The liver is the largest solid organ in the human body, located primarily in the right hypochondrium, with a portion extending across the midline into the left hypochondrium. The inferior border of the liver aligns with the right costal margin, and the left lower edge can be palpated below the xiphoid process, generally not exceeding the midpoint of the line connecting the xiphoid process and the umbilicus. The superior and anterior surfaces of the liver are anchored to the diaphragm and anterior abdominal wall by the left and right triangular ligaments, coronary ligament, falciform ligament, and round ligament. The visceral surface is connected via the hepatogastric ligament and hepatoduodenal ligament, the latter containing the portal vein, hepatic artery, lymphatic vessels, lymph nodes, and nerves, collectively referred to as the portal pedicle. Within the transverse groove of the liver, the portal vein, hepatic artery, and common hepatic duct each divide into left and right branches as they enter the liver parenchyma, forming the first hepatic hilum. Inside the parenchyma, the courses of the portal vein, hepatic artery, and intrahepatic bile ducts align and are encased within the Glisson capsule.
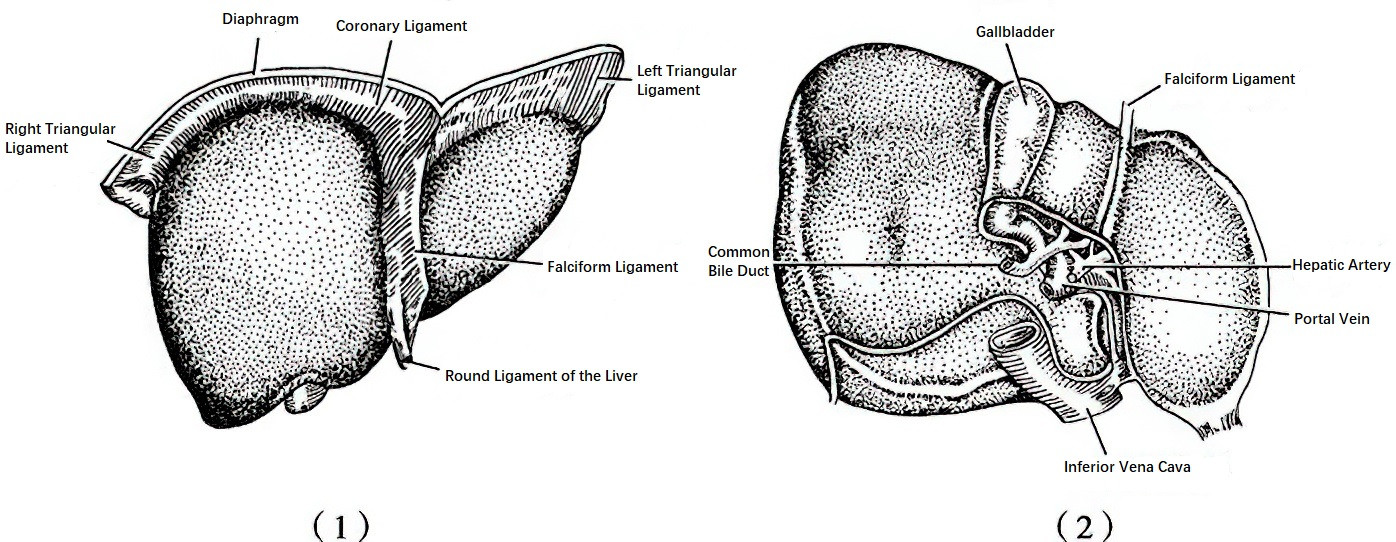
Figure 1 External surface of the liver
1, Diaphragmatic Surface
2, Visceral Surface
Hepatic veins serve as the outflow pathway for blood from the liver. Three major hepatic veins drain into the inferior vena cava through the hepatic venous fossa in the liver's posterior-superior region, which is referred to as the second hepatic hilum. A small portion of hepatic blood flows through short hepatic veins that directly drain into the posterior inferior vena cava, termed the third hepatic hilum.
Based on the distribution patterns of intrahepatic blood vessels and bile ducts, the liver is divided into the left and right lobes. These lobes are further subdivided into the left lateral segment, left medial segment, right anterior segment, right posterior segment, and caudate lobe. The left lateral and right posterior segments are each further divided into superior and inferior portions, while the caudate lobe is subdivided into left and right portions. The Couinaud system, which classifies the liver based on the intrahepatic distribution of the hepatic and portal veins, is widely used and divides the liver into eight segments. The International Hepato-Pancreato-Biliary Association (IHPBA) introduced an alternative nomenclature for liver anatomy and surgery, dividing the liver into three levels: "lobe," "sector," and "segment." Unlike the Couinaud system, which designates the caudate lobe as segment I, this terminology separates it into segments 1 and 9.
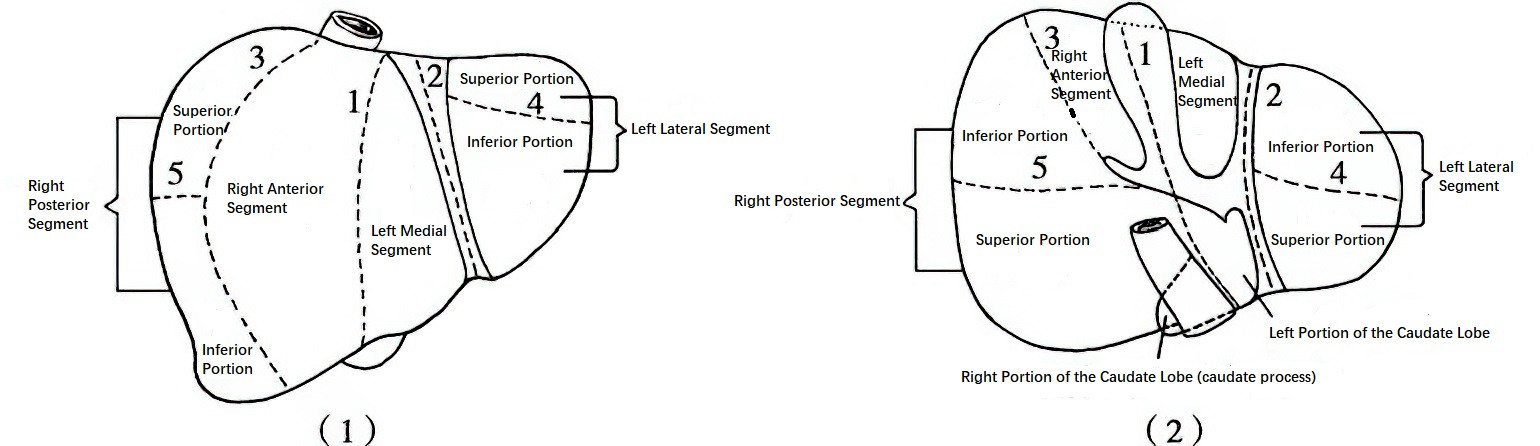
Figure 2 Liver segmentation
(1) Diaphragmatic Surface
(2) Visceral Surface
1, Median Fissure
2, Left Intersegmental Fissure
3, Right Intersegmental Fissure
4, Left Interlobar Fissure
5, Right Interlobar Fissure
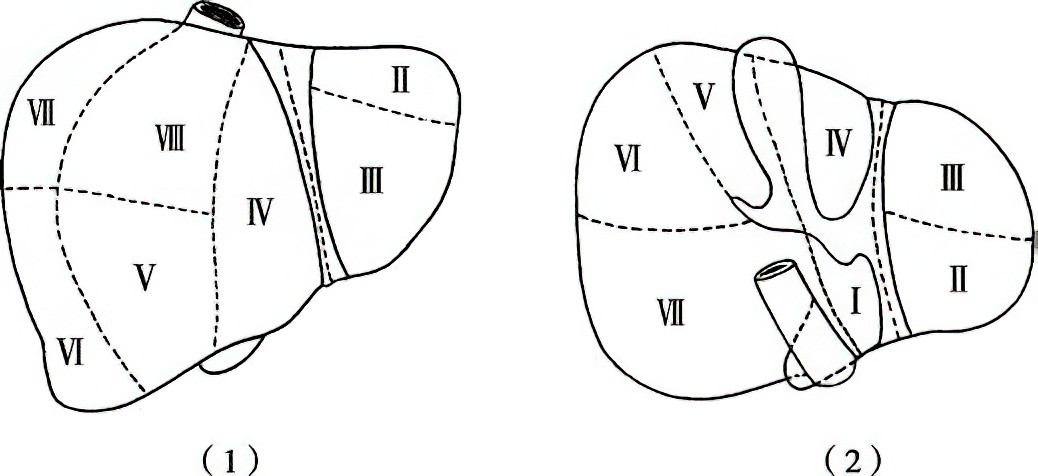
Figure 3 Couinaud segmentation method
1, Diaphragmatic Surface
2, Visceral Surface
The fundamental structural unit of the liver is the hepatic lobule. At its center lies the central vein, surrounded by radially arranged single layers of hepatic cell cords. Between these cords are liver sinusoids (sinusoidal capillaries), whose walls are lined with Kupffer cells, part of the mononuclear phagocyte system. Portal triads, located between adjacent hepatic lobules, consist of branches of the hepatic artery, portal vein, and bile ducts. Liver sinusoids form a capillary network that connects with branches of the hepatic artery and portal vein at one end and the central vein at the other. The surface of hepatocyte membranes along the sinusoids contains numerous microvilli that extend into the space of Disse, facilitating material exchange. Biliary canaliculi are formed by invaginations of adjacent hepatocyte membranes into their cytoplasm, creating microtubules.
The liver receives 25% to 30% of its blood supply from the hepatic artery and 70% to 75% from the portal vein. Despite contributing a smaller volume, the hepatic artery delivers highly oxygenated blood and supplies 40% to 60% of the liver's oxygen requirements. The liver accounts for approximately one-quarter of the cardiac output, with a blood flow rate of up to 1,500 mL/min.
The liver is responsible for critical and complex physiological functions, including:
Bile Secretion
It produces approximately 800–1,000 mL of bile daily, which aids in fat digestion and the absorption of fat-soluble vitamins (A, D, E, K).
Metabolic Functions
Carbohydrate metabolism involves the conversion of carbohydrates absorbed from the intestines into glycogen for storage in the liver. When blood glucose levels decrease, glycogen is broken down into glucose and released into the bloodstream.
Protein metabolism primarily includes synthesis, deamination, and transamination processes. Proteins are digested into amino acids, which are absorbed and used for synthesizing vital proteins, such as albumin, fibrinogen, and prothrombin. Severe liver damage can lead to hypoalbuminemia and coagulation disorders. The liver converts most ammonia generated during metabolism into urea, which is excreted by the kidneys. Impaired deamination due to severe liver cell damage can result in elevated blood ammonia levels, a primary cause of hepatic encephalopathy. Transaminases within hepatocytes facilitate the interconversion of amino acids. When hepatocytes are damaged and their membranes disrupted, transaminases are released into the bloodstream, leading to elevated serum levels.
Lipid metabolism involves regulating and maintaining the concentrations and proportions of various lipids, including phospholipids and cholesterol, in the body.
The liver is also involved in vitamin metabolism. Beta-carotene is converted into vitamin A and stored in the liver, which also stores B-complex vitamins, as well as vitamins C, D, E, and K.
In hormone metabolism, the liver deactivates hormones such as estrogen and antidiuretic hormones. It plays a central role in the intermediate metabolism of corticosteroids and aldosterone. In cirrhosis, the liver's ability to deactivate these hormones diminishes, leading to increased estrogen levels that manifest as spider angiomas, palmar erythema, and gynecomastia in males. Increased levels of antidiuretic hormone and aldosterone contribute to water and sodium retention, resulting in edema and ascites formation.
Coagulation Function
The liver synthesizes fibrinogen and prothrombin and produces coagulation factors V, VII, VIII, IX, X, XI, and XII. Additionally, vitamin K stored in the liver is essential for the synthesis of prothrombin and coagulation factors VII, IX, and X.
Detoxification
Endogenous or exogenous toxins are processed in the liver through the mononuclear phagocyte system, where they are phagocytosed or metabolized into non-toxic substances through mechanisms such as degradation, oxidation, and conjugation.
Phagocytic and Immune Functions
The liver removes bacteria, antigen-antibody complexes, pigments, and other debris from the bloodstream through the phagocytic activity of Kupffer cells.
Other Functions
The liver contains hematopoietic factors such as iron, copper, vitamin B12, and folic acid, enabling it to indirectly participate in hematopoiesis. The liver also serves as a reservoir of blood, playing a role in regulating blood circulation during acute blood loss.
The liver exhibits significant functional reserve and regeneration capacity. Studies have shown that normal physiological functions can be maintained even after 70%–80% of healthy liver parenchyma is resected, with regeneration occurring to nearly restore the liver to its original weight over time. As a result, segmental, lobar, or even more extensive resections (such as the right three lobes) can be performed for localized lesions.
However, the liver is highly sensitive to hypoxia. Although a normal liver can tolerate continuous hepatic pedicle clamping at normal temperatures for approximately 60 minutes, this tolerance is markedly reduced in patients with liver cirrhosis. For such patients, the duration of a single warm ischemia event during pedicle clamping should be limited to 15–20 minutes during liver resection.