Burn injury is a common and distinct type of trauma. In the narrow sense, burn injury generally refers to thermal burns, which are caused by the transfer and conduction of heat energy from hot objects, including flames, hot liquids (such as water, soup, oil), hot gases (such as steam), or hot solids (such as metal, charcoal), resulting in tissue damage. Injuries caused by flames are often referred to as burns, while injuries caused by hot liquids, steam, or solids are referred to as scalds. However, since their pathophysiological characteristics and clinical courses are identical, they are collectively referred to as burns in clinical practice.
In addition to heat, electrical energy, chemicals, and radioactive materials can cause similar pathological changes and clinical courses, known as electric burns, chemical burns, and radiation burns, respectively. Thermal burns account for approximately 90% of all burns, while electric and chemical burns each account for about 5%. Severe burns can cause not only local tissue damage but also a series of systemic physiological and pathological changes.
Assessment of Injury Severity
Factors Determining Burn Severity
The severity of a burn injury is primarily determined by four factors: the burn area, the depth of the burn wound, the presence of associated or combined injuries, and the patient's general condition.
Burn Area
To date, clinical estimation of burn area still largely relies on visual assessment and clinical experience, using the percentage of the total body surface area (TBSA) affected. Common methods include the Rule of Nines and the palmar method. For very small burn wounds, the absolute area is sometimes used. Although some studies have explored using 3D photography or scanning technologies for more accurate calculation, these methods are not yet widely used clinically.
Rule of Nines
The adult body surface is divided into areas of 9% each: head and neck (9%), both upper limbs (18%), anterior and posterior torso including perineum (27%), and both lower limbs and buttocks (36%). In children, the head constitutes a larger proportion, while the lower limbs and buttocks constitute a smaller proportion. For children, head and neck area is calculated as [9 + (12 - age)]%, and lower limbs as [46 - (12 - age)]%.
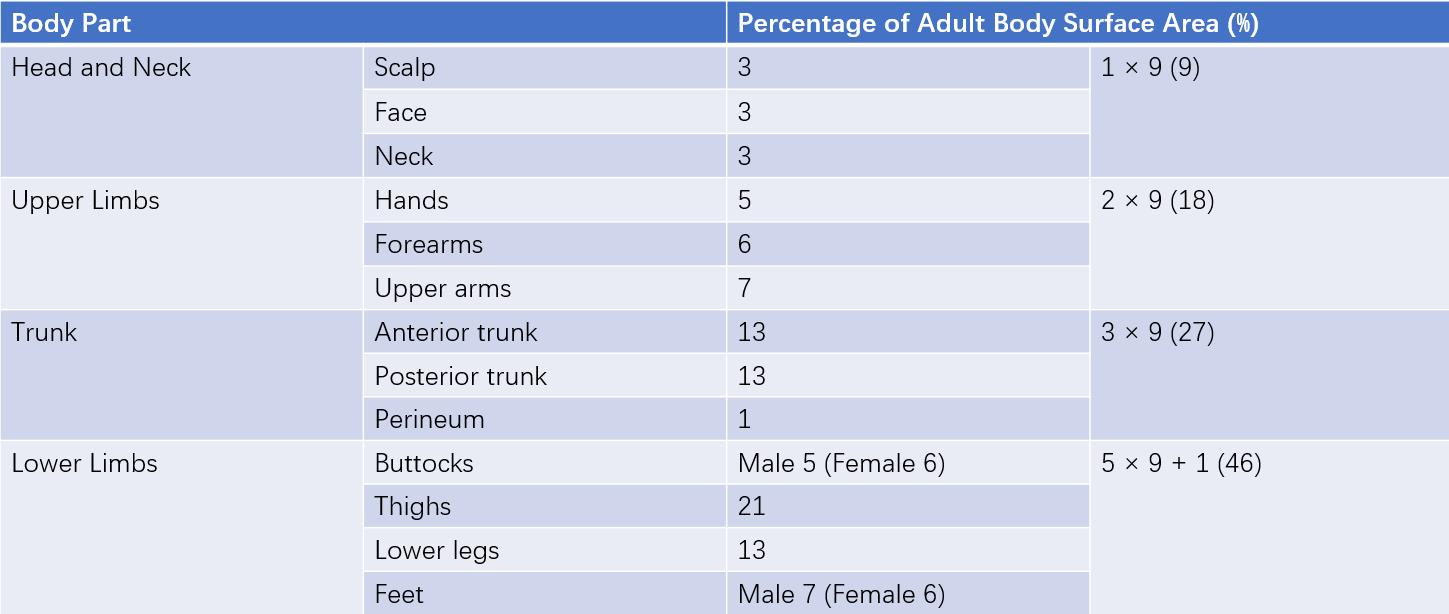
Table 1 Rule of nines for estimating adult body surface area
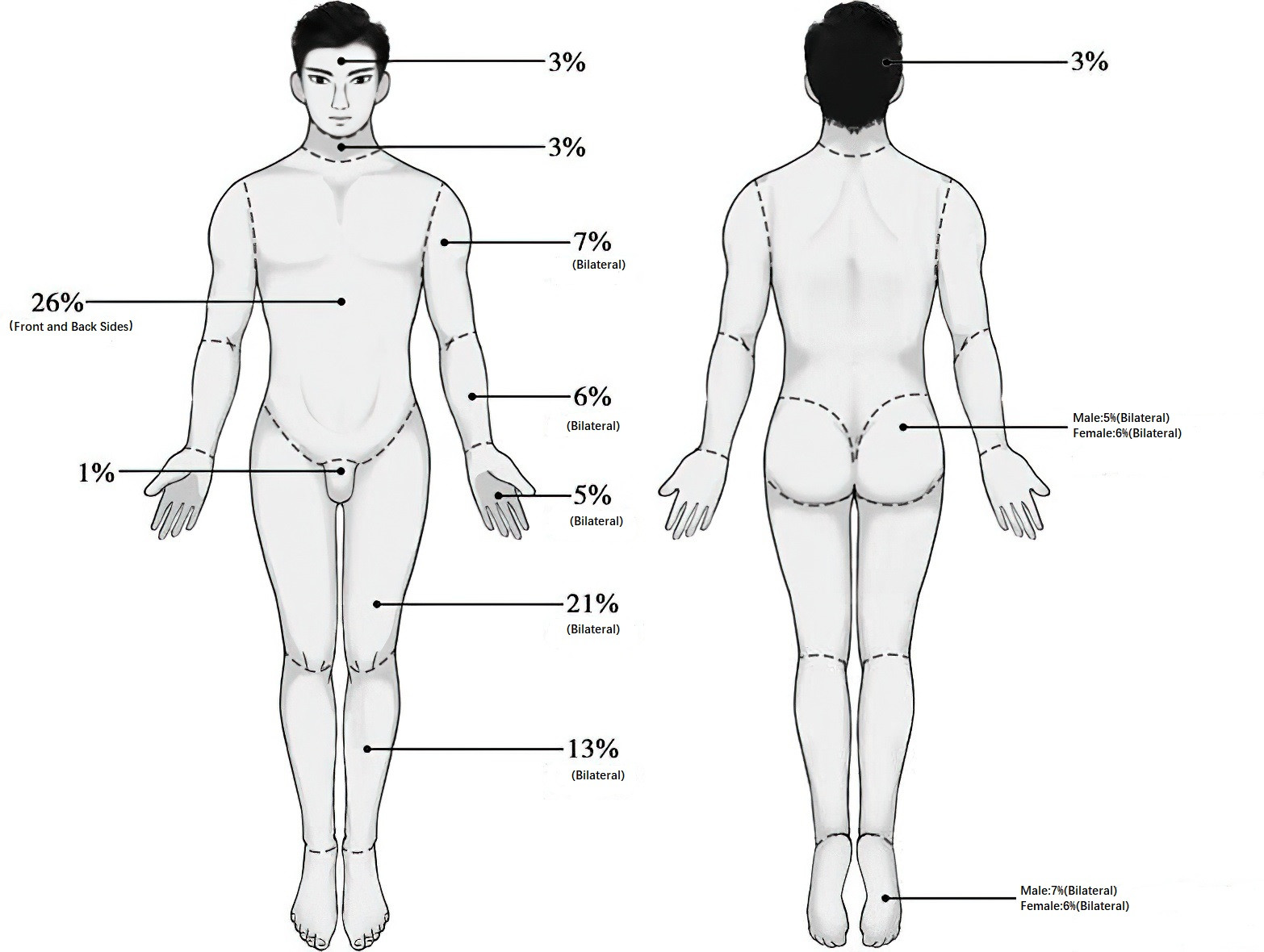
Figure 1 Rule of nines for estimating adult body surface area
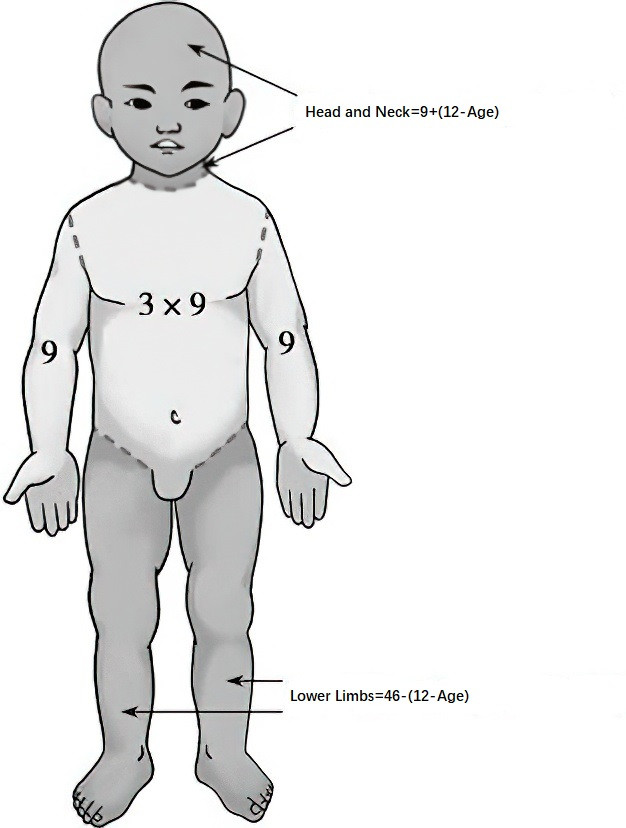
Figure 2 Estimation of burn area in children
Palmar Method
The surface of the patient’s palm with fingers together represents approximately 1% of their total body surface area. The entire hand, including the palm, back of the hand, and fingers, accounts for about 2.5%, and both hands together about 5%.
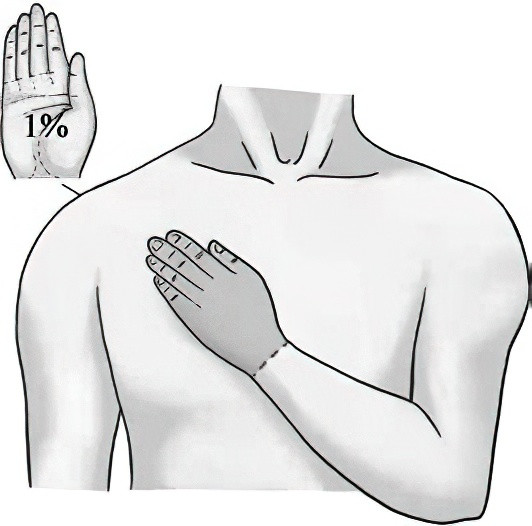
Figure 3 Palmar method for estimating burn area
Burn Depth
Burn depth determines the treatment approach and healing outcome. Clinically, depth is primarily assessed visually. Although technologies like infrared imaging, near-infrared imaging, and ultrasound are being explored, they are not yet widely practical. The commonly used classification is the three-degree, four-level system: first-degree, superficial second-degree, deep second-degree, and third-degree burns.
- First-Degree Burns: Affect the epidermis, presenting as erythema, localized pain, and a burning sensation. Healing usually occurs within three days without scarring.
- Second-Degree Burns: Characterized by the formation of blisters.
- Superficial Partial-Thickness Burns: Involve the superficial dermis, with blisters containing plasma-like fluid. The wound appears red with a granular texture, and is very painful. Healing typically occurs within 10–14 days without scarring.
- Deep Partial-Thickness Burns: Extend below the papillary dermis, often with fewer and smaller blisters. The wound may appear pale or mottled, with diminished sensation and lower temperature. Healing takes about 3–4 weeks and often results in scarring and functional impairment.
- Third-Degree Burns: Full-thickness burns extending through the entire dermis and potentially affecting muscles, bones, and internal organs. The wound forms an eschar and typically appears leathery, dry, and insensate. Healing usually requires surgical excision and skin grafting.
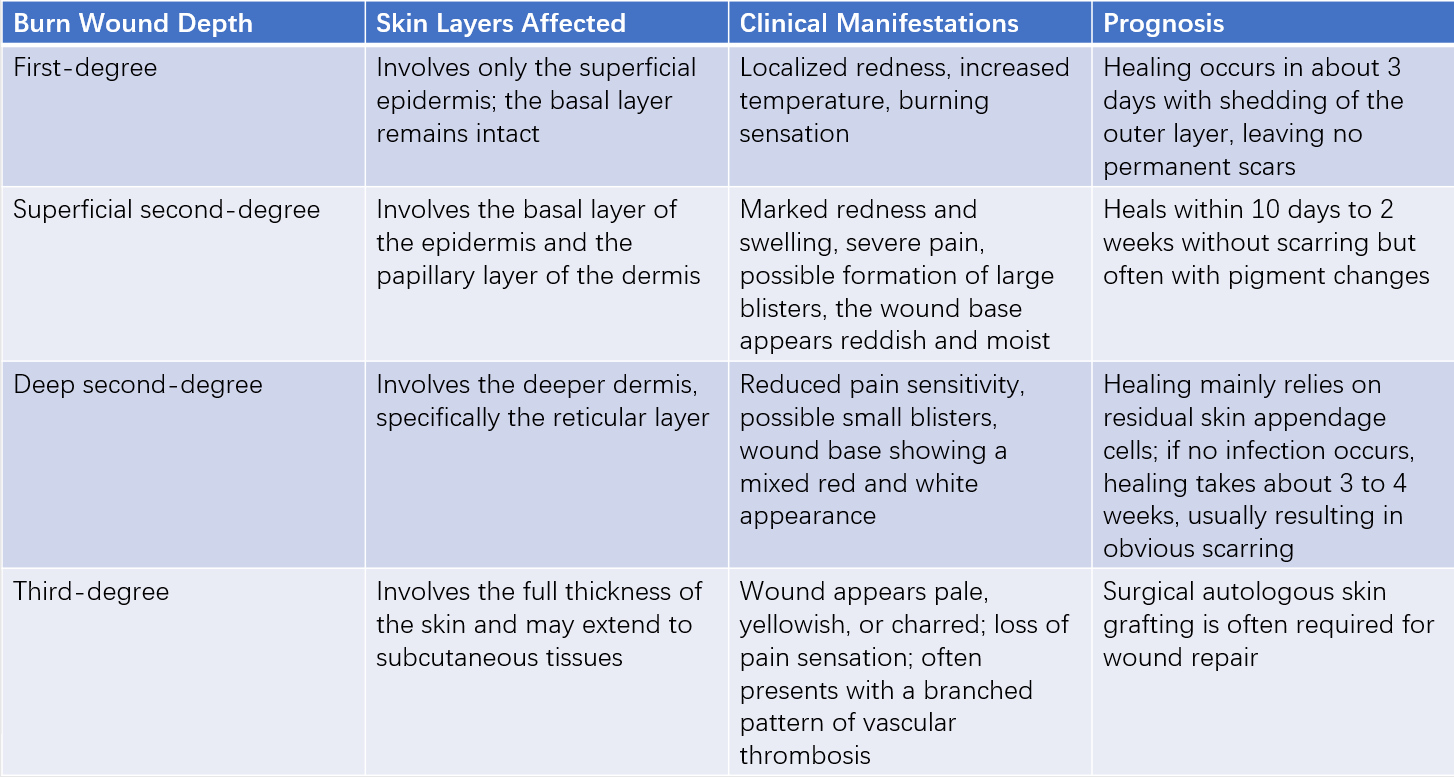
Table 2 Three-degree, four-level classification of burn depth
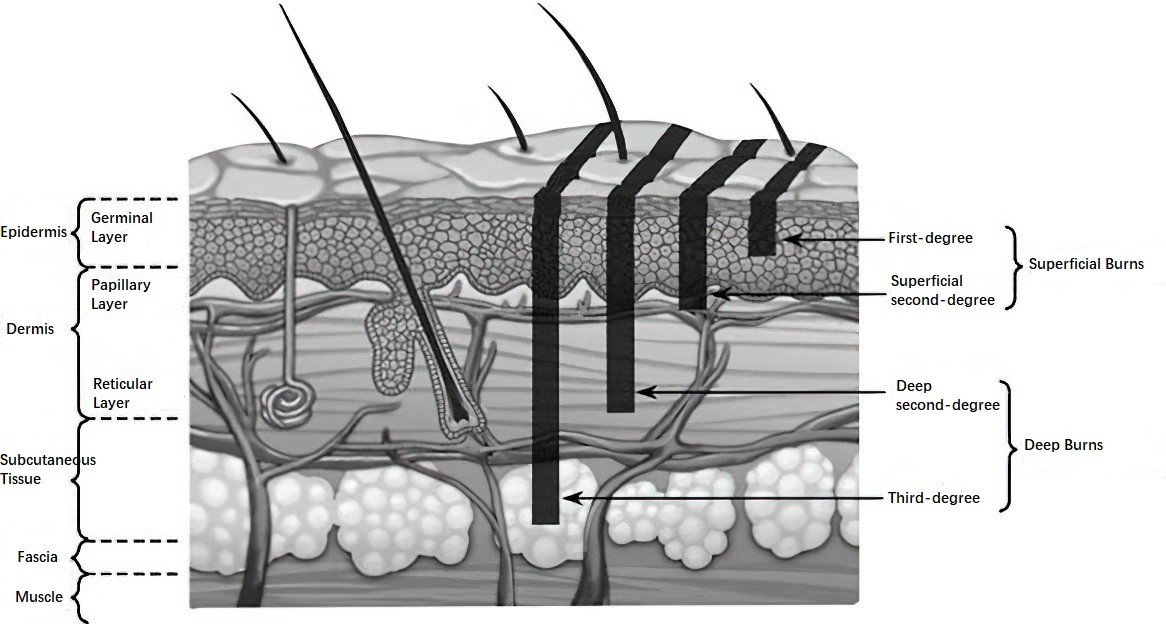
Figure 4 Three-degree, four-level classification of burn depth
Some burns are classified as mixed-thickness burns, and burns involving tissues below the deep fascia (such as muscles or bones) are sometimes categorized as fourth-degree burns. Burn depth may evolve over time, requiring reassessment around 72 hours after injury.
Associated and Combined Injuries
Inhalation Injury
This is common in burns, particularly in enclosed spaces. Inhalation of hot air, carbon monoxide, or toxic smoke can cause airway damage, hypoxia, and is a major early cause of burn-related mortality.
Combined Injuries
This refers to additional injuries (such as soft tissue, bone, vascular, or organ injuries) caused by mechanisms other than heat, such as falls or crush injuries, which can significantly complicate burn management.
Patient General Condition
Age, baseline health status, past medical history, and even gender can influence burn severity and outcomes.
Classification of Burn Severity
Burn severity is mainly determined by the extent and depth of the burn. Some experts use a burn index that combines these factors for overall assessment. Two common formulas include:
Burn Index=(Third-degree area + Second-degree area)/2
Or
Burn Index=Third-degree area + 2/3×Deep Second-degree area + 1/3×Superficial Second-degree area
Additionally, the Abbreviated Burn Severity Index (ABSI) incorporates factors such as gender, age, and inhalation injury to provide a more comprehensive assessment of burn severity.
Pathophysiology and Clinical Staging of Burns
Based on the pathophysiological progression of burns, the clinical course is generally divided into four stages: the fluid exudation and reabsorption phase, the acute infection phase, the wound healing phase, and the rehabilitation phase. In cases of mild burns, these stages may not be clearly distinguishable, while in severe burns, the four stages do not have precise time boundaries and often overlap.
Fluid Exudation and Reabsorption Phase
Burn injury compromises the skin barrier and damages blood vessels, leading to vascular leakage and local swelling. Severe burns (typically defined as second- and third-degree burns covering more than 10–15% of the body surface area in adults or more than 5% in children) trigger intense systemic stress and inflammatory responses, resulting in increased vascular permeability throughout the body. In addition to local fluid leakage at the burn site, similar leakage can occur in distant tissues and even organs.
Fluid exudation is most intense within 2–3 hours after injury, peaks at 6–8 hours, and generally lasts for 24–48 hours. In extremely severe burns, this phase may last longer.
As the burn progresses, vascular permeability gradually returns to normal, marking the onset of the reabsorption phase. During this phase, some of the small molecules that have leaked into the extravascular space are reabsorbed into the bloodstream, and tissue swelling subsides. The reabsorption phase generally lasts from 3 to 7 days after burn.
Acute Infection Phase
Following a burn, the mechanical barrier of the skin is compromised, allowing microorganisms from the environment or residual skin flora to invade the body. Necrotic tissue provides an excellent medium for microbial growth, increasing the risk of acute infection. Additionally, severe burns can impair immune function due to stress, shock, and disruption of gut microbiota, further predisposing patients to infection.
Clinical evidence indicates that the period between 7 and 14 days after burn is a peak time for early infections in severe burns. Treatment during this phase focuses primarily on wound care and infection prevention and management.
Wound Healing Phase
The wound healing process begins immediately after injury and continues until the wound is fully closed and healed. Factors such as burn depth, the local microenvironment, and the patient’s overall condition influence both the duration and the outcome of this phase.
Superficial and deep second-degree burns without severe infection generally heal spontaneously. However, third-degree burns and deep second-degree burns complicated by severe infection or prolonged pressure often require interventions such as autologous skin grafting for wound closure.
Rehabilitation Phase
Rehabilitation is gaining increasing importance in the management of burn patients. Those with severe burns often require multiple surgeries and extended periods of bed rest and hospitalization, making rehabilitation essential. Current clinical practice emphasizes initiating rehabilitation early in the course of severe burns and continuing it throughout the patient’s lifetime.
After healing, deep burn wounds frequently result in varying degrees of scarring, which can affect appearance, function, and psychological well-being. Rehabilitation efforts typically include surgical reconstruction, physical and occupational therapy, phototherapy and laser treatments, and psychological support.
Principles of Treatment
The principles of burn treatment include:
- Prompt cessation of the injury source, ensuring airway patency, and applying cooling therapy;
- Timely management of stress and inflammation responses and initiation of fluid resuscitation;
- Expedited wound closure;
- Prevention and management of wound and systemic infections through appropriate use of antimicrobial agents;
- Maintenance of internal homeostasis and organ function, along with enhanced nutritional and symptomatic support;
- Emphasis on restoring form, function, and psychological well-being.
On-Site First Aid, Transport, and Early Treatment
On-Site First Aid
Rapid Removal from the Heat Source
When exposed to flame burns, quick removal from the fire scene is essential. Burning clothing should be taken off, or methods such as rolling on the ground, dousing with water, or jumping into a water pool can be employed to extinguish the fire. Rescuers may use non-flammable thick items like quilts or blankets to cover the patient and isolate the fire from oxygen. Running or shouting while on fire should be avoided, as this may worsen the flames due to wind and increase the risk of facial burns or inhalation injuries. Clothing soaked with hot liquid should be quickly rinsed with cold water and cut away rather than forcibly removed, to prevent tearing blisters or skin and causing further injury.
Cooling Therapy
Immediately after rescue from the fire scene, cooling therapy becomes the most important emergency measure. The earlier it is applied, the better the effect. Cooling therapy helps prevent ongoing thermal damage that deepens the wound and can reduce pain, exudation, and swelling. This may involve rinsing or soaking the wound with clean cold water or tap water, or applying cold water–moistened towels or gauze pads to the affected area. Cooling is generally continued until severe pain subsides, often requiring 30 to 60 minutes or longer.
Initial Assessment and Pre-Hospital Care
While cooling therapy is ongoing, the victim’s vital signs should be promptly assessed to rule out life-threatening conditions such as massive hemorrhage, open pneumothorax, or severe poisoning. After ensuring vital signs are stable, a preliminary estimate of burn area and depth can be made to determine burn severity. Rapid first aid is required for conditions like massive bleeding, open pneumothorax, and fractures. For extensive burns, establishing an intravenous access for fluid resuscitation should occur as soon as possible. If intravenous access is not available on site, oral intake of salt-containing fluids is recommended to avoid simple large-volume water ingestion.
Transport
After on-site first aid, timely transfer to a medical facility is necessary. The wound should be covered with dressings, clean cloth, or sheets to prevent contamination and minimize further tissue damage during transport. For severe burns, airway patency should be ensured, and early endotracheal intubation or tracheostomy may be required. Patients with burns covering 20% to 50% or more of total body surface area (TBSA) should be sent as early as possible to specialized burn centers. During transport, active fluid resuscitation and anti-shock treatment are important.
Early In-Hospital Treatment
Early Treatment for Mild Burns
General care involves calming the patient and carefully assessing the burn condition. Patients experiencing significant pain may receive sedatives and analgesics. Tetanus antitoxin should be administered intramuscularly, along with oral or intravenous fluid supplementation.
Initial wound care includes shaving hair around the wound, cleaning surrounding healthy skin, and disinfecting the wound with sterile water or antiseptics such as 0.5% to 1% povidone-iodine. Dirt or foreign bodies should be gently removed with gauze or tweezers. Intact blisters may be aspirated, retaining the blister roof, while contaminated or dirty blister roofs should be removed. After cleaning and disinfecting, dressing the wound is preferred during early burn stages unless the burn is confirmed as third-degree or difficult to dress. Wounds in areas like the perineum, which are hard to dress, may be treated with semi-exposure or exposure techniques, while third-degree wounds are typically treated with iodine tincture followed by exposure.
Early Treatment for Moderate to Severe Burns
General care requires gathering information on the patient’s general condition, injury history, and past medical history; monitoring vital signs such as temperature, blood pressure, pulse, respiration, and heart rate; performing simple wound cleaning; and accurately assessing and documenting burn sites, area, and depth. It is important to check for signs of poisoning, inhalation injury, or combined trauma. Maintaining airway patency is critical, with tracheal intubation or tracheostomy performed if needed. Oxygen or ventilator support is provided in cases of hypoxia. Intravenous access should be rapidly established, with arterial and/or central venous catheterization and PiCCO monitoring as necessary to assess blood volume. Tetanus antitoxin and analgesics should be administered. Laboratory tests including blood gas analysis, complete blood count, electrolytes, liver function, urea nitrogen, creatinine, blood typing, and screenings for HIV, hepatitis C, and syphilis should be performed. A urinary catheter should be placed, monitoring for hemoglobinuria, myoglobinuria, or hematuria. When necessary, bronchoscopy with electronic fiber optic devices and CT scans may be conducted.
Further treatment planning depends on the area and depth of second- and third-degree burns and patient weight, including fluid resuscitation and organ protection strategies. The systemic stress and inflammatory response is a major pathological mechanism in severe burns and directly affects disease progression, complications, outcomes, and prognosis. Early prevention and management of systemic stress responses are crucial and include blocking neuroendocrine stress pathways, preventing oxidative stress, providing analgesia and sedation, and controlling excessive inflammatory responses to prevent or lessen systemic stress.
Based on wound conditions, dressing, semi-exposure, or exposure therapies are selected. Topical medications with infection-preventing and wound-healing-promoting properties are applied. For circumferential, constrictive eschars or wounds with high sub-eschar tension, timely escharotomy is indicated. Once the condition stabilizes, early wound debridement or other interventions are performed.
Burn Shock
Severe burns cause stress and inflammatory responses that increase vascular permeability, allowing small molecules to leak from blood vessels into surrounding tissues. This results in a reduction of the effective circulating blood volume and insufficient perfusion of tissues and organs, resembling the occurrence and development of hypovolemic shock, hence it is called burn shock. The occurrence and severity of burn shock are closely related to the severity of the burn; larger burn areas and deeper burns are more likely to result in shock, and the shock tends to be more severe. Unstable progression through the shock phase is often associated with inadequate or improper fluid replacement, delayed fluid therapy, or long-distance transport. The prevention and treatment of burn shock are among the most important early therapeutic measures for severe burns. Failure to restore blood volume promptly and effectively can lead to ischemic and hypoxic tissue damage, worsening of the wound, organ dysfunction, reduced immune function, and consequently influence the course and prognosis of the disease.
Clinical Manifestations and Diagnosis of Burn Shock
The clinical manifestations of burn shock are similar to those of other hypovolemic shocks, including changes in consciousness, increased heart rate, decreased blood pressure, reduced urine output, hemoconcentration, and elevated lactate levels.
Prevention and Treatment of Burn Shock
Fluid resuscitation is the primary measure for preventing and treating burn shock. Due to damage to superficial veins or poor venous return after severe burns, deep vein catheterization—such as via the subclavian, external jugular, or femoral veins—is commonly used to ensure rapid and effective fluid resuscitation. Other supportive treatments include analgesia, sedation, and maintaining body temperature.
Various fluid resuscitation protocols exist for burn shock. The fluid replacement schemes include:
- Adult burn shock fluid resuscitation: In the first 24 hours after burn, the fluid loss is calculated based on 1 ml balanced salt solution and 0.5 ml colloid solution per 1% total body surface area (TBSA) of second- and third-degree burns per kilogram of body weight, plus a basal fluid volume of 2000 ml (5% glucose solution). Half of the calculated fluid loss is administered within the first 8 hours after injury, and the remaining half within the subsequent 16 hours. During the second 24 hours after injury, half the amount of fluid given during the first 24 hours is evenly infused, with the basal fluid volume remaining unchanged.
- Pediatric burn shock fluid resuscitation: Considering the unique physiological development at different pediatric ages, fluid resuscitation during the burn shock phase is typically divided based on whether the child is older than 2 years or not. Within the first 24 hours, half of the calculated fluid loss is administered in the initial 8 hours, with the remaining half given over the next 16 hours; basal fluids are infused evenly throughout all fluid replacement periods. Fluids during the second 24 hours after injury should also be infused evenly.
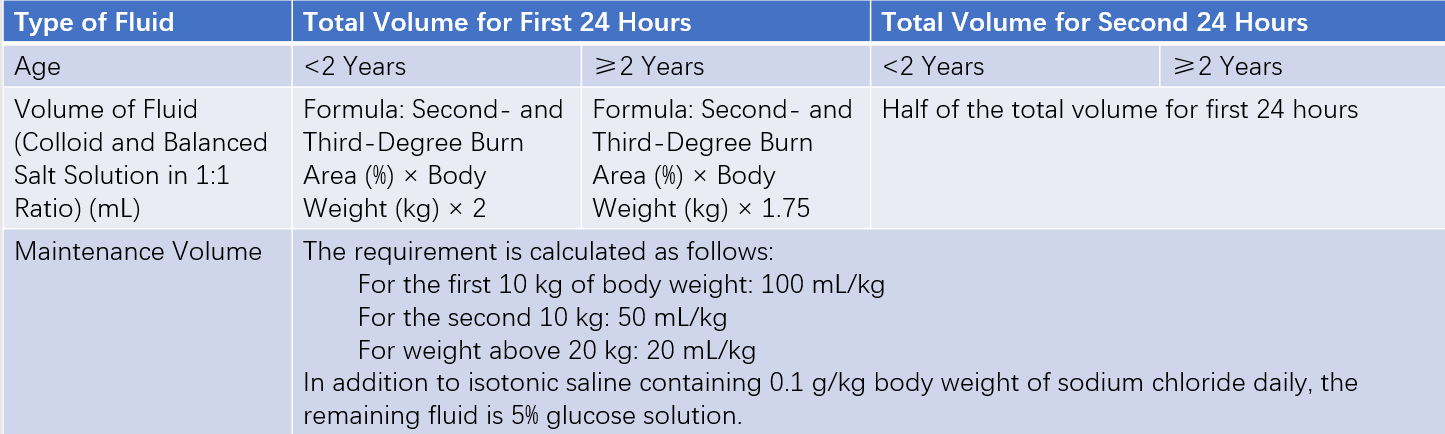
Table 3 Fluid resuscitation protocol for pediatric burns
Considerations in Burn Shock Fluid Resuscitation
All formulas provide only estimated starting points for fluid volumes and infusion rates. Actual fluid replacement should be adjusted promptly according to the patient's clinical presentation and changes following fluid therapy, including the rate and proportion of electrolyte solutions and colloids. Balanced electrolyte solutions such as lactated Ringer’s solution or acetate-based balanced solutions are generally selected; bicarbonate-balanced fluids can be prepared by mixing 0.9% sodium chloride solution with 1.25% isotonic sodium bicarbonate solution at a 2:1 volume ratio. Fresh frozen plasma is typically chosen as the colloid fluid.
Both excessively slow and excessively rapid infusion rates may lead to insufficient or excessive fluid replacement, worsening shock and tissue injury. Urine output is a critical indicator during shock resuscitation, with adult urine output ideally maintained at 0.5–1.0 ml/kg/h and pediatric urine output at 1.0–1.5 ml/kg/h. Assessment of shock treatment efficacy should be performed every 1–2 hours, and infusion rates may be adjusted up or down by 10%–20% based on the evaluation.
Systemic Infection in Burns
Burns damage the skin barrier function, and the wound’s large amount of necrotic tissue provides an ideal culture medium for microorganisms. Meanwhile, stress, inflammation, metabolic disorders, and immune suppression combined with intestinal flora imbalance make burn patients highly susceptible to infection. Infection is the most common complication of burns and the leading cause of mortality in burn patients. Effective prevention, early diagnosis, and rational treatment are crucial for managing systemic infections in burns. Burn infections can be categorized into local infections, common systemic infections, severe systemic infections (sepsis), and infectious shock (septic shock). The difference between sepsis and severe systemic infection is that sepsis involves organ dysfunction or impairment; infectious shock differs from sepsis mainly in requiring vasoactive drugs to maintain blood pressure and/or blood lactate levels above 2.0 mmol/L.
Effective Prevention
Timely Elimination and Prevention of Infection Sources
The wound is the primary source of infection and necrotic tissue such as eschar should be removed early and the wound sealed and repaired. Prevention and treatment of shock and reduction of intestinal ischemia and hypoxia injury should be emphasized. Early enteral nutrition can prevent gut-derived infections. Respiratory tract, vascular catheter, urinary tract, and other sources of infection should be actively prevented, as well as catheter-related bloodstream infections.
Prophylactic Use of Antibiotics
Small-area superficial burns generally do not require systemic antibiotics. Early prophylactic systemic antibiotics are also not recommended for large-area deep burns. Systemic antibiotics should be considered during large-area eschar removal, perioperative periods, or when infection is suspected.
Sterile Wound Management
Dressings, bedding, and items contacting the wound must be sterilized. Staff should wash hands or wear sterile gloves before and after touching the wound. Attention should be paid to sterile procedures and waste handling.
Meticulous Nursing Care
Frequent repositioning should be performed to fully expose the wound, avoid prolonged pressure, and keep eschar and scabs dry and intact. Strict management of all catheters (endotracheal tubes, invasive monitoring lines, urinary catheters) is necessary. Psychological monitoring and treatment should be addressed.
Other Measures
Nutritional therapy should meet the body's high metabolic demands, with detailed recording of intake/output and calories. Maintenance of internal environment stability, prevention and treatment of visceral complications, and symptomatic treatments are important.
Early Diagnosis
Close monitoring of vital signs, inspection of the wound and surrounding tissues, and laboratory tests including blood routine, procalcitonin, interleukin-6 (IL-6), C-reactive protein (CRP), endotoxin, G test, GM test, chest X-rays, microbial cultures, drug susceptibility testing, and metagenomic next-generation sequencing (NGS) should be conducted promptly to detect and diagnose burn infections.
Rational Use of Antibiotics
When infection is suspected but the pathogen is unclear, empirical use of dual or triple high-efficiency broad-spectrum antibiotics is common based on microbial prevalence and clinical presentation. After identifying the microorganism, antibiotic therapy should be adjusted to sensitive agents.
Timely Removal of Infectious Foci
Once an infection source on a specific wound or lesion is confirmed and the patient’s overall condition permits, timely removal of the infectious focus is indicated.
Other Treatments
Alongside removal of the infection focus and rational use of targeted antibiotics, maintenance of water, electrolyte, and acid-base balance is important. Symptomatic and supportive therapies, correction of metabolic disorders, nutritional and immunological treatments should be provided. Continuous blood purification treatments, such as high-energy continuous renal replacement therapy (CRRT), may be applied if necessary to remove bacterial toxins and inflammatory mediators.
Prevention and Treatment of Common Visceral Complications
Renal Dysfunction
Renal dysfunction is one of the most common complications following severe burns. The main pathogenic factors include ischemic-hypoxic injury, inflammatory responses, obstruction of renal tubules by coagulated hemoglobin/myoglobin, infections, toxicity, and medications. Prevention can be aimed at these related causes, such as timely and effective fluid resuscitation to prevent ischemic-hypoxic damage, urine alkalinization, infection control, and rational drug use. Once renal dysfunction occurs, prompt diagnosis, removal of causative factors, maintenance of water, electrolyte, and acid-base balance to stabilize the internal environment, appropriate use of diuretics, renal protection, and promotion of renal injury repair are necessary. Early initiation of continuous renal replacement therapy (CRRT) may be required if needed.
Pulmonary Complications
Pulmonary complications include ARDS, infections, pulmonary edema, and atelectasis, which mostly occur within two weeks after injury and are related to inhalation injury, shock, and infection. Prevention of pulmonary complications after burns primarily focuses on addressing the main causes through airway management, lavage, drainage, etc. The prone position is beneficial for the prevention and treatment of pulmonary complications. Early diagnosis and treatment are also important. Fiberoptic bronchoscopy serves not only as a diagnostic tool for airway injury but also as a precise route for drainage, lavage, and medication administration in the treatment of pulmonary infections and other complications.
Stress Ulcers of the Digestive Tract
The main mechanism of stress ulcer formation after severe burns involves vasoconstriction in the digestive tract and a reduction in effective circulating volume, leading to ischemic-hypoxic damage. The primary preventive measures include timely restoration of effective circulating volume and the use of acid-suppressive agents and other gastroprotective drugs. Symptoms such as unexplained abdominal pain, acute anemia, melena, or even hematochezia following severe burns should raise suspicion for stress ulcers. Once diagnosed, treatment includes red blood cell supplementation, volume expansion, fasting, local hemostatic agents in the digestive tract, and proton pump inhibitors. If these measures are ineffective, gastroscopy for diagnosis and hemostasis or angiography with interventional hemostasis may be considered. Surgical treatment is required if bleeding remains uncontrolled or perforation occurs.
Cerebral Edema
Children with severe burns are prone to developing cerebral edema. The causes include ischemic-hypoxic injury or excessive administration of hypotonic fluids over a short period causing intracellular cerebral edema, as well as excessive or rapid fluid resuscitation causing interstitial cerebral edema. Other causes include toxicity, metabolic disorders, severe infection, and combined traumatic brain injury. Early symptoms of cerebral edema include nausea, vomiting, drowsiness, tongue retraction, snoring, or sluggish responsiveness; some cases may present with irritability or agitation. Children may exhibit seizures and high fever; severe cases may develop arrhythmias, irregular breathing or apnea, coma, and even sudden death due to brain herniation. Once cerebral edema occurs, timely identification of the cause and targeted emergency treatment are necessary.
Wound Management
Debridement
Debridement is the primary step in wound treatment, which includes removal of hair around the wound, cleaning, and disinfection. Early debridement is preferred for mild to moderate burns, while for severe burns it should be performed after effective fluid resuscitation, with appropriate analgesia or anesthesia as needed. Clean and intact blisters can be preserved or have their fluid aspirated while keeping the blister roof; severely contaminated eschars should be removed. Early treatment of superficial burn wounds generally involves dressing, while third-degree wounds are preferably treated with exposure.
Treatment of Superficial Burn Wounds
Superficial burn wounds are generally defined as those without infection or pressure, capable of self-healing. These include first-degree wounds, superficial second-degree wounds, deep second-degree wounds, and some mixed-depth wounds. Treatment of first-degree wounds focuses on pain relief and prevention of further injury, such as early cold therapy and keeping the wound clean and dry later. For superficial and deep second-degree wounds, besides pain management, dressing or semi-exposure treatments help maintain the optimal microenvironment, prevent infection, and promote healing. Early cooling followed by dressing is usually applied; if infection occurs, cleaning and debridement are necessary along with topical antimicrobials and systemic antibiotics when required. Functional rehabilitation of the affected area is emphasized during wound treatment.
Dressing Therapy
Dressing therapy is the main clinical treatment method for burn wounds. After wound cleaning, debridement, and disinfection, a single layer of sterile medical gauze/oil gauze/non-adherent gauze containing topical antibacterial or wound-healing promoting agents, or other biological/artificial dressings, is evenly applied and covered with sterile gauze (about 2–3 cm thick) under uniform pressure. The dressing should extend 3–5 cm beyond the wound edge. Dressings are generally changed every 1–2 days, or more frequently if exudate is excessive.
Semi-exposure Therapy
After wound cleaning, debridement, and disinfection, only a single layer of gauze/oil gauze/non-adherent gauze containing topical antibacterial or wound-healing promoting agents or other biological/artificial dressings is applied directly on the wound without additional dressings.
Exposure Therapy
Exposure therapy is mainly used for preoperative treatment of third-degree burn wounds. After cleaning and disinfecting the wound, tincture of iodine or astringent herbal preparations are applied, leaving the wound exposed to air so that exudate and necrotic tissue dry and form a scab for temporary protection. Tincture of iodine is typically applied twice daily and forms a dry scab within 48 hours. Frequent repositioning is necessary to prevent prolonged pressure on the wound. If infection occurs under the scab, timely removal of the infected focus is required.
Treatment of Deep Burn Wounds
Deep burn wounds generally refer to wounds that cannot heal on their own, including deep partial-thickness (deep second-degree) burns and third-degree burns. Early treatment of deep partial-thickness wounds usually involves dressing to prevent wound deepening and to promote self-healing. After 3 to 5 days, dressing, semi-exposure, or exposure therapy may be applied. Third-degree wounds can be treated early with iodine tincture application followed by exposure therapy. For patients with deep burns covering 10% to 30% of the body surface area and who have stable hemodynamics and overall condition, early one-time escharotomy surgery to remove necrotic tissue and timely autologous skin grafting is often pursued. For patients with large burns covering 50% to 80% of the body surface, if systemic conditions allow, large-area escharotomy (excision or dermabrasion) can be performed during the shock phase or after stabilization. For those with burns exceeding 80%, large-area escharotomy should be done as soon as possible once the shock phase has passed and hemodynamics are stable. After extensive eschar removal, skin grafting methods such as sheet grafts, mesh grafts, stamp grafts, MEEK micrografts, or minced skin grafts may be arranged in one or two stages depending on the wound and available autologous skin.
Dermabrasion refers to the precise mechanical or hydrodynamic removal of necrotic and degenerated tissue layer by layer after wound disinfection in the early burn phase, aiming to preserve healthy or even sub-epidermal tissue as much as possible. After dermabrasion, a single layer of gauze, oil gauze, or non-adherent gauze containing topical antimicrobial and wound healing-promoting agents, or biological/artificial dressings, is applied smoothly over the wound.
Tangential Excision involves the use of tools such as roller dermatome or hydrodynamic devices to remove necrotic tissue of deep partial-thickness wounds until healthy or near-healthy tissue is exposed. Identification of the healthy dermis during this procedure is indicated by the appearance of milky white or porcelain white tissue with dense, glossy texture, unobstructed blood vessels, and active bleeding upon release of the tourniquet. The excised wound tends to bleed considerably and requires thorough hemostasis. Tangential excision typically results in a good wound bed and is usually followed immediately by autologous skin grafting.
Escharectomy refers to the complete surgical removal of all necrotic tissue in full-thickness (third-degree) burns, including necrotic skin, subcutaneous tissue, and even muscle. Depending on the wound bed and autologous skin availability, one-stage autologous grafting with sheet, mesh, MEEK micrografts, or minced skin may be performed, or temporary coverage with allografts (homografts), xenografts, or artificial materials may be applied, followed by delayed autologous grafting once the wound bed is prepared.
Pharmacological or Enzymatic Eschar Removal employs proteolytic enzymes such as protease and collagenase, or herbal preparations like burn ointments and healing powders, applied to the burn wound to remove necrotic tissue while preserving healthy tissue as much as possible.
Natural Eschar Separation is mainly used for small-area or special-location deep burns in patients unwilling or unable to undergo surgery. Maintaining a moist wound environment facilitates gradual natural eschar dissolution, detachment, and separation, generally requiring more than 3 to 4 weeks. Newly formed granulation tissue appears after eschar separation, which should be followed by early autologous skin grafting for wound repair.
Prevention and Management of Wound Infection
Prevention involves enhanced aseptic management, regular repositioning to avoid prolonged pressure, timely cleaning, and debridement with local use of anti-infective drugs such as 1% silver sulfadiazine cream or 0.5%–1.0% povidone-iodine solutions or dressings. Intact eschar should be kept complete and dry. When autologous skin grafting cannot be performed immediately, temporary coverage with allografts, artificial materials, or others is considered until the wound bed is ready for grafting.
Treatment of Infected Wounds requires early thorough cleaning, debridement, and drainage, with local application of anti-infective drugs or dressings. When invasive wound infections cause systemic infection, surgical debridement should be performed as soon as possible, conditions permitting, to reduce bacterial and toxin entry into the bloodstream and help control systemic infection.
Treatment of Fungal Wound Infections often presents as black eschar or scattered gray-white or dark fungal colonies or mold spots and necrotic areas on semi-exposed gauze surfaces. Severe mucormycosis or aspergillosis infections causing vascular thrombosis may lead to rapidly progressive wound deepening with cheesy or curd-like necrosis, involving deep muscle necrosis and/or distal limb necrosis. Once invasive fungal infection is confirmed, especially with aspergillus or mucor species, aggressive and thorough removal of infected tissue, including possible amputation, is performed. Local antifungal drugs are applied after thorough irrigation, and systemic antifungal therapy is administered as needed.
Burn Prevention
Burns are preventable. Current main measures for burn prevention include: (1) actively conducting public education to raise awareness of the social and familial harm caused by burns and their preventability, thereby enhancing overall disaster awareness and preventive education; (2) strengthening fire prevention education in daily life, including fire knowledge and escape training, as well as the use of various firefighting equipment; (3) promoting knowledge of self-rescue, mutual aid, and immediate cold therapy after burns; (4) emphasizing enhanced safety education and strict fire management and burn rescue plans in high-risk occupations and enterprises; (5) fully utilizing the roles of firefighters and specialized burn medical personnel in burn prevention education.