Interventional radiology technique is a minimally invasive method based on modern imaging technologies such as X-ray, ultrasound, CT, and MRI. This technique involves the use of puncture needles, catheters, guidewires, and other interventional tools to diagnose or treat diseases. It can be categorized into vascular interventional techniques and non-vascular interventional techniques based on the treatment field.
Vascular Interventional Techniques
Under the guidance of imaging equipment, vascular interventional techniques utilize specialized tools to establish percutaneous vascular access via the Seldinger technique. This allows targeted catheters to be directed into specific vessels for diagnostic imaging or therapeutic interventions such as drug infusion, embolization, balloon dilation, or stent placement.
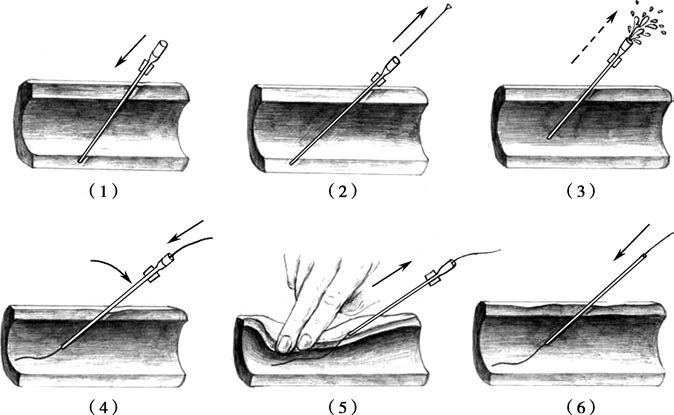
Figure 1 Seldinger technique overview
1, Puncture of the anterior and posterior walls of the artery using a needle with a stylet.
2, Removal of the stylet, followed by slight withdrawal of the needle sheath.
3, Observation of pulsatile bleeding.
4, Introduction of a guidewire into the vessel through the needle sheath, ensuring sufficient length of insertion.
5, Removal of the needle sheath while applying pressure at the puncture site to prevent blood leakage.
6, Insertion of a sheath with a dilator into the vessel.
Transcatheter Vascular Infusion (TVI)
Transcatheter vascular infusion involves delivering drugs directly into the arteries supplying blood to target organs or into returning veins. This approach enhances the drug concentration in the localized pathological area and reduces systemic side effects. It is commonly used in clinical settings for chemotherapy infusion in malignant tumors, local thrombolysis in arterial thrombosis, vasodilation treatment in vasospastic diseases such as Raynaud's disease, and the diagnosis and treatment of gastrointestinal bleeding.
Transcatheter Arterial Chemoembolization or Embolization (TACE or TAE)
TACE involves injecting a mixture of antitumor drugs and embolic agents (such as lipiodol or solid embolic materials) into tumor-feeding vessels via a catheter. This serves to directly destroy tumor cells and induce ischemic necrosis. It is commonly used in palliative care for unresectable liver cancer. TAE is primarily applicable for gastrointestinal bleeding, massive hemoptysis, traumatic hemorrhage (e.g., bleeding in the liver, spleen, kidney, retroperitoneum, and pelvis), arterial aneurysms, hypersplenism, or various arterio-venous fistulas.
Percutaneous Transluminal Angioplasty (PTA)
This technique includes balloon angioplasty and vascular stent placement. Balloon angioplasty uses a balloon catheter to mechanically dilate narrowed arterial walls within a limited range, causing partial stretching, rupture, and separation of the intimal and medial layers while overstretching the adventitia. This results in an expanded arterial lumen, achieving therapeutic effects. Vascular stent placement involves inserting a metal stent into a diseased vessel under X-ray fluoroscopy. The stent provides mechanical support to open a narrowed vessel, restoring normal blood flow. Covered stents can further isolate abnormalities and reconstruct the diameter of dilated vessels, correcting abnormal hemodynamics. This approach is mainly used for conditions such as atherosclerosis, Takayasu's arteritis (in its inactive phase), fibromuscular dysplasia, stenosis at graft or bypass anastomosis sites, and Budd-Chiari syndrome.
Transjugular Intrahepatic Portosystemic Shunt (TIPS)
This technique establishes a connection between the hepatic vein and portal vein within the liver via a transjugular access route. A catheter is inserted through the internal jugular vein, superior vena cava, right atrium, and inferior vena cava into the hepatic vein. With X-ray guidance, the portal vein is punctured using the catheter, creating a shunt that allows blood from the portal vein to flow directly into the hepatic vein. This reduces portal vein pressure and is used to treat complications of portal hypertension, such as upper gastrointestinal bleeding and refractory pleural or abdominal effusion.
Non-Vascular Interventional Techniques
Non-vascular interventional techniques involve procedures performed on non-cardiovascular sites under the guidance of imaging equipment. These include percutaneous biopsy, ablation of solid tumors, implantation of radioactive seeds into solid tumors, drainage and aspiration procedures, dilation and stent placement for luminal strictures, vertebroplasty, nerve block procedures, among others.
Percutaneous Transhepatic Cholangial Drainage (PTCD) and Percutaneous Transhepatic Gallbladder Drainage (PTGD)
These procedures are conducted under X-ray or ultrasound guidance. PTCD involves inserting a puncture needle through the skin and liver tissue to place a catheter in the intrahepatic bile ducts for biliary imaging or drainage. PTGD places a catheter in the gallbladder through a similar approach for drainage purposes.
PTCD is commonly used for palliative treatment of biliary obstruction caused by malignant tumors, reduction of jaundice in severe cases before surgery, biliary drainage in patients with acute biliary infections, or as a pathway for other treatments. For example, the PTCD sinus tract can be dilated to allow diagnostic and therapeutic procedures with a cholangioscope, a technique known as percutaneous transhepatic cholangioscopy (PTCS). Alternatively, post-dilation of biliary strictures through the PTCD sinus tract can permit stent placement, referred to as percutaneous transhepatic biliary stent placement.
PTGD is suitable for patients with acute suppurative cholecystitis who are not fit for surgery due to poor overall condition or severe local inflammation. It can also serve as an alternative to PTCD for biliary drainage in cases where PTCD has failed, such as obstructions in the lower bile duct. However, the presence of spiral valves in the cystic duct means that PTGD is generally less effective than PTCD for biliary drainage.
Percutaneous Ablation Techniques
Percutaneous ablation involves the introduction of physical or chemical agents through puncture routes to destroy target lesions. Ablation therapy is applicable for solid tumors in various parts of the body, especially when surgery is not feasible, not desired by the patient, ineffective with other treatments, or when residual lesions are present. Physical ablation primarily utilizes thermal or cryogenic effects to destroy lesions, including methods like radiofrequency ablation, microwave ablation, and cryoablation. Chemical ablation achieves lesion destruction by injecting agents such as absolute ethanol directly into the target area.
Percutaneous Catheter Drainage for Abscesses or Fluid Collections
Under imaging guidance, a drainage catheter is inserted into an abscess cavity or fluid collection area for treatment. Conditions such as liver abscesses, intra-abdominal abscesses, pelvic abscesses, or fluid accumulations can be treated using this method.
Interventional radiology techniques offer advantages such as minimal invasiveness, precise targeting, rapid efficacy, reproducibility, the ability to combine multiple techniques, and ease of operation. They form an essential part of minimally invasive surgery. However, complications may occur, some of which can be severe and warrant attention. Common complications include infections at the puncture site, bleeding, hematomas, vascular endothelial injury, or pseudoaneurysm formation. Other risks may arise from contrast agent reactions, such as allergic responses or nephrotoxicity, or damage to surrounding tissues and organs. For example, intestinal injury from radiofrequency ablation, pneumothorax or lung damage following thoracic drainage, and tumor seeding along the needle tract may occur.