empties into the portal vein.
Lymphatic drainage of the gallbladder flows into the cystic lymph nodes and hepatic lymph nodes, with connections to intrahepatic lymph vessels. The lymphatic drainage of the extrahepatic bile ducts flows into lymph nodes located along the posterior of the common hepatic duct and common bile duct.
The biliary system is richly innervated with nerve fibers, which mainly arise from the vagus nerve and sympathetic nerves emanating from the celiac plexus. Excessive traction on the gallbladder during surgery may stimulate the vagus nerve, triggering the gallbladder-cardiac reflex. This may manifest as gallbladder-cardiac syndrome, and in severe cases, may lead to cardiac arrest. Appropriate attention is required to mitigate these effects.
Structural Characteristics of the Biliary Tract
The bile canaliculi are formed by local invaginations of adjacent hepatocyte membranes. These canaliculi connect into a reticular network within the hepatic plates, progressively converging from the central to peripheral regions. At the margins of the lobules, they form short intercalated ducts composed of a single layer of cuboidal epithelium. After emerging from the hepatic lobules, intercalated ducts merge into interlobular bile ducts, which further converge to form the segmental and lobar bile ducts, eventually draining into the left and right hepatic ducts.
The mucosal layer of the extrahepatic bile ducts consists of a single layer of columnar epithelium, which contains goblet cells and other mucus-secreting cells. The muscular layer contains smooth muscle fibers and elastic fibers, which, when stimulated, may undergo spasmodic contraction, leading to colic. The serosal layer is composed of connective tissue containing nerve fibers and vascular branches.
The mucosal layer of the gallbladder is made up of high columnar cells, which facilitate absorption. The base of the mucosa contains tubuloalveolar glands that secrete mucus. Numerous mucosal folds within the gallbladder enhance its capacity to concentrate bile. The muscular layer consists of longitudinal fibers on the inner surface, circular fibers on the outer surface, and elastic fibers in the middle. The outer membrane is formed by connective tissue and serosa, a continuation of the hepatic capsule.
Physiological Functions of the Biliary System
The primary physiological functions of the biliary system include the secretion, storage, concentration, and transport of bile.
Bile Secretion, Composition, and Metabolism
Secretion and Functions of Bile
An adult secretes approximately 800–1,200 ml of bile daily, most of which (roughly three-fourths) is produced by hepatocytes. The remaining portion is secreted by bile duct cells as mucus. Bile is composed of approximately 97% water, with the remaining components including bile acids and bile salts, bile pigments, cholesterol, phospholipids, fatty acids, mucin, and inorganic salts.
Cholesterol is a metabolic byproduct of fats in the body. After metabolism in the liver, cholesterol is converted into primary bile acids, namely cholic acid and chenodeoxycholic acid. In the small intestine, primary bile acids are degraded by bacteria into secondary bile acids, such as deoxycholic acid and lithocholic acid. Free bile acids include cholic acid, deoxycholic acid, chenodeoxycholic acid, and lithocholic acid, which combine with glycine or taurine to form conjugated bile acids (bile salts) in the form of sodium or potassium salts. The primary bile pigment in bile is bilirubin, with oxidative byproducts, such as biliverdin, and reductive byproducts, such as urobilinogen and stercobilinogen, being present in minimal amounts.
Bilirubin, a breakdown product of hemoglobin, may diffuse into tissues and cause jaundice when its uptake by the liver is reduced or when biliary obstruction occurs, leading to increased bilirubin concentrations in the blood. A precise balance of bile salts, cholesterol, and phospholipids is essential to maintaining cholesterol in a dissolved state.
Bile is slightly alkaline and serves several physiological functions, including:
- Emulsification of fats;
- Clearance of toxins and metabolic waste products;
- Suppression of growth and reproduction of pathogenic intestinal bacteria and prevention of endotoxin formation;
- Stimulation of intestinal peristalsis;
- Neutralization of gastric acid.
Regulation of Bile Secretion
Bile secretion is regulated by both neural and humoral factors. Excitation of the vagus nerve increases bile secretion, whereas stimulation of the sympathetic nerve reduces bile secretion. Hormones such as secretin, gastrin, and cholecystokinin (CCK) enhance bile secretion, while somatostatin inhibits it. After gastric acid, fat, and protein degradation products enter the duodenum from the stomach, they stimulate the duodenal mucosa to secrete secretin and CCK. Both of these hormones induce contraction of the smooth muscle of the gallbladder and relaxation of the sphincter of Oddi.
Bile Metabolism
Cholesterol Metabolism
Cholesterol is water-insoluble but dissolves in bile. In bile, micelles formed by bile salts and phospholipids encapsulate cholesterol, enabling its solubility. Cholesterol achieves maximum solubility when the ratio of bile salts to phospholipids is approximately 2–3:1. Bile also contains vesicles composed of equal proportions of phospholipids and cholesterol, without bile salts. These vesicles have a 10–20-fold greater capacity for dissolving cholesterol than micelles, accounting for the dissolution of 70%–80% of cholesterol in bile. When the concentration of bile salts in bile is high, cholesterol predominantly exists in micellar form.
As cholesterol concentration increases, micelles become saturated and the number of vesicles increases. When the cholesterol in vesicles becomes oversaturated, it precipitates out as crystals, leading to the formation of cholesterol gallstones. Bile salts, synthesized from cholesterol in the liver, are secreted into bile and stored and concentrated in the gallbladder.
Bile Salt and Pigment Metabolism
During feeding, bile salts are excreted into the intestine with bile, and approximately 95% of these bile salts are absorbed into the bloodstream, primarily from the ileum. They are transported to the liver via the portal vein, re-enter bile, and are again excreted into the intestine. This process is referred to as the enterohepatic circulation of bile salts. The remaining 5% of bile salts are excreted in feces and urine. As a result, the liver only needs to synthesize a small amount of bile salts (0.2–0.6 g/day) to maintain the stability of the bile salt pool. When enterohepatic circulation is disrupted, the concentration of bile salts in bile decreases, whereas cholesterol concentration increases, making cholesterol more likely to precipitate and form stones.
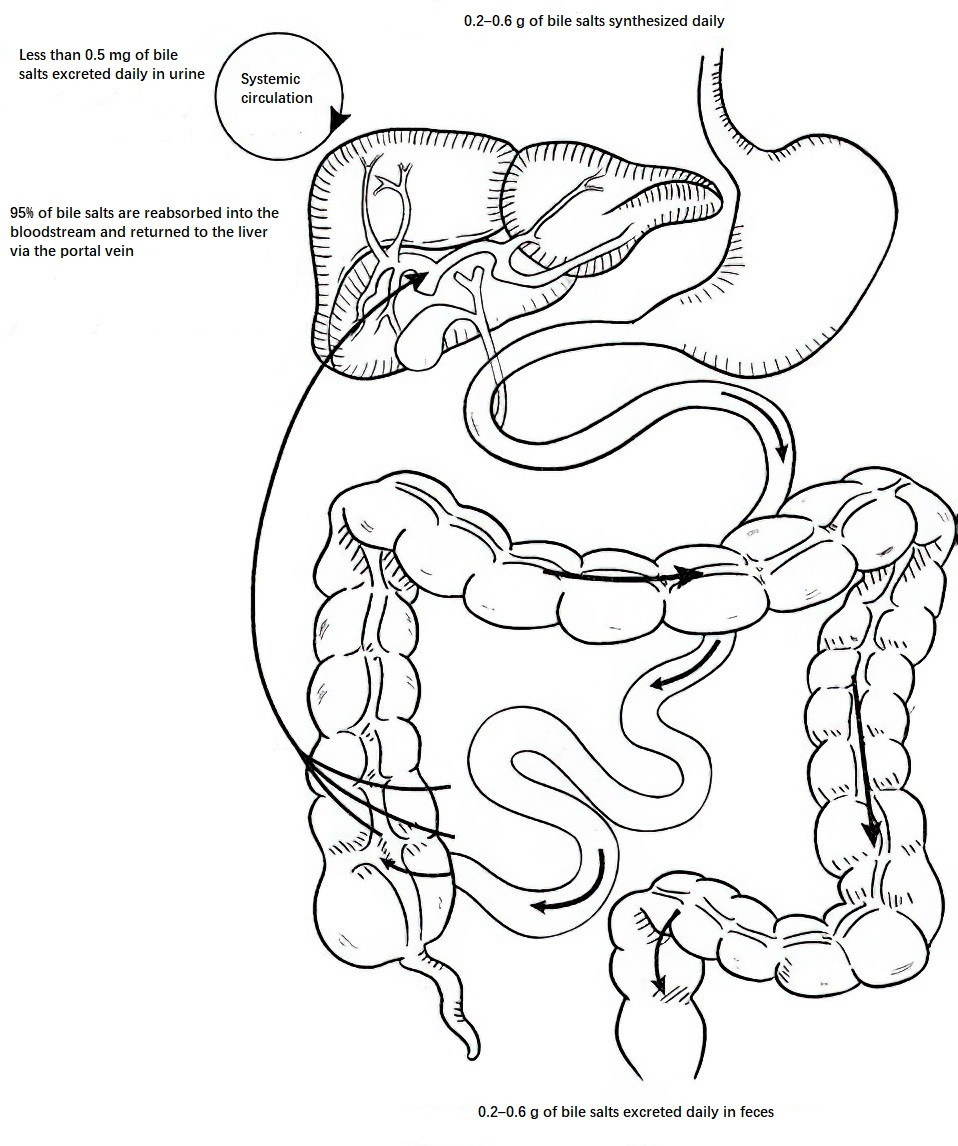
Figure 4 Enterohepatic circulation of bile salts
Unconjugated bilirubin (also known as indirect bilirubin) binds to glucuronic acid in the liver to form soluble conjugated bilirubin (also known as direct bilirubin), which is excreted into the intestine with bile. In the distal ileum and colon, bacterial activity transforms conjugated bilirubin into urobilinogens, a small portion of which is absorbed by the intestine, forming an enterohepatic circulation of bile pigments. If bilirubin in the liver fails to conjugate with glucuronic acid or if there is bile duct infection, β-glucuronidase produced by Escherichia coli can hydrolyze conjugated bilirubin into unconjugated bilirubin. This unconjugated bilirubin easily aggregates and precipitates, combining with calcium to form calcium bilirubinate, which promotes the formation of pigment stones.
Physiological Functions of the Bile Ducts
The primary physiological function of the bile ducts is to transport bile to the gallbladder and duodenum, a process coordinated by the gallbladder and the sphincter of Oddi. During fasting, the sphincter of Oddi contracts, increasing pressure within the bile ducts, which directs bile toward the gallbladder for storage and concentration. Following food intake, vagus nerve activation and the presence of fats, proteins, and gastric acid in food stimulate the release of cholecystokinin (CCK) from the duodenum. This leads to gallbladder contraction and sphincter of Oddi relaxation, allowing bile to flow into the duodenum.
Physiological Functions of the Gallbladder
Concentration and Storage of Bile
Although the gallbladder has a capacity of only 30–60 ml, it can accommodate approximately 500 ml of bile over 24 hours. The mucosal lining of the gallbladder has a strong capacity to absorb water and electrolytes, concentrating bile to 5–10 times its original concentration.
Bile Release
Bile secretion is continuous, whereas the discharge of bile is intermittent and occurs in response to feeding. This process is regulated by gallbladder smooth muscle contraction and sphincter of Oddi relaxation, under the influence of neural and humoral factors. The duration of bile release depends on the type and amount of food consumed. CCK is the primary physiological stimulus for gallbladder contraction after meals. Approximately 40 minutes after eating, the gallbladder releases 50%–70% of its contents. By 60–90 minutes, as CCK levels decline, bile begins to be restored and further concentrated in the gallbladder.
Secretory Function
The gallbladder secretes approximately 20 ml of mucus daily. Mucus, primarily composed of mucin, serves to lubricate and protect the gallbladder mucosa. In cases of cystic duct obstruction, bilirubin is reabsorbed from bile, and mucus secretion by the gallbladder mucosa increases. The accumulated fluid in the gallbladder becomes colorless and clear, a condition known as "white bile."