The patient is assessed in either the supine or sitting position, with both breasts fully exposed.
Visual Inspection
In a well-lit environment, the appearance, shape, and size of both breasts are observed for symmetry. The level and condition of the nipples are evaluated for any retraction, inversion, or discharge. Any localized swelling, indentations, redness, swelling, ulceration, "orange peel" skin changes, dimpling, or prominent veins are noted on the breast skin.
Palpation
Using the palmar surface of the fingers, a systematic examination of all four quadrants of the breast (upper outer quadrant including the axillary tail, upper inner quadrant, lower outer quadrant, lower inner quadrant) and the central area is performed. The examination begins on the healthy side, followed by the affected side.
When a breast mass is identified, attention is given to its location, size, consistency, surface smoothness, margin clarity, and mobility. Gentle pinching of the skin over the mass determines whether it is adherent to the overlying skin. Benign tumors typically have well-defined margins, are more mobile, and possess a smooth surface. Malignant tumors tend to have poorly defined borders, are firm, have an irregular surface, limited mobility, and may adhere to the skin. For larger masses, the relationship of the mass to the deeper tissues is assessed. The patient may be instructed to place their hands on their hips and tense the chest muscles. Limited mobility of the mass in this position suggests invasion of deeper tissues by the tumor. Lastly, the nipple is gently squeezed to check for any discharge. If discharge is present, the areas around the areola are systematically pressed to locate the specific duct from which the discharge originates, which can be marked accordingly.
Axillary Lymph Node Examination
The sitting position is preferred for axillary lymph node examination. While facing the patient, the examiner uses their right hand to examine the patient's left axilla and their left hand for the patient's right axilla. The patient is asked to abduct their arm, and the examiner’s fingers are inserted into the apex of the axilla, pressing against the chest wall. The patient is then instructed to relax their arm, resting it on the examiner's forearm. A gentle, top-to-bottom movement is used to palpate the axillary apex lymph nodes. Next, the examiner’s fingers palpate the lymph nodes behind the anterior axillary fold (deep to the pectoralis major muscle). Standing behind the patient, the examiner assesses the lymph nodes along the anteromedial edge of the latissimus dorsi muscle. The subclavian and supraclavicular lymph nodes are examined last. When enlarged lymph nodes are detected, their size, texture, tenderness, fusion, and mobility are evaluated.
Imaging Studies
Ultrasound
Ultrasound is unaffected by breast density and provides high sensitivity in distinguishing cystic from solid lesions. Doppler ultrasound and elastography can further provide valuable information about blood flow and stiffness of the lesion.
Mammography
Mammography is a commonly used imaging technique and highly sensitive for detecting microcalcifications. It is widely employed for breast cancer screening. Breast cancer often manifests on mammography as a high-density mass with irregular borders or spiculated features.
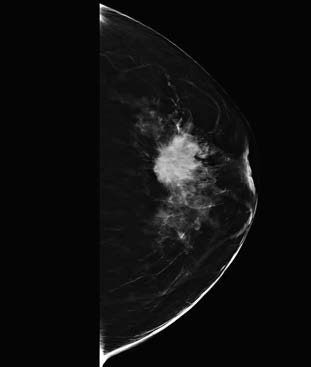
Figure 1 Mammography showing a spiculated mass lesion
Magnetic Resonance Imaging (MRI)
MRI offers high soft tissue resolution and greater sensitivity than mammography and ultrasound in detecting lesions. It is particularly advantageous for identifying small lesions, multicentric, or multifocal disease and for assessing the full extent of involvement. Breast cancer appears on T1-weighted imaging after contrast enhancement as a lesion with irregular margins and significant enhancement.
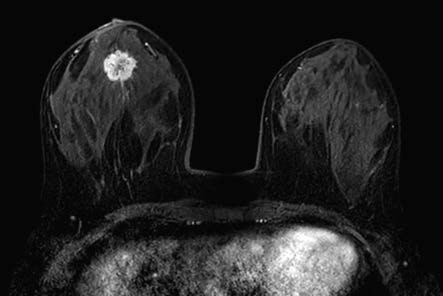
Figure 2 Breast magnetic resonance imaging (MRI)
Histopathological Biopsy
Common biopsy techniques include core needle biopsy, vacuum-assisted breast biopsy, and fine-needle aspiration biopsy. The first two methods have a diagnostic accuracy of 90% to 97%, while fine-needle aspiration biopsy has a diagnostic rate of 70% to 90%.
If there is suspicion of breast cancer and the above methods fail to provide a definitive diagnosis, surgical excision of the mass along with surrounding tissue for intraoperative frozen section pathology is recommended. Incisional biopsy is generally not preferred.
For patients with nipple discharge, ductoscopy or cytological examination of nipple discharge smears may be performed. In cases of nipple erosion suspected to be Paget’s disease of the breast, cytological examination of scrapings or imprint smears, or excisional biopsy of the eroded nipple area, may be conducted.