The thyroid gland is the largest endocrine gland in the human body. It consists of two lateral lobes (left and right) and an isthmus, with the isthmus sometimes connected to the hyoid bone by a pyramidal lobe. The lateral lobes are located on either side of the larynx and trachea, with their lower poles often between the fifth and sixth tracheal cartilages. The isthmus is typically situated anterior to the second to fourth tracheal cartilages. On the posterior aspect of the lateral lobes lie the parathyroid glands, and the thyroid is medially adjacent to the larynx, pharynx, and esophagus.
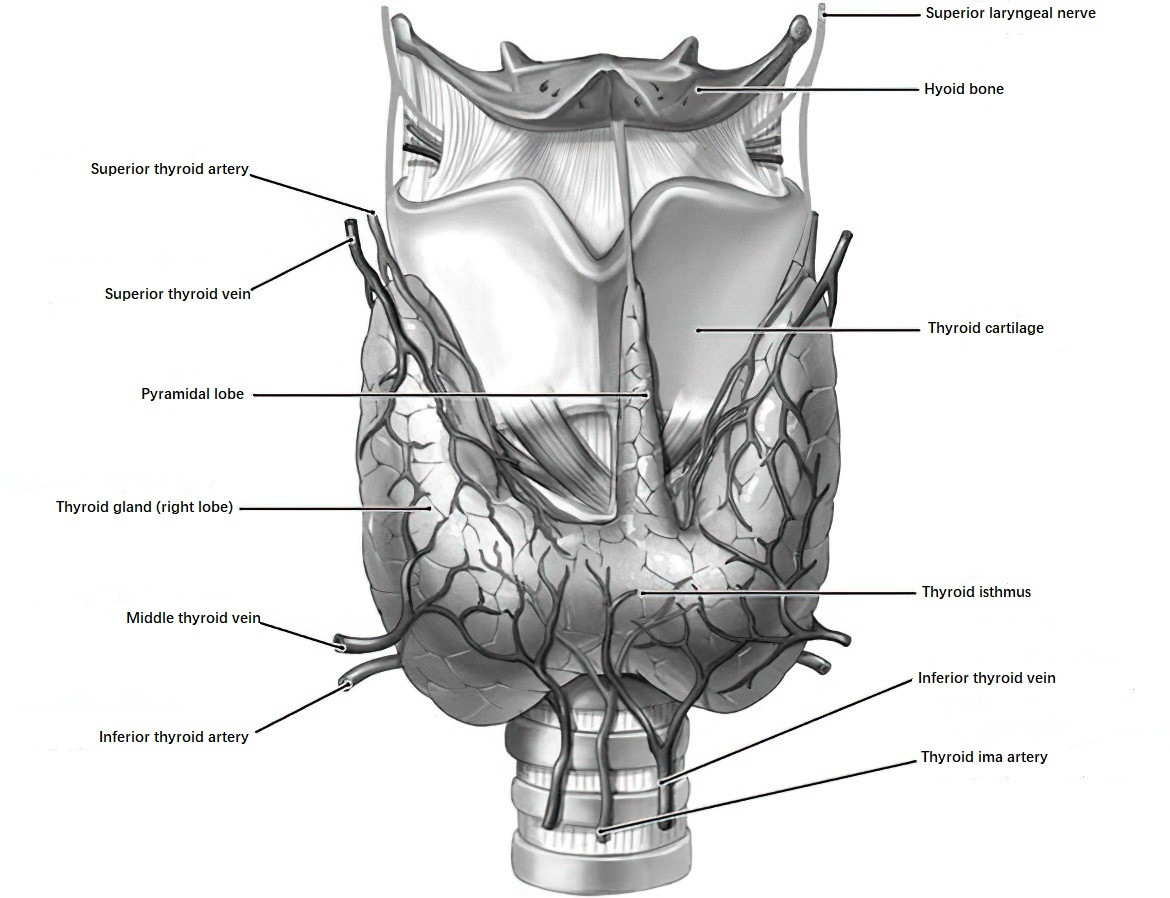
Figure 1 Anterior view of the thyroid gland
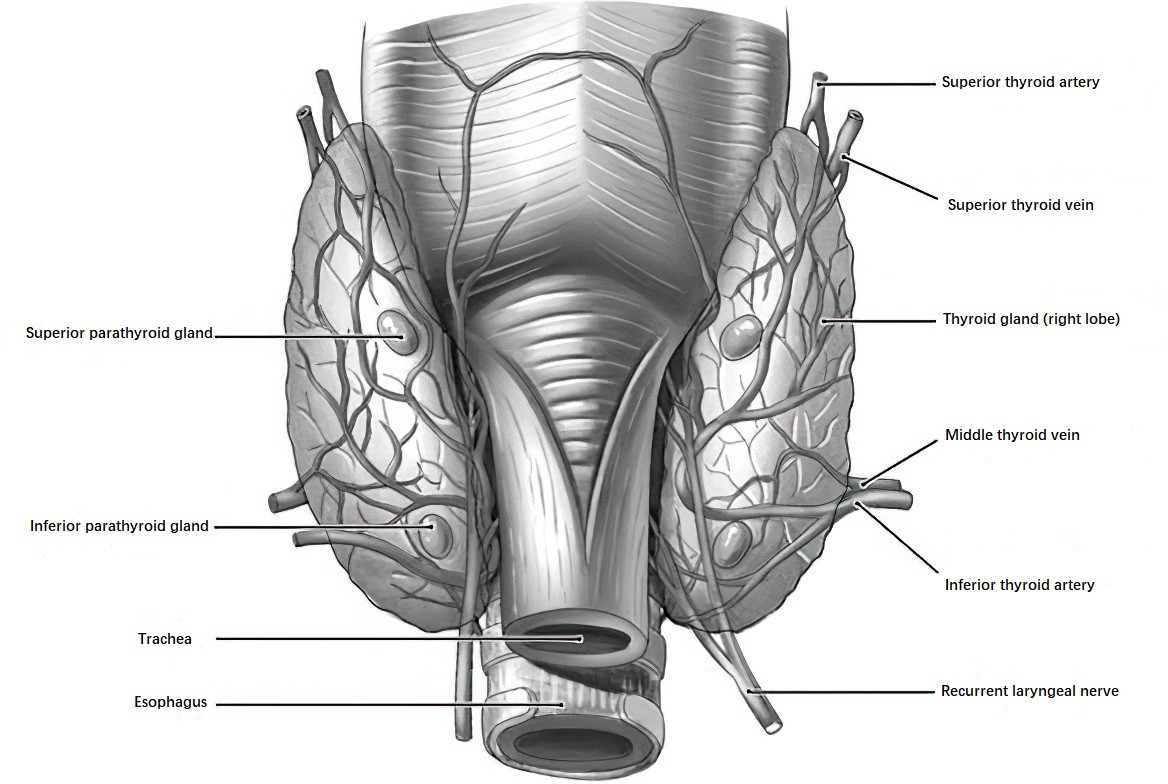
Figure 2 Posterior view of the thyroid gland
The thyroid is encapsulated by two layers: an inner and an outer capsule. The inner layer, known as the true capsule, is thin and tightly adheres to the gland. The outer capsule, a continuation of the pretracheal fascia, surrounds and secures the thyroid to the trachea and cricoid cartilage, and is also referred to as the surgical capsule. Between these two layers lies loose connective tissue containing the parathyroid glands and the recurrent laryngeal nerve. During thyroid surgery, dissection occurs in this plane, adhering closely to the true capsule to preserve the parathyroid glands and the recurrent laryngeal nerve.
The thyroid gland has an abundant blood supply, primarily from the superior thyroid artery (a branch of the external carotid artery) and the inferior thyroid artery (a branch of the thyrocervical trunk). In fewer than 5% of individuals, a thyroid ima artery may also be present. Extensive anastomoses exist between branches of the superior and inferior thyroid arteries, as well as between these and branches of the arteries supplying the pharynx, larynx, trachea, and esophagus. This network ensures that even if both the superior and inferior thyroid arteries are ligated during surgery, the remaining thyroid tissue continues to receive blood supply. Venous drainage from the thyroid gland occurs through an extensive capillary network that drains into the superior, middle, and inferior thyroid veins. The superior and middle veins drain into the internal jugular vein, while the inferior vein typically drains into the brachiocephalic vein.
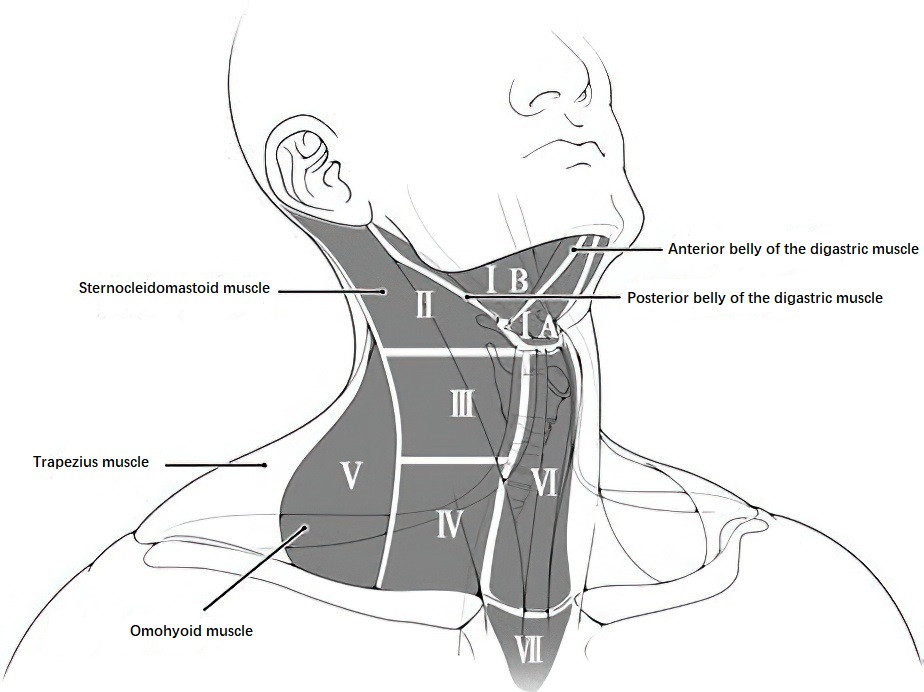
Figure 3 Cervical lymph node levels
The thyroid gland is also highly enriched with lymphatic vessels, which converge toward the true capsule, forming collection ducts. These ducts either follow or bypass the peripheral veins, draining into cervical lymph nodes. The cervical lymph nodes are anatomically divided into seven levels:
- Level I: Submental (IA) and submandibular (IB) lymph nodes. IA is confined by the anterior bellies of the digastric muscles and the hyoid bone, while IB is bounded by the anterior and posterior bellies of the digastric muscles and the inferior border of the mandible.
- Level II: Upper internal jugular lymph nodes, extending from the posterior belly of the digastric muscle to the lower border of the hyoid bone.
- Level III: Middle internal jugular lymph nodes, spanning from the lower border of the hyoid bone to the lower border of the cricoid cartilage.
- Level IV: Lower internal jugular lymph nodes, located between the lower border of the cricoid cartilage and the clavicle.
- Level V: Posterior triangle lymph nodes, with anterior, posterior, and inferior boundaries formed by the posterior border of the sternocleidomastoid muscle, the anterior border of the trapezius muscle, and the clavicle, respectively.
- Level VI (Central Zone): Lymph nodes located in the anterior neck, including prelaryngeal, pretracheal, paratracheal, and nodes in the tracheoesophageal groove. The boundaries are the hyoid bone superiorly, the suprasternal notch inferiorly, and the medial borders of the common carotid arteries laterally.
- Level VII: Represents an inferior extension of Level VI, ranging from the suprasternal notch to the upper margin of the brachiocephalic artery.
The recurrent laryngeal nerve, originating from the vagus nerve, travels within the tracheoesophageal groove and often passes between branches of the inferior thyroid artery, innervating the vocal cords for motor function. The superior laryngeal nerve, also arising from the vagus nerve, has an internal branch providing sensory innervation to the mucosa of the larynx above the glottis, and an external branch that innervates the cricothyroid muscle to tense the vocal cords.
The primary function of the thyroid gland is the synthesis, storage, and secretion of thyroid hormones. These hormones play significant roles in accelerating tissue oxidation, heat production, and promoting growth and development. Regulatory mechanisms include the hypothalamic-pituitary-thyroid axis as well as intrinsic autoregulatory processes within the thyroid gland.