The preoperative preparation of a patient is closely related to the severity of the disease and the scope of the surgery. Surgical procedures can be categorized into three types based on their urgency:
Emergency Operations
These include procedures such as surgery for traumatic intestinal rupture, which are performed immediately after minimal necessary preparation. In extremely critical situations, such as rupture and bleeding of large blood vessels in the chest or abdomen, surgery is performed urgently to save the patient's life without delay.
Confined Operations
These involve procedures such as radical surgeries for malignant tumors. Although the timing of surgery is flexible, it should not be delayed for long. Preoperative preparation should be completed in the shortest time possible.
Elective Operations
These include procedures such as cholecystectomy for gallstones, thyroid adenoma excision, and inguinal hernia repair, which can be performed at an appropriate and carefully chosen time after adequate preoperative preparation.
A thorough understanding of the patient's general condition before surgery is necessary. This assessment includes their psychological and nutritional status, as well as the functioning of critical systems such as the heart, lungs, liver, kidneys, endocrine system, hematological system, and immune system. A detailed medical history, comprehensive physical examination, and routine laboratory tests, along with specific evaluations for the function of vital organs, are required to provide a detailed assessment of the patient's surgical tolerance.
General Preparation
General preparation includes both psychological and physiological aspects.
Psychological Preparation
Patients often experience fear, tension, and anxiety before surgery. Healthcare professionals provide adequate care and encouragement, explaining the patient's condition, the necessity of the surgery, the expected outcomes, potential perioperative complications, recovery processes, and prognosis in detail. These efforts help patients and their families approach the perioperative treatment with a positive attitude. Informed consent is obtained, and the necessary documentation is signed, including the surgical informed consent form, anesthesia consent form, and blood transfusion consent form. In life-saving emergency surgeries, if the patient’s relatives cannot arrive at the hospital to sign the consent forms, the situation must be documented in the patient’s medical record.
Physiological Preparation
Adjustments to the patient’s physiological state are made to ensure they are in the best possible condition to safely undergo surgery and postoperative care.
Preoperative Adaptive Exercises
Patients practice activities such as urination and defecation in bed before surgery and are trained in proper coughing and sputum expectoration techniques. Patients with a history of smoking or alcohol consumption are advised to quit smoking and drinking at least four weeks before surgery.
Blood Transfusion and Fluid Replacement
For medium to large surgical procedures, blood typing and cross-matching are performed, and an adequate supply of blood products is prepared. Patients with imbalances in water, electrolytes, or acid-base levels, as well as those with anemia or hypoproteinemia, require correction before the surgery.
Infection Prevention
Identified foci of infection, such as dental caries, are treated before surgery, and patients avoid contact with individuals who have infectious conditions. Prophylactic antibiotic use is necessary in the following situations:
- Procedures involving infectious sites or incisions near areas of infection.
- Gastrointestinal surgeries.
- Surgeries with prolonged duration or significant trauma.
- Open wounds with contaminated surfaces, extensive soft tissue damage, prolonged intervals between injury and debridement, or those requiring extensive and incomplete debridement.
- Surgeries for malignant tumors.
- Surgeries involving major blood vessels.
- Surgeries that require the implantation of artificial devices.
- Organ transplantation surgeries.
The method of administration for prophylactic antibiotics requires completion of infusion 30–60 minutes before skin incision. A second dose may be administered intraoperatively if the surgery lasts more than three hours or the intraoperative blood loss exceeds 1,500 mL. The duration of prophylactic antibiotic use generally does not exceed 24 hours, but in specific cases, it may be extended to 48 hours.
Gastrointestinal Preparation
This can be seen in the "Gastrointestinal Preparation" section under "Pre-Anesthesia Assessment and Preparation."
Other Measures
The night before surgery, patients may be given sedatives to ensure adequate sleep. If unrelated issues arise, such as an unexplained fever or menstrual onset in female patients, the surgery date may need to be postponed. Before entering the operating room, the patient’s bladder needs to be emptied. If surgery is expected to last a long time or involves the pelvis, a urinary catheter should be inserted. Patients with removable dentures should remove them preoperatively to prevent accidental swallowing or aspiration during anesthesia or surgery.
Specialized Preparation
In addition to general preoperative preparation, specific measures should be taken based on the patient's condition.
Malnutrition
Preoperative malnutrition is a significant risk factor for increased postoperative complications and mortality. Assessing and correcting preoperative malnutrition is an essential step during the surgical perioperative period. Nutritional assessment includes the patient’s medical history, physical examination, and special attention to weight changes since disease onset. A weight loss of more than 20% due to illness is associated with a higher mortality rate and a threefold increase in postoperative infection rates. Laboratory indicators such as serum albumin, transferrin, and prealbumin levels can evaluate nutritional status. Patients with severe malnutrition require nutritional support prior to surgery, and surgery should be performed after their nutritional status improves.
Cerebrovascular Disease
Perioperative stroke is uncommon (with an incidence of less than 1%, or about 2–5% in cardiac surgeries), with 80% of cases occurring postoperatively. Most cases are caused by hypotension or cardiogenic embolism associated with atrial fibrillation. Risk factors include advanced age, hypertension, coronary artery disease, diabetes, and smoking. Patients with asymptomatic carotid bruits or recent transient ischemic attacks should undergo further evaluation and treatment. For patients with a recent history of stroke, elective surgeries should be delayed by at least two weeks, preferably six weeks.
Cardiovascular Disease
Patients with hypertension should continue their antihypertensive medications, with resting blood pressure controlled to below 140/90 mmHg. For non-emergency surgeries, patients with excessively high blood pressure (above 180/100 mmHg) need preoperative antihypertensive treatment to stabilize blood pressure. For hypertensive patients experiencing sudden blood pressure spikes after entering the operating room, anesthesiologists and surgeons work together to decide whether to proceed or postpone the surgery.
Patients with cardiac diseases face significantly higher mortality rates during surgery compared to those without cardiac conditions. A multidisciplinary approach involving surgeons, anesthesiologists, and cardiologists is necessary to assess and manage cardiac risk factors. The Goldman Cardiac Risk Index is commonly used to quantify the risk of perioperative cardiac mortality and life-threatening complications. For patients aged ≥40 undergoing non-cardiac surgery, the risk of cardiac death and major complications increases with higher scores:
- 0–5 points: Risk < 1%.
- 6–12 points: Risk 7%.
- 13–25 points: Risk 13% (mortality 2%).
- ≥26 points: Risk 78% (mortality 56%).
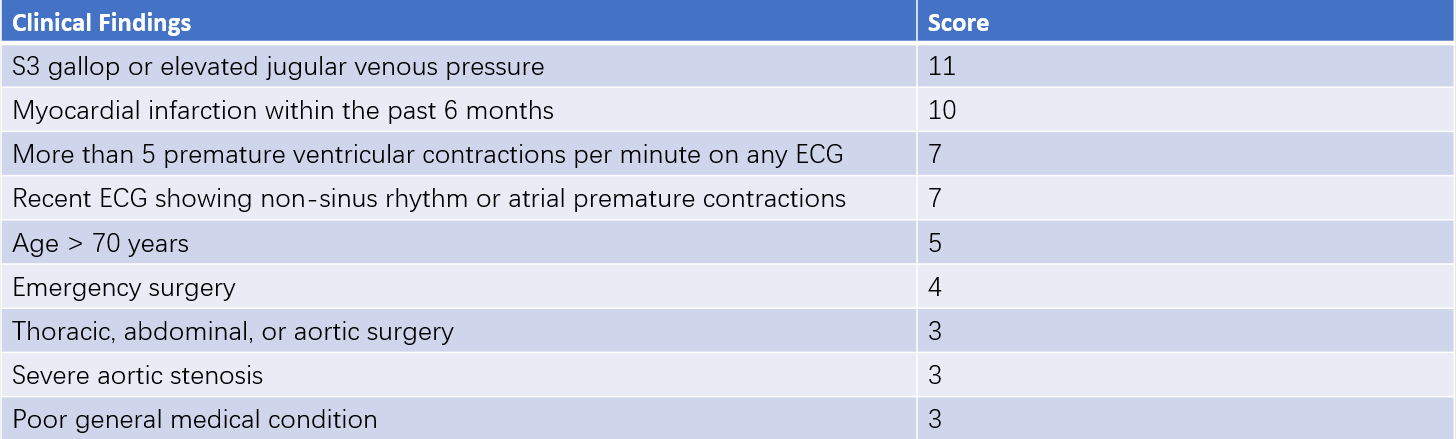
Table 1 Goldman index
The advantage of the Goldman Index is that over half of its scoring factors are modifiable. For instance, resolving congestive heart failure reduces the score by 11 points, while delaying surgery after myocardial infarction reduces the score by 10 points.
Pulmonary Dysfunction
Pulmonary complications are the second-leading cause of postoperative morbidity and mortality, after cardiovascular complications. For patients with a history of pulmonary disease or those undergoing surgeries such as pulmonary resection, esophageal tumor excision, or mediastinal tumor surgery, preoperative pulmonary function evaluation is particularly important. Risk factors include chronic obstructive pulmonary disease (COPD), smoking, advanced age, obesity, and acute respiratory infections. Chest imaging can help differentiate between pulmonary parenchymal disease and pleural abnormalities. Polycythemia may indicate chronic hypoxemia; if arterial partial pressure of oxygen (PaO2) is below 60 mmHg or partial pressure of carbon dioxide (PaCO2) exceeds 45 mmHg, the risk of perioperative pulmonary complications increases.
Preoperative pulmonary function tests are important for high-risk patients. A forced expiratory volume in 1 second (FEV1) below 2 liters may indicate dyspnea; an FEV1/forced vital capacity (FVC) ratio below 50% suggests severe pulmonary dysfunction and potential need for postoperative mechanical ventilation and specialized monitoring. Preoperative respiratory training improves pulmonary function and reduces complications.
Smoking cessation before surgery is critical. Within 1–2 weeks, mucosal ciliary function is restored, and sputum production decreases; cessation for six weeks improves lung capacity. Respiratory training increases functional residual capacity and reduces pulmonary complications. Elective surgeries for patients with acute respiratory infections are postponed until one or two weeks after recovery. For emergency procedures, respiratory infections must be actively treated. Bronchodilators are used perioperatively for patients with obstructive airway diseases. Elective surgeries are delayed during acute asthma exacerbations.
Renal Disease
Anesthesia and surgical trauma place additional stress on renal function. Risk factors for acute kidney injury include elevated preoperative blood urea nitrogen and creatinine levels, congestive heart failure, advanced age, intraoperative hypotension, abdominal aortic clamping, sepsis, and the use of nephrotoxic drugs. Laboratory assessments, including serum sodium, potassium, calcium, phosphorus, urea nitrogen, and creatinine, provide a comprehensive evaluation of renal function.
For patients with chronic renal insufficiency, multidisciplinary collaboration involving surgeons, anesthesiologists, and nephrologists optimizes preoperative preparation to maximize renal function. Dialysis should be performed within 24 hours prior to the scheduled surgery if necessary. Electrolyte levels, particularly serum potassium, need to be maintained within normal ranges for patients with preexisting renal failure.
Diabetes
Patients with diabetes experience stress throughout the perioperative period, leading to a 50% higher rate of complications and mortality compared to non-diabetic individuals. Preoperative assessment for diabetic patients includes evaluation of chronic complications of diabetes (e.g., cardiovascular and renal diseases) and blood glucose control, followed by appropriate management:
- For patients who maintain satisfactory blood glucose levels through diet alone, no special preparation is required before surgery.
- For those taking oral hypoglycemic medications, the medication is usually continued until the evening before surgery. Patients taking long-acting oral hypoglycemic agents discontinue these drugs 2–3 days prior to surgery. During fasting periods, intravenous glucose and insulin are used to maintain a mildly elevated blood glucose level (5.6–11.2 mmol/L).
- For patients on regular insulin therapy, normal glucose metabolism is maintained by the administration of glucose and insulin prior to surgery, while insulin use is withheld on the morning of surgery.
- For patients with diabetic ketoacidosis who require emergency surgery, efforts are made to correct acidosis, hypovolemia, and electrolyte imbalances (particularly hypokalemia) to the greatest extent possible.
Before surgery, HbA1c levels in diabetic patients are recommended to be maintained below 7%. During surgery, blood glucose levels should be monitored and controlled to not exceed 8.33 mmol/L.
Coagulation Disorders
Severe coagulation abnormalities identified through routine coagulation tests account for only 0.2% of cases, making a detailed medical history and physical examination particularly important. The medical history should cover any personal or family history of bleeding or thromboembolic events, prior blood transfusions, bleeding tendencies (e.g., severe hemorrhage during surgeries or menstruation), easy bruising, frequent nosebleeds, or gum bleeding. It should also include questions about coexisting conditions such as liver or kidney disease, malnutrition, excessive alcohol consumption, and the use of aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), or lipid-lowering agents (which may lead to vitamin K deficiency). Additionally, the use of anticoagulants, such as warfarin for atrial fibrillation, venous thromboembolism, or mechanical heart valve replacement, should be reviewed.
During physical examination, attention is given to signs of skin or mucosal bleeding (e.g., petechiae or purpura), splenomegaly, or other indications of systemic disease. For patients on antiplatelet medications, such as ticlopidine and clopidogrel, treatment is discontinued 10 days before surgery. Aspirin is typically stopped 7 days prior, and other NSAIDs are stopped 2–3 days before surgery.
When clinical coagulation disorders are confirmed, treatment is performed before elective surgeries. For procedures where platelet counts fall below 50×109/L, platelet transfusion is recommended. For major surgeries or those involving vascular sites, platelet counts should be maintained above 75×109/L. In neurosurgical procedures, the platelet count should not be lower than 100×109/L. In cases of splenomegaly or immunologically mediated platelet destruction, platelet transfusion may show limited efficacy, and prophylactic platelet transfusion is not routinely recommended. In emergencies, platelet dysfunction caused by medications can be addressed by administering DDAVP (desmopressin) or performing a platelet transfusion. For patients on anticoagulation therapy, the risks of intraoperative bleeding versus postoperative thrombosis must be carefully weighed. Hemophilic patients undergoing surgery require perioperative management with the involvement of hematologists.
Prevention of Deep Vein Thrombosis in the Lower Limbs
Venous thromboembolism is one of the most common postoperative complications. Risk factors for perioperative deep vein thrombosis (DVT) include the following: age over 40 years, obesity, a history of thrombotic events, varicose veins, smoking, major surgeries (especially pelvic, urological, lower limb, or malignancy-related surgeries), prolonged general anesthesia, and coagulation abnormalities. DVT typically originates in the deep veins of the lower limbs and can lead to fatal pulmonary embolism if thrombi dislodge.
For patients with risk factors for venous thrombosis, prophylactic antithrombotic therapy with unfractionated heparin or low molecular weight heparin is recommended. Mechanical preventive measures, such as limb exercises and the use of intermittent pneumatic compression devices, can serve as adjuncts to pharmacological prevention. The combined use of pharmacological and mechanical prophylaxis is beneficial for preventing thromboembolism in high-risk patients.