Etiology and Pathology
Paronychia refers to a purulent bacterial infection of the paronychial tissue along the sides of the fingernail or toenail. It is often caused by minor injuries, blunt trauma, hangnail removal, or overly deep nail trimming. Felon, or purulent infection of the pulp of the fingertip or toe, occurs in the subcutaneous tissue of the distal phalanx and is often the result of exacerbation of paronychia or direct skin trauma.
Clinical Manifestations
Paronychia
The infection usually begins on one side of the paronychial region, presenting initially with localized redness, swelling, warmth, and pain. Once suppuration occurs, a white purulent spot and fluctuance become noticeable under the paronychial skin, though spontaneous rupture is unlikely. The infection may spread to the nail root or the opposite side, forming a semi-circular abscess. If the abscess extends beneath the nail, it can develop into a subungual abscess. Severe cases involve intense pain, fever, and other systemic symptoms. Delayed treatment may lead to chronic paronychia or chronic osteomyelitis of the distal phalanx.
Felon (Purulent Finger/Toe Infection)
Early symptoms include a pricking pain and mild swelling of the affected finger or toe, which progressively worsen with increased swelling and severe throbbing pain. Fever, general malaise, and elevated white blood cell counts may accompany the infection. In advanced cases, compression of sensory nerve endings can cause numbness and temporary relief from pain, indicating local ischemia and necrosis. The skin may change from red to pale. If osteomyelitis of the distal phalanx develops, complications such as skin rupture, persistent purulent discharge, bone necrosis, and a chronic non-healing wound may occur.
Prevention and Treatment
For paronychia without suppuration, treatment involves the application of antibiotic ointments, warm compresses with acriflavine solution, potassium permanganate warm baths, or physical therapies such as ultra-short waves or infrared light. Oral administration of sensitive antibiotics is also indicated. If an abscess forms, early surgical intervention is required, with a longitudinal incision along the side of the paronychial region for drainage. Subungual abscesses may necessitate partial or complete removal of the fingernail or toenail, with careful protection of the nail bed during surgery to preserve nail regrowth.
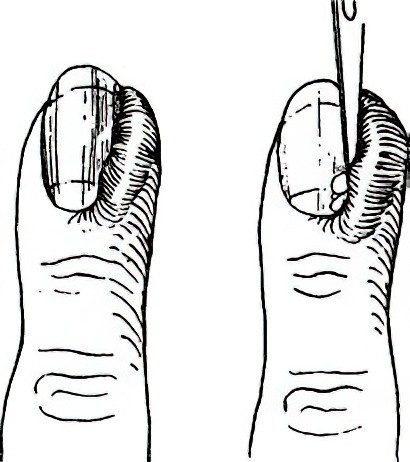
Figure 1 Paronychia and incision for drainage
In the early stages of felon, affected fingers or toes should remain elevated, and treatment includes systemic antibiotics and warm wet compresses with acriflavine solution. Severe cases presenting with intense pain, significant swelling, and systemic symptoms require prompt incision and drainage to prevent complications such as bone necrosis and osteomyelitis.
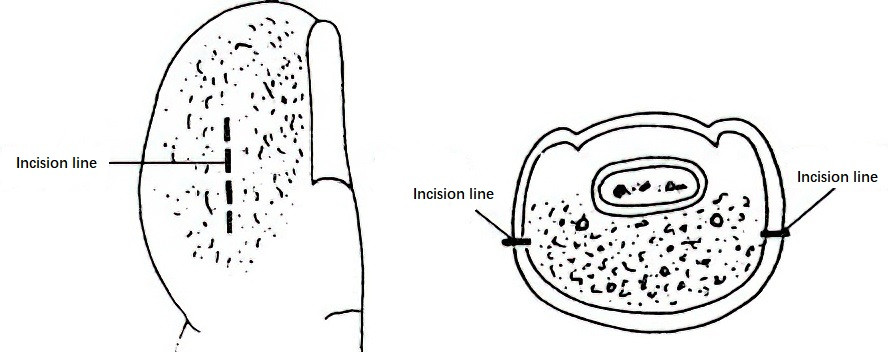
Figure 2 Felon and incision lines
Regional anesthesia via a digital nerve block or general anesthesia is preferable. Local infiltration anesthesia near the site of infection is avoided to prevent spread. A longitudinal incision is typically made along the lateral side of the affected fingertip or toe, extending no farther than half the width of the nail bed distally and no farther than the flexion crease of the distal interphalangeal joint proximally. Subcutaneous fibrous septa are divided and detached to allow thorough drainage. Larger abscess cavities may require counter-incisions for adequate drainage, and sequestra or necrotic bone fragments must be removed when present. The use of fish-mouth incisions is avoided to prevent scarring that could impair functionality post-healing.