Sepsis refers to life-threatening organ dysfunction caused by a dysregulated host response to infection and often arises from severe surgical infections. When sepsis is accompanied by profound circulatory dysfunction and metabolic disturbances, it is referred to as septic shock, which carries a significantly higher mortality risk than sepsis alone.
Etiology
Sepsis is predominantly caused by high bacterial loads, virulent pathogens, and weakened immune responses. It commonly follows infections secondary to severe trauma or pyogenic conditions, such as extensive burn wound infections or acute diffuse peritonitis. Individuals with compromised immunity are particularly prone to sepsis upon the occurrence of pyogenic infections. Additionally, a few potential routes of infection warrant attention:
Catheter-Related Infections (CRIs)
Intravenous catheters, especially central venous lines, can become conduits for direct pathogen entry into the bloodstream if not properly cared for or left in place for prolonged durations. Once an infection site forms, it can serve as a reservoir for the continuous dissemination of pathogens and toxins throughout the body.
Gut-Derived Infections
The gut serves as the body's largest reservoir of bacteria and endotoxins. Under healthy conditions, the intestinal mucosa functions as a robust barrier. However, in critically ill patients with impaired or failed gut barrier function, intestinal pathogens and endotoxins may translocate across the gut lining and cause gut-derived infections.
Currently, sepsis caused by gram-negative bacteria occurs at significantly higher rates than gram-positive bacterial sepsis. Additionally, the ongoing use of antibiotics has led to the emergence of previously lesser-known opportunistic pathogens, such as Acinetobacter baumannii and Stenotrophomonas maltophilia. Opportunistic fungal infections also require particular attention.
Clinical Manifestations
Key clinical features of sepsis include:
- Fever and Chills: Patients commonly present with fever and chills.
- Tachycardia and Tachypnea: Increased heart rate, weak pulse, and rapid or labored breathing are often observed.
- Mental Status Changes: Altered mental states—including lethargy, agitation, delirium, or even coma—may occur.
- Hepato-Splenomegaly and Rashes: Enlargement of the liver and spleen or the appearance of skin rashes may also present.
Sepsis caused by different pathogens exhibits distinct characteristics:
- Gram-Negative Bacterial Sepsis: Frequently secondary to abdominal infections or extensive burn wound infections, gram-negative bacterial sepsis tends to be particularly severe. It may present with the "three lows" phenomenon: hypothermia, leukopenia, and hypotension. The incidence of septic shock is high in these cases.
- Gram-Positive Bacterial Sepsis: Often secondary to conditions such as severe abscesses or cellulitis, gram-positive bacterial sepsis is commonly associated with Staphylococcus aureus. It tends to cause high fever, rashes, and metastatic abscess formation.
- Anaerobic Bacterial Sepsis: Anaerobic bacteria frequently form mixed infections with aerobic bacteria and are commonly implicated in sepsis secondary to abscesses or perineal infections. Severe tissue necrosis at the infection site and a characteristic foul odor are often present.
- Fungal Sepsis: Typically arising from prolonged use of broad-spectrum antibiotics or immunosuppressants, fungal sepsis may present with embolic phenomena such as conjunctival petechiae or focal cotton-wool spots in the retina.
Diagnosis
Sepsis is diagnosed using the Sequential Organ Failure Assessment (SOFA) score, which evaluates sepsis-related organ dysfunction. However, because SOFA scoring involves complex calculations and requires laboratory tests, the quick SOFA (qSOFA) is commonly employed for preliminary evaluation in patients with suspected infection. A qSOFA score of ≥2 suggests that further evaluation with the full SOFA score is indicated.
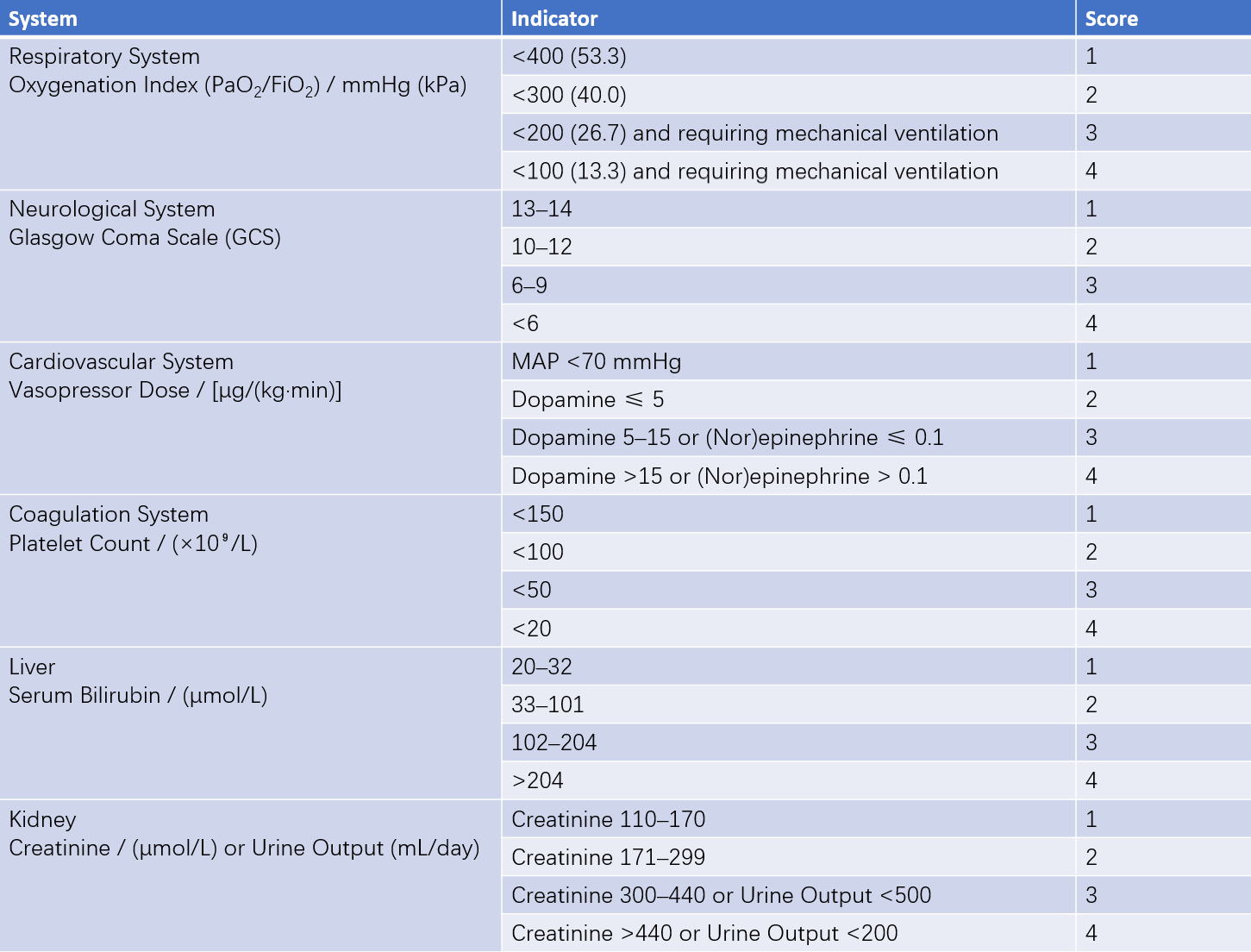
Table 1 SOFA scoring table
An infection leading to an increase in the SOFA score of ≥2 points relative to baseline indicates organ dysfunction and defines sepsis. If a septic patient requires vasopressors to maintain a mean arterial pressure of ≥65 mmHg after adequate fluid resuscitation, combined with a serum lactate level >2 mmol/L, the condition is defined as septic shock.
The identification of causative pathogens is crucial for the confirmation and treatment of sepsis. Blood samples should ideally be collected before initiating antibiotic therapy, provided this does not delay treatment. In patients with catheterization exceeding 48 hours, catheter samples should be submitted for testing if catheter-related infection is suspected. For patients with multiple negative blood cultures, anaerobic or fungal sepsis should be considered, and additional relevant tests should be conducted. Cultures of pus or aspirated fluid may also aid in identifying pathogens.
Treatment
According to the 2021 International Guidelines for the Management of Sepsis and Septic Shock, treatment can be divided into the following four components:
Early Resuscitation
Patients diagnosed with sepsis or septic shock should undergo immediate fluid resuscitation. For those showing signs of sepsis-induced hypoperfusion or septic shock, a crystalloids volume of no less than 30 mL/kg is recommended within the first three hours. For septic shock patients requiring the use of vasopressors, an initial resuscitation target of a mean arterial pressure (MAP) of 65 mmHg is suggested. After completing early fluid resuscitation, further resuscitation strategies should be determined based on the patient's hemodynamic findings.
Antimicrobial Therapy
For patients with suspected septic shock or a high probability of sepsis, the administration of antimicrobial agents as soon as possible after identification is highly recommended, preferably within the first hour. For those at high risk of infection due to multidrug-resistant (MDR) organisms, combination therapy with two antimicrobial agents covering gram-negative bacteria is suggested for empirical treatment. Once the causative organism and susceptibility test results are known, targeted narrow-spectrum antibiotics are recommended.
Source Control
The primary site of infection should be identified promptly, and appropriate measures to control the infection source should be taken without delay. These include the removal of necrotic tissue and foreign bodies, elimination of dead spaces, and drainage of abscesses. Coexisting causative factors such as vascular obstruction or blockages should also be managed as needed. For catheter-related infections, removal of the catheter is considered a priority.
Additional Supportive Treatments
After successful early resuscitation, the patient’s hemodynamic status should be reassessed, and supplemental fluid administration or vasopressor use should be adjusted accordingly. For septic shock patients requiring continuous vasopressor support, intravenous hydrocortisone (200 mg/day) may be administered. Blood transfusion is recommended when hemoglobin levels drop below 70 g/L. For sepsis patients without acute respiratory distress syndrome (ARDS), the use of low tidal volume (6 mL/kg) ventilation is suggested. Insulin therapy should be provided to those with hyperglycemia to maintain blood glucose levels below an upper limit of 10 mmol/L. In patients without contraindications, the prophylactic use of low molecular weight heparin (LMWH) for preventing venous thrombosis is recommended. For patients at risk of gastrointestinal bleeding, prophylaxis for stress ulcers is advised. For patients who can tolerate enteral nutrition, initiating enteral feeding at an early stage of treatment is recommended.