Anatomy of the Stomach
Position and Regions of the Stomach
The stomach is located in the upper abdomen, between the esophagus and the duodenum. The junction between the stomach and the esophagus is referred to as the cardia, while the junction between the stomach and the duodenum is called the pylorus; both are controlled by sphincters that regulate the flow of contents. The right side of the stomach between the cardia and pylorus is called the lesser curvature, while the left side is referred to as the greater curvature. A line dividing the stomach into three equal sections between the lesser and greater curvatures categorizes it into three regions from top to bottom: the cardia and fundus region, the body region, and the pyloric region. The circular muscles in the pyloric region are thickened, forming a circular groove visible on the serosal surface. The gastric vein marks the surface and helps distinguish between the pylorus and the duodenum.
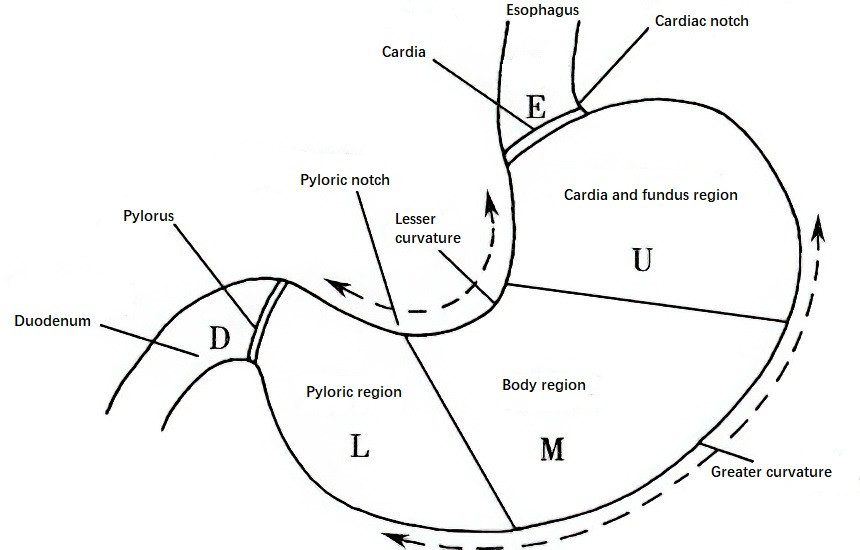
Figure 1 Anatomical regions of the stomach
Gastric Ligaments
The stomach is anchored in the upper abdomen by ligaments connecting it to surrounding organs, including the gastrophrenic ligament, hepatogastric ligament, gastrosplenic ligament, gastrocolic ligament, and the gastro-pancreatic ligament.
Gastric Blood Supply
Arterial blood supply to the stomach is derived from the celiac artery and its branches. The left gastric artery originates from the trunk of the celiac artery, and the right gastric artery branches from the proper hepatic artery. These two arteries form an arterial arch along the lesser curvature. The right gastro-omental artery from the gastroduodenal artery and the left gastro-omental artery from the splenic artery form a vascular arch for the greater curvature. Additional short gastric arteries and 1–2 posterior gastric arteries arising from the splenic artery supply the gastric fundus and the proximal stomach. Venous drainage includes the left gastric vein (also known as the coronary vein), which drains into the portal vein or the splenic vein; and the right gastric vein, which drains into the portal vein. The right gastro-omental vein drains into the superior mesenteric vein via the gastrocolic trunk, while the left gastro-omental and short gastric veins drain into the splenic vein.
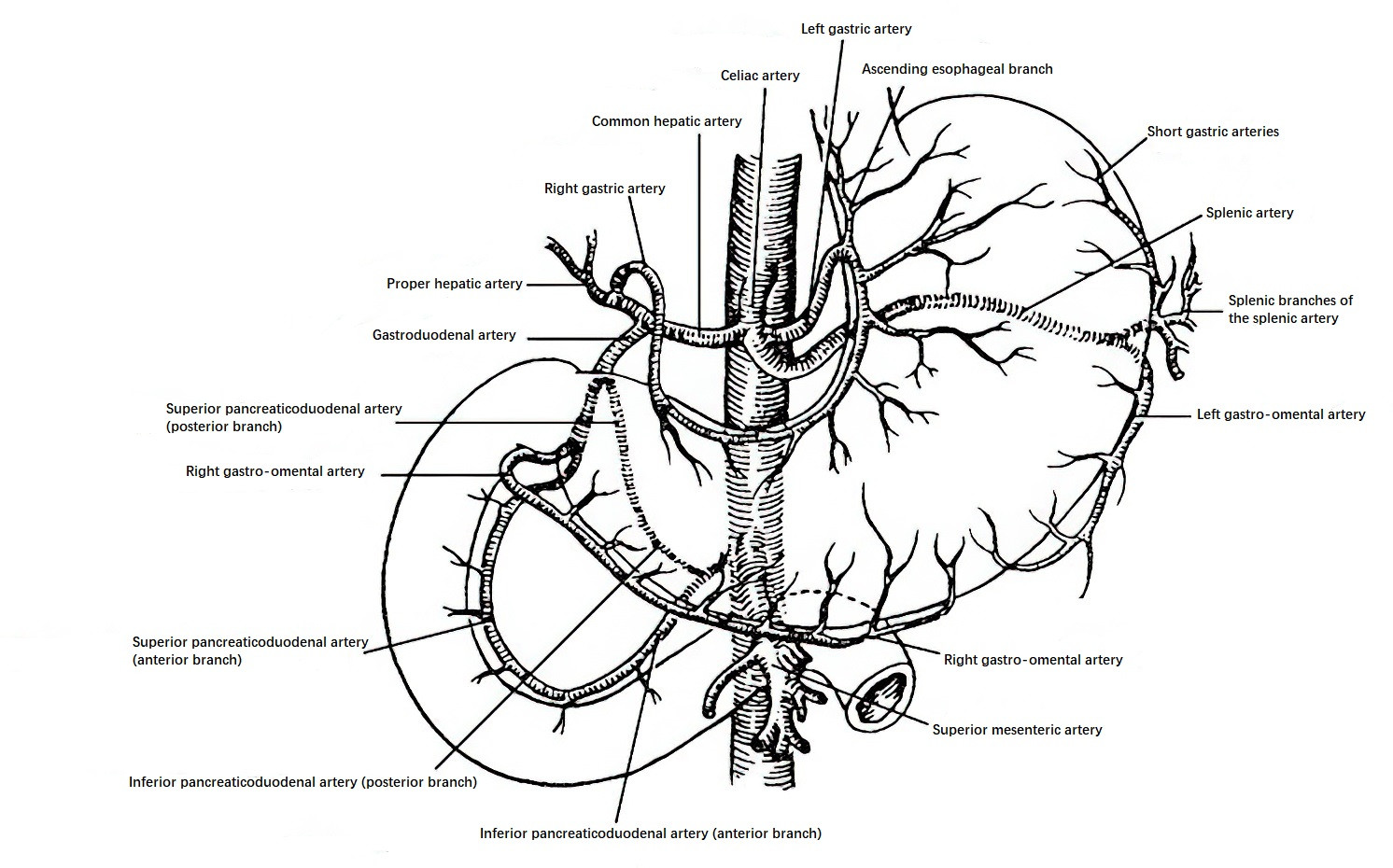
Figure 2 Blood supply of the stomach and duodenum
Gastric Lymphatic Drainage
The stomach has a dense submucosal lymphatic network, which connects to the esophageal lymphatic network proximally and the duodenal lymphatic network distally. Lymphatic drainage follows the course of the gastric arteries in reverse direction. Sixteen groups of regional lymph nodes are categorized into four main groups:
- Celiac lymph nodes: Drain the upper portion of the lesser curvature.
- Superior pyloric lymph nodes: Drain the lower portion of the lesser curvature.
- Inferior pyloric lymph nodes: Drain the lower portion of the greater curvature.
- Pancreatic-splenic lymph nodes: Drain the upper portion of the greater curvature.
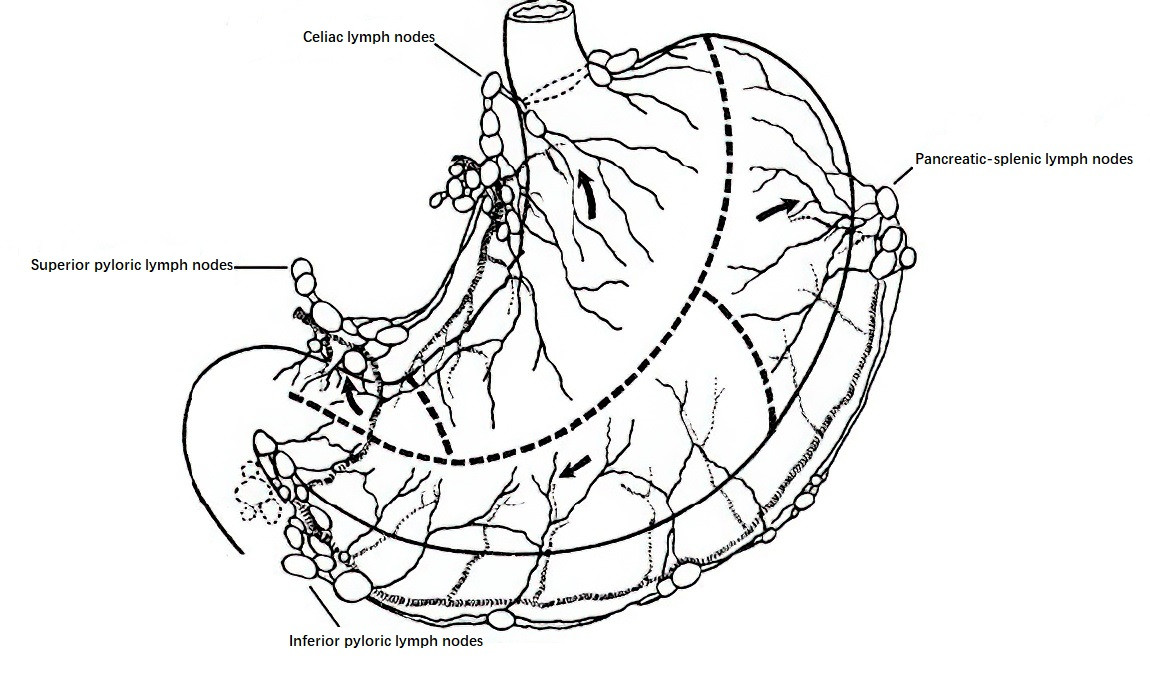
Figure 3 Lymphatic drainage of the stomach
Gastric Innervation
The stomach receives dual autonomic and central nervous system control. The central nervous system influences the stomach via the autonomic nervous system, with its sympathetic and parasympathetic components. Intrinsic autonomic nerves of the stomach, referred to as the "gut brain," include the submucosal plexus (Meissner's plexus) located within the submucosa, and the myenteric plexus (Auerbach's plexus) situated between the circular and longitudinal muscle layers. Gastric motility and secretion are primarily regulated by the sympathetic and parasympathetic nerves. Sympathetic nerves, derived from postganglionic fibers of the celiac plexus, inhibit gastric motility and secretion, whereas parasympathetic nerves, originating from the vagus nerve, stimulate these functions. The left and right vagus nerves descend along the right side of the esophagus, with the left branch giving rise to hepatic and anterior gastric branches (Latarjet’s anterior nerve branch) at the ventral side of the cardia, and the right branch giving rise to celiac and posterior gastric branches (Latarjet’s posterior nerve branch) at the dorsal side of the cardia. The anterior and posterior branches descend along the lesser curvature and send off branches to the anterior and posterior gastric walls. Near the gastric antrum, the final 3–4 terminal branches innervate the antrum in a "crow’s foot"-shaped distribution, regulating antral motility and pyloric emptying.
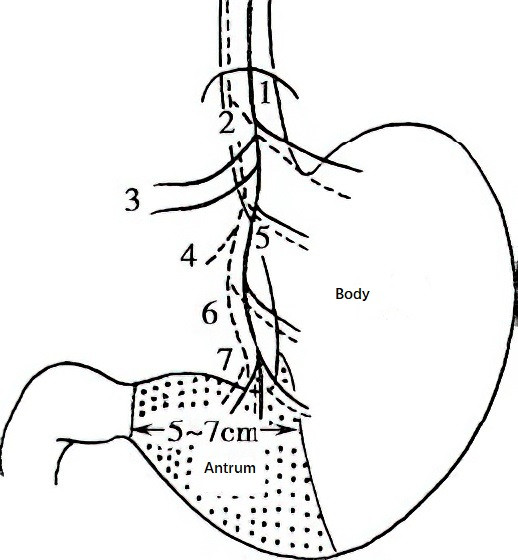
Figure 4 Vagus nerves of the stomach
1, Left vagus nerve
2, Right vagus nerve
3, Hepatic branch
4, Celiac branch
5, Anterior gastric branch (Latarjet anterior nerve)
6, Posterior gastric branch (Latarjet posterior nerve)
7, "Crow's foot"
Gastric Wall Structure
The gastric wall consists of four layers, listed from the outermost to the innermost: the serosal layer, muscular layer, submucosa, and mucosa. The muscular layer is made of smooth muscle and includes an outer longitudinal layer and an inner circular layer. The circular muscle layer thickens at the cardia and pylorus to form the cardiac and pyloric sphincters, respectively. The submucosal structure is loose, rich in blood vessels, lymphatic vessels, and nerve plexuses, and serves as the operational plane for submucosal dissection and surgical mucosal stripping.
The mucosa includes an epithelial layer, lamina propria, and muscularis mucosae. The mucosal glands, which are primarily distributed in the gastric fundus and the body, consist of various secretory cells such as:
- Parietal cells: Aid in acid secretion.
- Chief cells: Responsible for enzyme production.
- Mucous cells: Secrete mucus.
The cardiac glands, located in the cardia, mainly produce mucus, while the pyloric glands, located in the antrum and pyloric region, contain chief cells and specialized endocrine cells, including:
- G cells: Secrete gastrin.
- D cells: Secrete somatostatin.
- Argentaffin cells and other endocrine cells: Secrete histamine, serotonin, and various peptide hormones.
Physiology of the Stomach
The stomach's primary functions include motility and secretion.
Gastric Motility
Gastric motility encompasses accommodation, grinding, and gastric emptying. When food enters the stomach, receptive relaxation occurs mainly in the proximal stomach, including the gastric fundus and body, allowing for the accommodation of food without a significant rise in intragastric pressure. While the fasting stomach typically accommodates around 50 mL, its capacity may expand up to 1,000 mL during receptive relaxation without causing a notable increase in pressure. When the proximal stomach contracts, food is pushed into the antrum, where it mixes with gastric juice and undergoes grinding until the chyme particle size is reduced to approximately 1 mm. At this point, the pyloric sphincter opens, allowing 2–10 mL of chyme to flow into the duodenum. This cycle repeats until the stomach is emptied. Gastric emptying rates are influenced by the properties and quantity of the ingested food, as well as neural and hormonal regulation.
Gastric smooth muscle contraction is mediated by gastric electrical activity. Two primary waveforms are recognized:
- Slow waves: These occur at a frequency of approximately 3 cycles per minute and originate from a "pacemaker" region located at the junction of the upper and middle-thirds of the greater curvature.
- Spikes (Fast Waves): These are periodic electrical patterns superimposed on slow waves. They migrate distally as part of the migrating myoelectric complex (MMC), a motor pattern that persists even in the absence of central nervous regulation. The MMC cycle occurs every 90–120 minutes during fasting.
Gastric Secretion
A normal adult secretes 1,500–2,500 mL of gastric juice per day. Gastric juice primarily consists of hydrochloric acid, enzymes, mucus, electrolytes, and water. Hydrochloric acid is secreted by parietal cells, whereas non-parietal cells secrete a slightly alkaline fluid, with sodium ions being the predominant cation.
Gastric secretion can be categorized into basal secretion during the interdigestive phase and postprandial secretion during the digestive phase.
Basal Secretion
This type of secretion occurs naturally without food stimulation and has a low output.
Postprandial Secretion
This has three distinct phases:
- Cephalic phase: Initiated by sensory stimuli such as sight, taste, and smell, this phase activates the central nervous system, and efferent signals travel via the vagus nerve to stimulate parietal cells, chief cells, and mucus cells in the stomach to secrete gastric acid, pepsin, and mucus. The vagus nerve also activates G cells and other endocrine cells to release gastrin and histamine, which further enhance acid secretion. This phase is short and produces 20–30% of the total gastric secretion.
- Gastric phase: In this phase, physical distension of the stomach and chemical stimulation from food interacting with the gastric mucosa trigger both vagovagal reflexes and cholinergic reflexes, leading to gastric secretion. Gastrin secretion by G cells plays a dominant role in acid production during this phase. However, when the pH in the antrum falls below 2.5, gastrin release is inhibited, and it ceases entirely when the pH drops below 1.2.
- Intestinal phase: This phase begins when chyme enters the small intestine, stimulating the duodenum and proximal jejunum to release enteric gastrin, which weakly promotes gastric secretion. This phase accounts for 5–10% of the overall gastric secretion.
Anatomy and Physiology of the Duodenum
The duodenum, approximately 25 cm in length, serves as the connection between the stomach and jejunum. It originates at the pylorus and terminates at the ligament of Treitz, forming a C-shaped loop around the pancreatic head. It is the most fixed portion of the small intestine and can be divided into four parts:
- The Superior Part (Duodenal Bulb): Measuring about 4–5 cm, this intraperitoneal segment is a common site for duodenal ulcers.
- The Descending Part: Measuring about 7–9 cm, this retroperitoneal segment is fixed in position. Approximately 8–10 cm distal to the pylorus lies the major duodenal papilla, where the common bile duct and pancreatic duct open. This anatomical feature serves as a key landmark for locating these ducts.
- The Horizontal Part: About 10 cm long, this segment runs transversely to the left and is retroperitoneal. The superior mesenteric artery and vein cross anteriorly. A sharp downward angle of the superior mesenteric artery can compress this segment, leading to obstruction, a condition known as "superior mesenteric artery syndrome."
- The Ascending Part: Measuring approximately 3–5 cm, this segment ascends before sharply turning inferiorly and anteriorly to connect with the jejunum at its starting point. It is anchored to the retroperitoneum by the ligament of Treitz, marking the boundary between the duodenum and jejunum.
Blood supply to the duodenum is provided by the superior and inferior pancreaticoduodenal arteries. Bile and pancreatic secretions enter the duodenum through its papilla. Digestive enzymes secreted by Brunner's glands in the duodenal mucosa, including proteases, lipases, and sucrase, mix with the luminal contents to facilitate food breakdown. Endocrine cells in the duodenal mucosa secrete hormones such as gastrin, cholecystokinin, and secretin to regulate digestion and other gastrointestinal processes.