Microsurgery refers to a surgical technique performed under an operating loupe or surgical microscope, using specialized, fine instruments and materials to repair and reconstruct delicate tissues. Operating under magnification overcomes the natural limitations of human vision, transitioning from macroscopic to microscopic precision, thereby enabling surgeries to be more accurate and meticulous. This technique is characterized by minimal tissue trauma, high surgical quality, and an expanded range of surgical possibilities, allowing procedures previously unachievable with the naked eye to be performed. After more than 60 years of development, microsurgery is now widely applied across various surgical disciplines, such as hand surgery, orthopedics, neurosurgery, plastic surgery, and ophthalmology.
Microsurgical Equipment and Instruments
Optical Magnification Equipment
This includes surgical microscopes and loupes. Different specialties have varied requirements for surgical microscopes. For example, surgical microscopes used in hand surgery, orthopedics, and plastic surgery require:
- Magnification levels from 6 to 40 times, with manual or foot-controlled zoom adjustment.
- A working distance of 200–300 mm, adjustable as needed.
- Dual binocular eyepieces for primary and secondary usage, with a 180° opposing view (90° for neurosurgery and ophthalmic microscopes). Each eyepiece should allow independent adjustment of refractive power and interpupillary distance, provide a large diameter field of view, and deliver upright stereoscopic images.
- A cold light source for coaxial illumination with adjustable intensity.
- A support system for suspending and stabilizing the microscope, which should be flexible and lightweight.
- Interfaces for connecting display screens, observation scopes, cameras, and video systems for demonstration, teaching, and data collection.
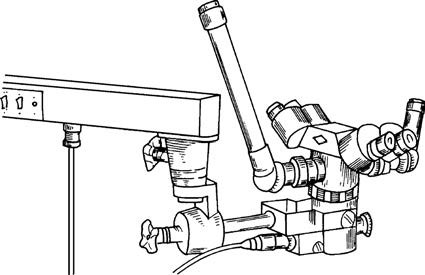
Figure 1 Binocular surgical microscope for two operators
Figure 2 Surgical loupe
Surgical loupes, designed like telescopic systems, can be divided into adjustable and fixed-focus types. The magnification ranges from 2.5 to 6 times, and these loupes are convenient and flexible, making them suitable for suturing blood vessels and nerves with diameters greater than 2 mm.
Microsurgical Instruments
These include microvascular clamps, forceps, scissors, needle holders, vascular clips, approximators, irrigating blunt needles, and more. Common microsurgical instruments include:
- Forceps: Used for grasping and separating delicate tissues as well as holding suture threads for knotting. The forceps should have fine tips with precise alignment, adequate grip, and no cutting edges.
- Scissors: Used for tissue dissection, trimming, and cutting sutures.
- Needle Holders: Equipped with smooth, toothless clamping surfaces of appropriate width, enabling firm grip of fine microsurgical needles and sutures.
- Vascular Clips: Designed to accommodate varying vascular diameters and to occlude blood flow without damaging the vessel wall.
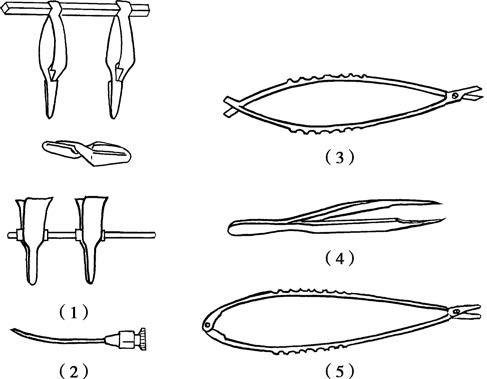
Figure 3 Microsurgical instruments
(1) Vascular Clamps and Approximator
(2) Irrigating Blunt Needle
(3) Spring-Handle Microsurgical Scissors
(4) Vascular Forceps
(5) Needle Holder
Microsurgical Sutures and Needles
Microsurgical sutures and needles come in varying specifications to suit different vessel diameters.
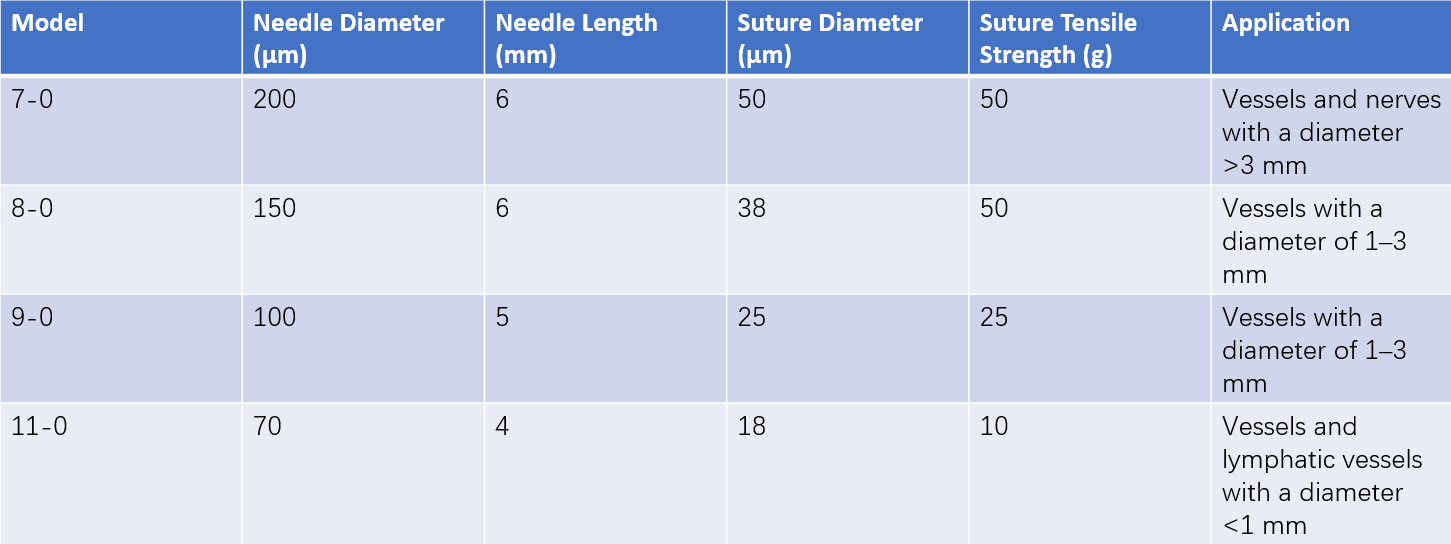
Table 1 Common specifications of microsurgical sutures and needles
Basic Microsurgical Techniques
The basic techniques of microsurgery encompass vascular and lymphatic anastomosis as well as nerve and tendon suturing, with vascular anastomosis being the most commonly performed and technically demanding. Microsurgical vascular and nerve anastomoses are described as follows:
Microsurgical Vascular Anastomosis
This includes two types: end-to-end and end-to-side anastomosis. End-to-end anastomosis is the more common of the two. Key principles and techniques include:
Non-Traumatic Technique
While operating, the vessel adventitia is clamped, avoiding the introduction of sharp instruments into the vessel lumen or clamping the vessel wall with forceps. This minimizes the risk of endothelial damage and subsequent thrombosis.
Heparinization of Vessel and Vascular Bed
Heparinized saline is dripped onto the vascular bed and vessel surface and used to flush the vessel lumen to maintain heparinization and prevent localized blood clotting.
Vessel End Cleansing and Adventitia Trimming
The vessel wall should be carefully examined for damage under the microscope. Injured parts of the vessel wall must be excised. The edge of the adventitia near the severed end should be grasped with forceps, pulled outward, and trimmed to prevent it from entering the vessel lumen and causing thrombosis.
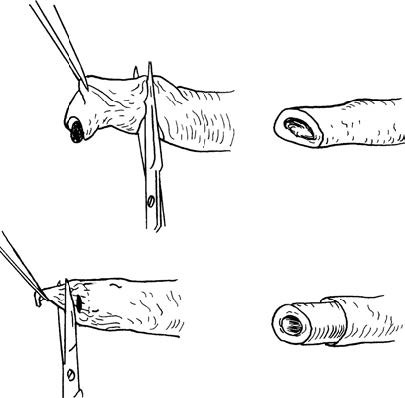
Figure 4 Vessel debridement and adventitia removal
Vessel Suturing
Suturing Method
The two-point fixation method is commonly used. One suture is placed at the 0° position of the vessel, and another at the 180° position. These two sutures are pulled to achieve even traction, and the vessel wall is sutured according to its diameter with 2–4 additional stitches. The vessel is then rotated for 180°, and the remaining wall is sutured evenly.
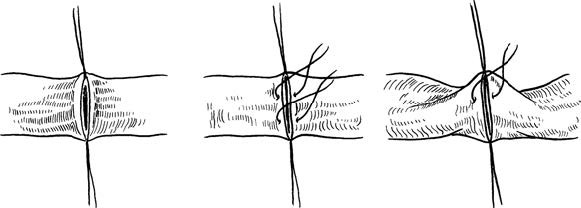
Figure 5 Two-point fixation method for vascular suturing
Stitch Interval and Margins
These are determined by the vessel diameter, wall thickness, and intraluminal pressure. For arteries, the stitch margin is typically twice the thickness of the vessel wall, with stitch intervals twice the stitch margin. For veins, which have thinner walls, the stitch margin can be slightly larger than that for arteries.
Needle Insertion and Exit
The needle should enter the vessel wall vertically and follow its arc to exit smoothly.
Knot Tying
The knots should result in slight external eversion of the vessel with proper alignment of the intima. The first knot should be moderately tightened, while the second and third knots should be firmly secured.
Leakage Check and Management
After suturing, the vascular clamps are released and blood flow is restored. Minor leaks can be treated by gently compressing with a small piece of moistened gauze. Jet-like bleeding at the anastomotic site indicates the need for an additional suture.
Besides suturing, non-suturing techniques for microsurgical vascular anastomosis (e.g., laser welding, electrocautery, and adhesive methods) have also been researched but remain largely experimental with limited clinical application.
Microsurgical Nerve Suturing
Microsurgical nerve suturing techniques include epineurial and perineurial suturing methods.
Applications of Microsurgery
Microsurgery can be applied in all surgical disciplines that rely on surgery as the primary treatment method.
Replantation of Severed Limbs (or Digits)
The replantation of severed limbs or digits is one of the important applications of microsurgical techniques.
Vascularized Tissue Transplantation
The most common and widely applicable use of microsurgery lies in the transplantation of vascularized tissues.
Vascularized Flap or Composite Flap Transplantation
This includes skin flaps or composite muscle and bone-containing flaps. These tissue flaps, incorporating a complete arterial and venous system, consist of skin, subcutaneous tissue, or muscles forming skin flaps or muscle (skin/bone) flaps. Survival after transplantation depends on vascular anastomosis to restore blood supply, hence they are referred to as "free tissue transfers."
Skin flaps are mainly used in situations such as:
- Skin and soft tissue defects with underlying exposed structures (e.g., tendons, bones, or joints) caused by trauma, burns, or tumors.
- Severe contracture deformities of joints due to scarring.
- Chronic, non-healing ulcers.
- Reconstruction of missing or damaged tissues or organs.
Muscle flaps are not only used to repair soft tissue defects but are also employed to fill dead spaces resulting from bone infections. If a muscle flap includes its innervating motor nerve, it can be transplanted to repair damaged or necrotic muscles or to replace permanently denervated muscles, thereby restoring joint mobility.
Currently, more than 30 types of commonly used free skin flaps and more than 20 types of muscle (skin) flaps are available. Selection is based on the location, size, characteristics of the tissue defect, or specific therapeutic requirements. Common types include scapular flaps, abdominal flaps, radial forearm flaps, anterolateral thigh flaps, pectoralis major muscle (skin) flaps, and latissimus dorsi muscle (skin) flaps.
Vascularized Bone and Periosteal Transplantation
Transplantation of vascularized bone and periosteal tissues is used to treat nonunion fractures, bone defects, and osteonecrosis. Due to the presence of a blood supply, the healing process shifts from the conventional "creeping substitution" seen in conventional bone grafting to the natural healing mechanism of fractures, significantly reducing the time required for bone healing. Commonly used vascularized bone grafts include fibula, iliac crest, and scapula.
Vascularized Omental Transplantation
This involves the repair of soft tissue defects, treatment of obliterative vascular diseases, and management of chronic osteomyelitis.
Vascularized Free Lymph Node Transplantation
This method is employed in the treatment of limb lymphedema.
Toe-to-Hand Transplantation for Thumb or Finger Reconstruction
Since the first report in 1966 of using vascularized second toe transplantation to reconstruct a thumb, significant advancements have been made in the reconstruction of finger defects. This has not only restored the appearance of the hand but has also greatly improved its sensory and motor functions.
Vascularized Jejunal Transplantation
This method is used to repair esophageal defects caused by cervical or thoracic esophageal stricture, congenital defects, or atresia, as well as to reconstruct lost esophageal segments following surgeries for cancers such as pharyngolaryngeal or upper/mid-esophageal carcinoma.
Peripheral Nerve Microsurgical Repair
Microsurgical techniques address the limitations of conventional repair methods, such as poor alignment and neuroma formation in peripheral nerve repairs performed under direct vision. This has resulted in more precise nerve coaptation and improved repair outcomes.
Microsurgical Repair of Small Ducts
This includes microsurgical anastomosis of structures such as the vas deferens, fallopian tubes, and nasolacrimal ducts.
Vascularized Organ Transplantation
Microsurgery plays a key role in organ transplantation fields, including liver transplantation, kidney transplantation, heart transplantation, lung transplantation, testicular transplantation, ovarian transplantation, and parathyroid transplantation.
Recent Advances in Microsurgical Techniques
Since the 1990s, developments in surgical techniques, widespread application of digital technology, and improvements in microsurgical instruments have driven the field of microsurgery towards new frontiers, giving rise to supermicrosurgery and digital microsurgery.
Supermicrosurgery
Supermicrosurgery is defined as a technique involving the anastomosis of extremely small blood vessels or single nerve fascicles, with vessel diameters ranging from 0.3 to 0.8 mm. Technically, supermicrosurgery requires greater precision and the use of specialized microsurgical instruments. The advent of supermicrosurgery has enabled the anastomosis of vessels previously considered too small to handle, thereby expanding donor tissue options. Donor sites can now be selected based on tissue type, volume, similarity, and texture to better match the recipient site, enabling more precise repairs and achieving highly satisfactory outcomes.
In recent years, supermicrosurgery has been successfully employed for various specialized perforator flaps, such as ultra-thin perforator flaps, flow-through perforator flaps, chimeric perforator flaps, segmented perforator flaps, and conjoined perforator flaps. Common perforator flaps include anterolateral thigh perforator flaps, deep inferior epigastric artery perforator flaps, thoracodorsal artery perforator flaps, and circumflex scapular artery perforator flaps. Additionally, lymphaticovenous anastomosis and free lymph node flap transplantation have emerged as new and growing applications of supermicrosurgery.
Digital Microsurgery
Conventional anatomical studies often describe the vascular supply system, trajectory, and relationship with surrounding tissues in terms of probabilities or concepts. However, vascular anomalies occasionally result in surgical plan alterations or inadvertent vascular injury, potentially leading to surgical failures.
Digital microsurgery allows for a transition from two-dimensional to three-dimensional imaging and from static to dynamic anatomical visualization. Microsurgical anatomical structures can be observed in 3D from any angle. Using preoperative CT angiography and post-processing workstations, three-dimensional reconstructions of the surgical field can be created, providing a clear and detailed depiction of the arterial network in the operative area. This approach clarifies the relationship between skin and blood vessels and offers precise preoperative measurements, including vascular pedicle length and vessel diameter compatibility. As a result, digital microsurgery not only enhances the precision of surgical planning but also significantly improves the success rate of microsurgical procedures.