Ankylosing spondylitis (AS) is a chronic inflammatory disease that typically begins in the sacroiliac joints and gradually extends upwards along the spine. It leads to fibrous or bony ankylosis of the spine and may involve the joints of the lower limbs, ultimately resulting in deformities.
Etiology
AS falls under the category of rheumatic diseases, and its exact cause remains unclear. It is generally believed that human leukocyte antigen (HLA)-B27 is associated with the disease.
Pathology
The primary pathological change is a chronic and destructive vascularized inflammatory process, while ligament ossification represents a secondary repair mechanism. The lesions typically originate in the sacroiliac joints and slowly spread upwards along the spine. They involve the synovium and joint capsule of the intervertebral facet joints, as well as the surrounding soft tissues of the spine. In advanced stages, calcification and ossification of the surrounding soft tissues can affect the entire spine, leading to severe kyphotic deformities. The disease may also extend downwards, affecting both hip joints and, in some cases, the knee and ankle joints.
Clinical Manifestations
The disease predominantly affects young adults aged 16 to 30, with males accounting for 90% of cases. A significant familial inheritance pattern is often evident.
In the early stages, patients typically experience lower back pain, discomfort or pain in the sacroiliac region, and stiffness. Stiffness is most noticeable in the lower back upon waking or after prolonged sitting, but improves with activity. Hip joint involvement manifests as soreness and discomfort in the buttocks and groin, with pain that can radiate down to the lower limbs. Symptoms tend to worsen during rest or inactivity and improve with movement.
In approximately half of patients, inflammation of large joints in the lower extremities, such as the hip, knee, or ankle joints, serves as the initial symptom. In the later stages, severe spinal stiffness may cause the trunk and hip joints to become flexed, resulting in kyphotic deformities. Thoracic vertebrae may exhibit pronounced posterior curvature (greater than 90°), preventing the patient from maintaining a level gaze and restricting the visual field to just below the feet. Due to limited rotational movement of the cervical and lumbar spine, patients are forced to rotate their entire body for side vision. Hip joint involvement often leads to a waddling gait during ambulation.
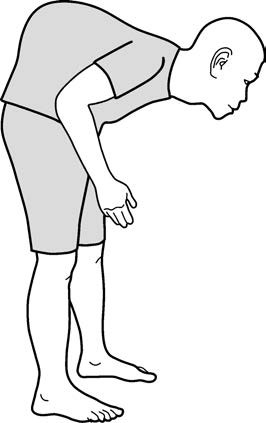
Figure 1 Kyphotic deformity in ankylosing spondylitis
In some cases, the disease originates in the cervical spine and gradually extends downward to involve the thoracic and lumbar spine. This condition, called Bechterew disease, frequently affects nerve roots, leading to upper limb paralysis and respiratory difficulties with a poorer prognosis.
Auxiliary Examinations
Laboratory Tests
Results may show elevated platelet counts, reduced hemoglobin levels, increased erythrocyte sedimentation rates (ESR), and elevated C-reactive protein (CRP). However, symptoms can be pronounced even when these indices remain normal in some patients. Rheumatoid factor is generally negative, and immunoglobulin levels may exhibit mild elevations. The positivity rate of HLA-B27 ranges from 88% to 96%.
Imaging Studies
Early X-ray findings include osteoporosis of the sacroiliac joints, with worm-eaten changes along the joint margins, irregular widening of joint spaces, and subchondral bone sclerosis. As the disease progresses, the joint surfaces become increasingly indistinct, and joint spaces gradually narrow until eventual complete fusion of the bilateral sacroiliac joints. Similar changes occur in the intervertebral facet joints, with ossification in the surrounding ligaments forming extensive "bony bridges," producing the characteristic "bamboo spine" appearance. In advanced stages, involvement of the hip and knee joints may show joint space narrowing, ultimately resulting in bony ankylosis.
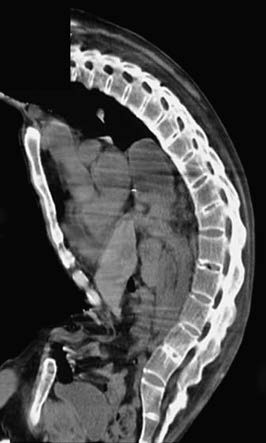
Figure 2 Bamboo spine appearance on MRI

Figure 3 X-ray showing bony ankylosis of the hip joint
CT imaging provides clearer visualization of structural changes in the sacroiliac joints compared to X-rays. MRI can reveal both acute inflammatory changes and structural alterations in the sacroiliac joints, allowing for earlier detection of sacroiliac joint involvement in AS patients.
Diagnosis and Differential Diagnosis
Diagnostic Criteria
Diagnostic criteria include:
- Chronic lower back pain lasting at least three months, with relief of pain after physical activity.
- Restricted movement in all directions of the affected spinal segment.
- Chest expansion range that is less than the normal value for the same age and gender group.
- Bilateral sacroiliitis at grade II–IV or unilateral sacroiliitis at grade III–IV.
A diagnosis of ankylosing spondylitis can be established if criterion 4 is present along with any one of criteria 1–3.
Major Differential Diagnoses
Rheumatoid Arthritis
Ankylosing spondylitis occurs more frequently in males, whereas rheumatoid arthritis predominantly affects females.
Sacroiliac joint involvement is universal in ankylosing spondylitis but is rare in rheumatoid arthritis.
Ankylosing spondylitis involves the entire spine in an ascending pattern from the lower segments, while rheumatoid arthritis is limited to the cervical spine.
Peripheral joint involvement in ankylosing spondylitis mainly affects the large joints of the lower extremities, whereas rheumatoid arthritis primarily affects the small joints of the hands.
The positivity rate for rheumatoid factor in rheumatoid arthritis is 70–80%, while ankylosing spondylitis is usually negative for rheumatoid factor.
Ankylosing spondylitis is predominantly associated with HLA-B27 positivity, while rheumatoid arthritis is usually negative for HLA-B27.
Osteitis Condensans Ilii
Most commonly seen in young women, it manifests as chronic low back pain and morning stiffness. Clinical examination typically reveals only lumbar muscular tension without other abnormalities.
Characteristic X-ray findings include marked sclerosis in the lower two-thirds of the iliac bone along the sacroiliac joint, without involvement of the sacroiliac joint surfaces or narrowing of the joint spaces.
The condition does not typically exhibit postural pain following prolonged sitting or lying, and the effectiveness of nonsteroidal anti-inflammatory drugs (NSAIDs) is less pronounced compared to ankylosing spondylitis.
Treatment
The primary goals of treatment are to relieve pain, prevent deformities, and improve function.
Non-Pharmacological Treatment
Patients are encouraged to gain a thorough understanding of the disease's characteristics and prognosis to improve their confidence in adhering to standardized treatment. Training and stretching exercises to maintain spinal and joint mobility are recommended, along with maintaining proper posture to reduce or delay the progression of kyphotic deformity. Smoking cessation is associated with better functional outcomes.
Pharmacological Treatment
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the first-line choice for symptom control. If two different NSAIDs fail to produce satisfactory results with continuous usage, disease-modifying anti-rheumatic drugs (DMARDs), including biological agents, should be considered.
Surgical Treatment
In cases of joint ankylosis, artificial joint replacement surgery can be performed. For severe kyphotic deformities that significantly impact daily living, spinal osteotomy and corrective surgeries may be considered.