The surgical treatment of obesity and metabolic diseases began in the 1950s. Over the past 70 years, numerous procedures that involved complex techniques, significant trauma, suboptimal outcomes, or high rates of complications have gradually been phased out. Procedures that are both safe and effective have been increasingly promoted and implemented.
Surgical Indications
Surgical indications include:
- Body Mass Index (BMI) ≥ 32.5 kg/m2.
- BMI between 27.5–32.49 kg/m2, accompanied by two or more metabolic or obesity-related conditions that cannot be effectively controlled through lifestyle modifications or pharmacological treatment.
Contraindications to Surgery
There are no absolute contraindications to surgery. Relative contraindications include:
- Severe substance or alcohol addiction.
- Severe intellectual disabilities or severe psychiatric illnesses.
- Inability to adhere to postoperative dietary and lifestyle changes.
- Poor general health with significant functional impairments of major organs, making tolerance to general anesthesia or surgery difficult.
- Advanced cancer, decompensated portal hypertension due to liver cirrhosis, large abdominal wall hernias, or severe intra-abdominal adhesions.
Additionally, a growing body of evidence suggests that weight-loss surgery can yield favorable outcomes for obese children, adolescents, and elderly individuals. However, surgery for these groups requires careful multidisciplinary evaluation prior to proceeding.
Preoperative Preparation
Thorough preoperative evaluation and preparation can enhance the safety and efficacy of surgery.
Multidisciplinary evaluation is performed preoperatively, involving specialists from metabolic and bariatric surgery, anesthesiology, endocrinology, nutrition, cardiology, pulmonology, gastroenterology, psychiatry, and psychology. Surgical indications should be confirmed, the appropriate surgical approach determined, and the risks and potential effects of the procedure evaluated.
For high-risk patients with a BMI > 50 kg/m2 or functional organ failure, conservative treatment is advised preoperatively to reduce body weight by more than 5% and improve organ function before elective surgery is scheduled.
Surgical Techniques
Weight-loss procedures achieve their effects either by reducing the effective volume of the stomach and altering gastrointestinal hormone levels to suppress hunger and reduce food intake, or by shortening the functional length of the small intestine to decrease nutrient digestion and absorption. Weight-loss surgeries can be categorized into restrictive (stomach volume reduction) procedures, malabsorptive small-intestinal procedures, and mixed procedures. Although malabsorptive procedures are effective, they often result in significant postoperative nutritional complications and are now less commonly used, primarily as revision surgeries.
The primary surgical techniques currently in use include sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), one-anastomosis gastric bypass (OAGB), and malabsorptive procedures like biliopancreatic diversion with duodenal switch (BPD/DS) and single-anastomosis duodenal ileal bypass with sleeve gastrectomy (SADI-S). Among these, the first two are the most commonly performed.
Sleeve Gastrectomy (SG)
This procedure involves completely mobilizing the greater curvature of the stomach and the gastric fundus. A 32–40F bougie is inserted orally to guide the procedure. The gastric greater curvature is resected using a stapler, starting 2–3 cm from the pylorus, extending upward. The gastric fundus is entirely excised, creating a tubular stomach along the lesser curvature with a volume of 60–80 ml.
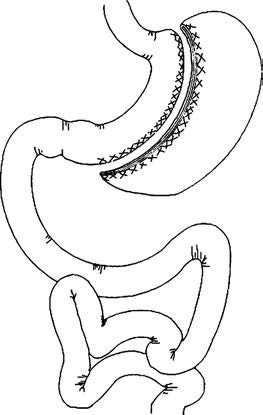
Figure 1 Sleeve gastrectomy
Outcomes
Sleeve gastrectomy demonstrates significant weight-loss effects and can be performed as a standalone procedure. It can also serve as a first-stage surgery for patients with extreme obesity (BMI > 50 kg/m2). After one year, patients typically achieve an excess weight loss of 60–70%, with Type 2 Diabetes Mellitus (T2DM) remission rates of approximately 65%.
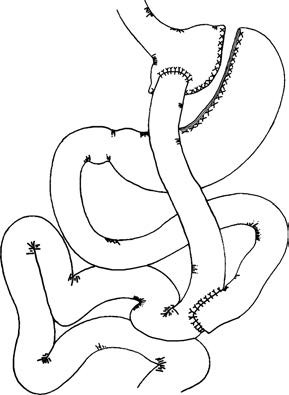
Roux-en-Y Gastric Bypass (RYGB)
This surgery involves creating a proximal gastric pouch with a volume of 10–20 ml, leaving the distal stomach in place. The jejunum is transected 25–100 cm below the ligament of Treitz. The distal jejunum (alimentary limb) is connected to the gastric pouch via a gastrojejunostomy with an anastomotic diameter of 1.0–1.5 cm. The biliopancreatic limb (proximal jejunum) is connected to the alimentary limb 100–175 cm downstream through a side-to-side anastomosis. Mesenteric defects are closed to prevent internal hernias.
Figure 2 Roux-en-Y gastric bypass
Outcomes
Roux-en-Y gastric bypass effectively improves glucose metabolism and other metabolic disorders. After one year, excess weight loss ranges from 70–80%, with T2DM remission rates between 80–85%.
Emerging Techniques
Endoscopic weight-loss procedures are also being explored and applied, including techniques like intragastric balloon placement and endoscopic sleeve gastroplasty (ESG).
Complications
Overall, the complication rate for weight-loss surgery is relatively low. However, prevention, early diagnosis, and timely treatment remain important considerations.
Gastrointestinal Leakage
The incidence ranges from 0–7.0% and often occurs at the gastrojejunal anastomosis or the proximal remnant stomach near the angle of His. Contributing factors include insufficient blood supply, inadequate sutures, and preexisting conditions such as diabetes. Clinical manifestations include peritonitis, tachycardia, and fever. Upon confirmation of the diagnosis, treatments such as fasting, gastrointestinal decompression, acid suppression, anti-infective therapy, and nutritional support are typically implemented. If conservative management is ineffective, endoscopic interventions or, in some cases, additional surgery may be required.
Bleeding
The incidence ranges from 0.1–4.4% and is associated with the use of anticoagulants or nonsteroidal drugs during the perioperative period, improper intraoperative handling, or severe postoperative vomiting. Clinical signs include hypotension and tachycardia. Prevention of postoperative bleeding relies on precise surgical technique and multidisciplinary coordination during the perioperative period. Thorough intraoperative inspection of anastomoses and resection margins is critical. Once diagnosed, appropriate interventions must be performed based on the severity of the bleeding.
Malnutrition
Malnutrition may occur due to reduced food intake and/or absorption. Common deficiencies include protein, vitamin D, folate, vitamin B12, iron, and calcium. Severe vitamin B1 deficiency can lead to Wernicke encephalopathy, characterized by oculomotor paralysis, mental disturbances, and ataxia.
Gastroesophageal Reflux
A minority of patients may experience gastroesophageal reflux after sleeve gastrectomy. Potential causes include the disruption of the angle of His and surrounding structures as well as reduced lower esophageal sphincter tone. Additionally, a hiatal hernia markedly increases the likelihood of reflux. For patients with a concurrent hiatal hernia, repair of the hernia is often performed during sleeve gastrectomy.
Other complications include venous thromboembolism, anastomotic or gastric margin ulcers, dumping syndrome, internal hernias and bowel obstruction, gallstones, and hypoglycemia. Overall, the incidence of these complications is relatively low.
Postoperative Management
Weight-loss surgery is not a one-time solution, and effective postoperative management is essential to achieve optimal long-term outcomes.
Postoperative diet transitions typically follow a progression from a full-liquid diet to a semi-liquid diet, then to soft foods, and finally to a regular diet.
Regular follow-up visits and assessments are recommended to monitor progress. Smoking and alcohol consumption should be avoided. Adequate supplementation of vitamins and minerals such as iron and calcium is recommended as needed, along with sufficient protein intake. Excessive consumption of carbohydrates and fats should be avoided.
Healthy habits, including appropriate physical activity, should be cultivated after surgery.
Long-term periodic follow-up is necessary. This includes monitoring changes in body weight, dietary and exercise habits, complications, and the remission of metabolic and obesity-related conditions. Personalized guidance and interventions may be provided based on these observations.
Efficacy Assessment
The evaluation of surgical outcomes primarily focuses on weight-loss effects and the improvement of metabolic and obesity-related conditions.
Weight-Loss Effects
The percentage of total weight loss (%TWL) and the percentage of excess weight loss (%EWL) are used to assess postoperative weight loss. The formulas are as follows (with ideal weight defined as the weight corresponding to a BMI of 25 kg/m2):
%TWL = [(Preoperative weight - Follow-up weight) / Preoperative weight] × 100%
%EWL = [(Preoperative weight - Follow-up weight) / (Preoperative weight - Ideal weight)] × 100%
Generally, %EWL > 50% is considered a successful outcome, %EWL between 25–50% reflects suboptimal results, and %EWL < 25% indicates ineffective results (failure to meet expected outcomes).
Resolution of Comorbidities
The effectiveness of treating comorbidities such as diabetes, hypertension, and hyperlipidemia is assessed according to relevant medical guidelines. For Type 2 Diabetes Mellitus (T2DM), evaluation criteria are as follows:
- Complete Remission: Blood glucose levels (fasting glucose, postprandial glucose, glycated hemoglobin) return to normal without the use of any hypoglycemic medication.
- Partial Remission: Blood glucose levels remain above the normal range but below the diagnostic threshold for diabetes, without the use of hypoglycemic medications.
- Improvement: The type or dosage of hypoglycemic medications required postoperatively is significantly reduced compared to preoperative levels, with postoperative HbA1c < 7.0%.
- Ineffectiveness: No significant changes in the type or dosage of hypoglycemic medications required, or no significant improvement in blood glucose levels compared to preoperative measures.
Revision Surgery
Revision surgery refers to a secondary surgical procedure for patients with obesity who require additional interventions after the initial weight-loss surgery due to suboptimal outcomes, postoperative weight regain, and/or the occurrence of severe complications. Revision surgery can be categorized into three types: restorative surgery (restoring normal gastrointestinal anatomy), conversion surgery (changing one procedure to another), and corrective surgery (modifying the original procedure without altering its type).
Indications for Surgery
Indications include:
- Suboptimal or ineffective weight-loss outcomes, or weight regain, with BMI ≥ 32.5 kg/m2.
- Poor or recurrent outcomes regarding treatment of obesity-related metabolic or associated diseases, with BMI ≥ 27.5 kg/m2.
- Severe postoperative complications unresponsive to conservative treatment.
Contraindications for Surgery
In addition to the general contraindications for surgery, specific contraindications for revision procedures include:
- An interval of less than 24 months since the initial surgery, except in cases of severe postoperative complications necessitating revision surgery.
- BMI < 27.5 kg/m2, except for patients requiring revision due to severe complications such as malnutrition following the initial surgery.
Preoperative Evaluation
A thorough evaluation is conducted to determine the underlying causes of the suboptimal outcomes and/or the occurrence of complications following the initial weight-loss surgery.
Comprehensive assessment of the patient's weight-loss progress, improvement of metabolic and obesity-related diseases, and postoperative lifestyle habits is performed.
A multidisciplinary team approach is employed for diagnosis and treatment, with particular attention to addressing nutrition-related and psychological issues.
Surgical Options
Revision surgery involves higher risks, greater technical difficulty, and less favorable outcomes compared to initial procedures. For these reasons, revision procedures require careful selection based on the type of initial surgery and the specific circumstances of the patient. A variety of surgical techniques are available, including repeat sleeve gastrectomy and Roux-en-Y gastric bypass, among others.