Various types of organ transplantation have been applied in clinical practice, including kidney, liver, heart, pancreas, lung, small intestine, spleen, adrenal gland, parathyroid gland, testis, ovary, as well as combined transplants such as heart-lung, liver-small intestine, heart-liver, pancreas-kidney, liver-lung, and multi-visceral transplantation within the abdominal cavity. With improving outcomes year over year, a significant number of recipients have achieved long-term survival, returning to normal life and work.
Kidney Transplantation
Among all types of organ transplantation, kidney transplantation (renal transplantation) is the most well-established. The overall 1-year and 5-year survival rates currently exceed 97% and 90%, respectively, with even higher survival rates observed in living-donor kidney transplants. Chronic rejection remains the leading cause of graft failure, while infections, cardiovascular diseases, and malignancies are the primary factors affecting long-term survival in kidney transplant recipients. Indications for kidney transplantation include various kidney diseases that have progressed to chronic renal failure (uremia), such as chronic glomerulonephritis, chronic pyelonephritis, polycystic kidney disease, diabetic nephropathy, hypertensive nephropathy, interstitial nephritis, and autoimmune kidney diseases.
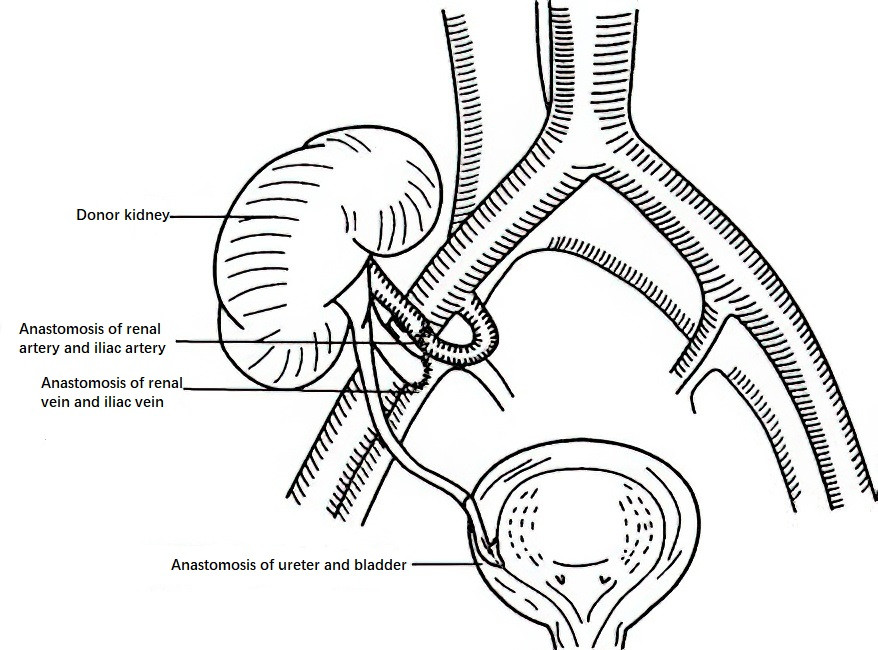
Figure 1 Kidney transplantation
The surgical procedure for kidney transplantation has been standardized. The transplanted kidney is placed in the retroperitoneal iliac fossa, with the right iliac fossa chosen as the first option and the left iliac fossa as the alternative. The renal artery is anastomosed to the internal or external iliac artery, while the renal vein is anastomosed to the external iliac vein. The ureter is connected to the bladder mucosa via a short tunnel formed by the bladder's seromuscular layer to prevent urinary reflux. Typically, a double "J" stent is placed at the ureter-bladder anastomosis site to reduce the risk of ureteral complications.
Liver Transplantation
For liver transplantation (Liver transplantation), the current 1-year survival rate approaches 90%, and the 3-year survival rate is close to 80%, with better outcomes observed in pediatric cases compared to adults. Indications for liver transplantation include progressive, irreversible, and life-threatening end-stage liver diseases where no other effective treatments are available, such as end-stage liver cirrhosis, cholestatic liver diseases, congenital metabolic liver disorders, acute liver failure, and benign or malignant liver tumors. The internationally recognized criteria for liver transplantation in hepatocellular carcinoma are the Milan criteria, which specify a single tumor with a diameter not exceeding 5 cm, or up to three tumors with the largest diameter no greater than 3 cm, without major vascular invasion, lymph node involvement, or extrahepatic metastasis.
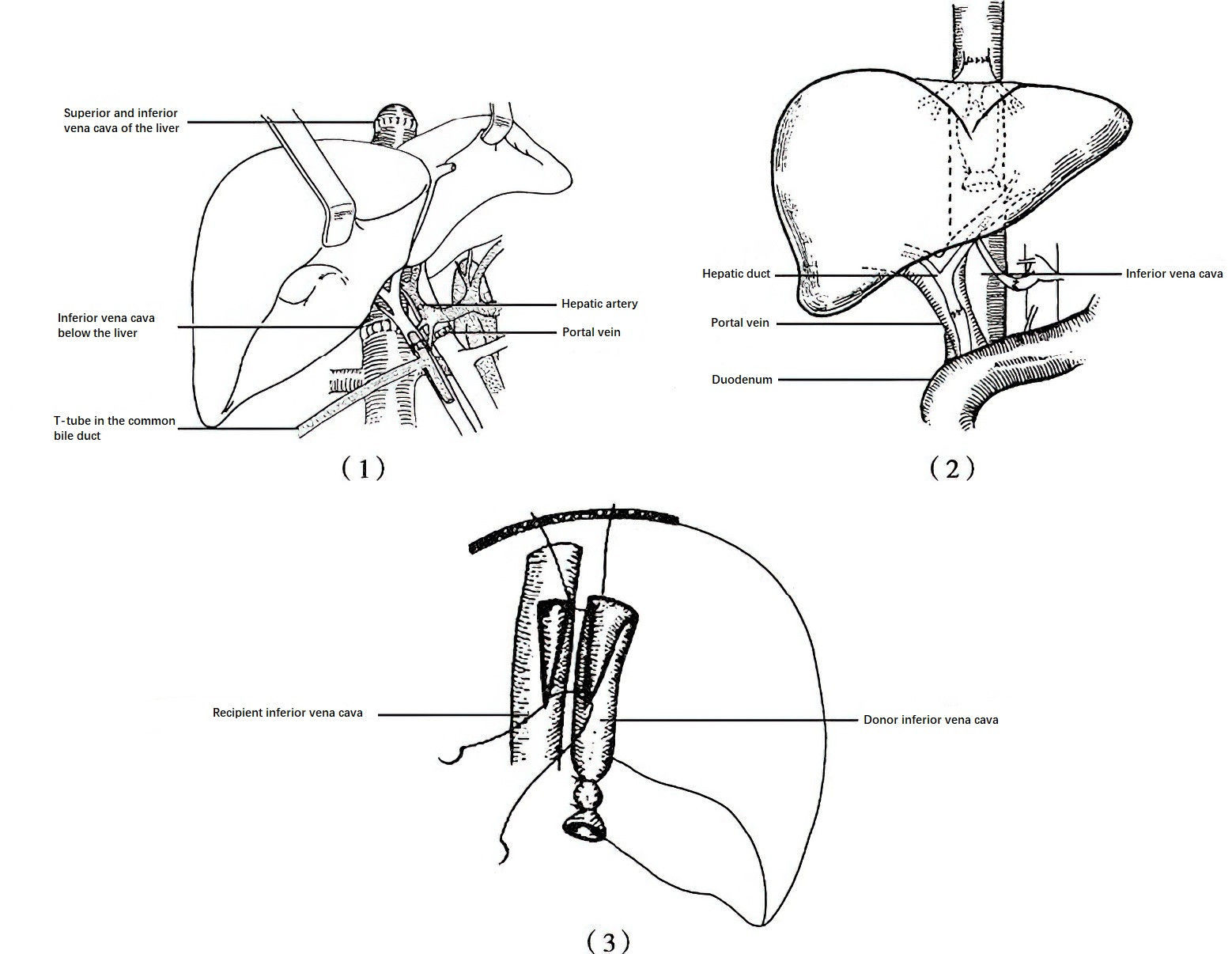
Figure 2 Liver transplantation
1, Orthotopic Liver Transplantation
2, Piggyback Liver Transplantation
3, Ameliorated Piggyback Liver Transplantation
The classical surgical approaches for liver transplantation include orthotopic liver transplantation, piggyback liver transplantation, and ameliorated piggyback liver transplantation.
In orthotopic liver transplantation, both the recipient's inferior vena cava and diseased liver are removed, followed by orthotopic anastomosis of the donor liver.
In piggyback liver transplantation, the recipient's inferior vena cava is preserved, and the recipient's hepatic veins are reconstructed and anastomosed with the donor's superior and inferior vena cava. This approach allows maintenance of partial or complete venous return to the heart during the anastomosis of the donor and recipient vena cava and the portal vein, thereby ensuring circulatory stability in the recipient.
The ameliorated piggyback liver transplantation further improves the procedure by enlarging the ostia of the donor's inferior vena cava and the recipient's three hepatic veins, reshaping them into triangular openings for better alignment, thus facilitating unobstructed venous outflow.
In addition to whole liver transplantation, partial liver transplantation is also performed. Split-liver transplantation involves dividing a single donor liver into two parts, which are then transplanted into two different recipients. Living-related liver transplantation involves taking a portion of a relative's liver (such as the left lateral segment, left lobe, or right lobe) for transplantation into the recipient, under the condition that minimal harm is caused to the donor and the recipient achieves outcomes comparable to conventional liver transplantation. Other techniques include reduced-size liver transplantation, heterotopic and auxiliary liver transplantation, and domino liver transplantation.
Pancreas Transplantation
Pancreas transplantation in clinical practice can be categorized into three types: simultaneous pancreas-kidney transplantation (SPK), pancreas-after-kidney transplantation (PAK), and pancreas transplantation alone (PTA). SPK is the most commonly performed pancreas transplantation procedure. In recent years, some transplant centers have reported patient 1-year survival rates exceeding 95%, while 1-year graft survival rates can surpass 85%.
Simultaneous pancreas-kidney transplantation has become widely recognized as the most effective treatment for type 1 diabetes with uremia and select cases of type 2 diabetes. Pancreas transplantation alone can delay or even partially reverse severe diabetes-related complications, but careful evaluation of surgical risks versus patient benefits is necessary. The indications for surgery need to be strictly adhered to, and decisions are typically based on the severity of diabetes complications, blood glucose control, and kidney function.
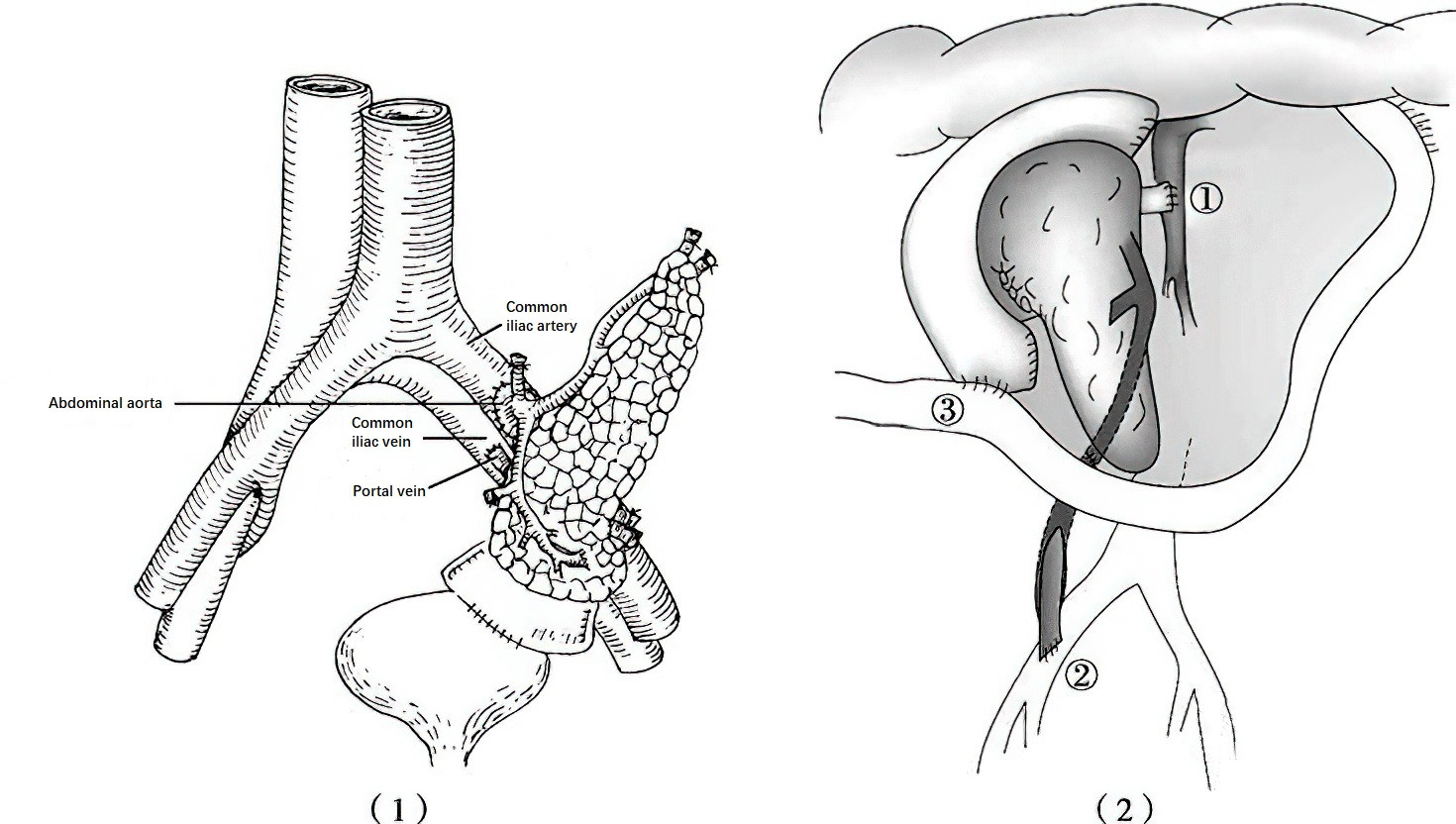
Figure 3 Pancreas transplantation
1, External exocrine bladder drainage and endocrine systemic circulation drainage
2, External exocrine intestinal drainage and endocrine portal venous drainage (① Portal vein anastomosis; ② Iliac artery anastomosis; ③ Duodenum-jejunum anastomosis)
The key aspects of pancreatic transplantation surgery involve reconstruction of the exocrine and endocrine drainage of the transplanted pancreas. For exocrine drainage, two main techniques are employed: enteric drainage and bladder drainage. Early pancreas transplants often used bladder drainage, where a segment of the donor duodenum was anastomosed to the recipient's bladder. However, this method has significant drawbacks, such as substantial pancreatic juice loss through the urine, leading to intractable metabolic acidosis, as well as long-term complications like chemical cystitis, chronic urinary tract infections, and urethral strictures. Enteric drainage is now more commonly used, where the donor duodenum is anastomosed to the recipient's jejunum or duodenum. Enteric drainage is more physiologically appropriate and avoids the disadvantages associated with pancreatic fluid excretion through the urinary tract, making it the standard surgical technique.
For endocrine drainage, circulation from the transplanted pancreas can flow into either the systemic circulation or the portal venous system. While portal venous drainage is theoretically more physiologically appropriate than systemic drainage, studies have shown no significant difference in clinical outcomes between the two methods. Currently, systemic circulation is more commonly used in clinical practice.
Small Intestine Transplantation
Small intestine transplantation (bowel transplantation) is associated with a high incidence of rejection, severe infections, and complications such as graft-versus-host disease, due to the unique physiological characteristics of the small intestine. Despite these challenges, advances in small intestine transplantation have led to 1-year and 5-year post-transplant survival rates of 91% and 75%, respectively, in some transplant centers.
The primary indication for small intestine transplantation is intestinal failure caused by various conditions, particularly in cases where nutritional support is poorly tolerated. Based on the contents of the graft, small intestine transplantation can be classified into isolated small intestine transplantation, combined liver-small intestine transplantation, and multi-visceral transplantation.
The general steps of the procedure include anastomosing the donor's superior mesenteric artery to the recipient's abdominal aorta or common iliac artery, and the donor's superior mesenteric vein to the recipient's inferior vena cava, common iliac vein, portal vein, or superior mesenteric vein. A proximal end-to-end anastomosis is performed on the intestinal segment, while the distal end is externalized as a stoma.
Lung Transplantation
Lung transplantation (lung transplantation) has been widely performed across the globe. Data from some transplant centers indicate 1-year, 3-year, and 5-year survival rates of 80%, 64%, and 52%, respectively. Primary graft dysfunction in the early postoperative period and long-term complications such as bronchiolitis obliterans syndrome remain major limiting factors for long-term survival.
Common indications for lung transplantation include idiopathic pulmonary fibrosis, chronic obstructive pulmonary disease, silicosis, primary pulmonary hypertension, cystic fibrosis, bronchiectasis, alpha-1-antitrypsin deficiency, and lymphangioleiomyomatosis of the lung.
Common surgical techniques include single lung transplantation, bilateral sequential lung transplantation, lobe transplantation, and transplantation following lung volume reduction.
Heart Transplantation
Heart transplantation (cardiac transplantation) remains the only effective treatment for end-stage heart disease. The current 1-year and 5-year survival rates after the procedure are 85% and 75%, respectively. Coronary artery disease caused by chronic rejection is the leading factor affecting long-term survival following heart transplantation.
The primary indications for heart transplantation include nonspecific cardiomyopathy and ischemic heart disease. In addition, conditions such as primary pulmonary hypertension, Eisenmenger syndrome, and severe cardiac disease with irreversible pulmonary or pulmonary vascular involvement may require combined heart-lung transplantation.
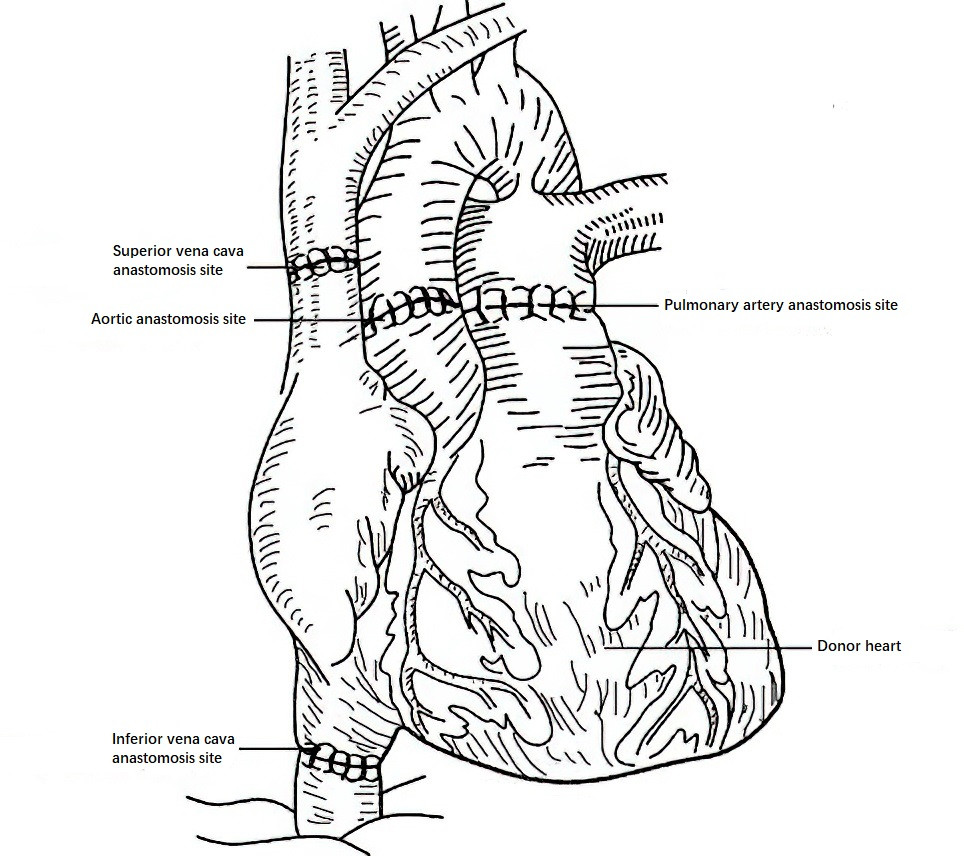
Figure 4 Heart transplantation
The main surgical techniques for orthotopic heart transplantation include the biatrial technique, the total technique, and the bicaval technique. Currently, the bicaval technique has become the standard approach for heart transplantation, as it offers improved surgical outcomes.